![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
Name the bones of the skull.
|

Calvaria:
---Frontal bone, parietal bones, temporal bones, occiptal bone Base: ---sphenoid, palatine (occiptal, and temporal bones) Viscerocranium: ---maxilla, mandible, zygomatic bones, nasal bone, lacrimal bones, ethmoid bones, vomer, |
|
|
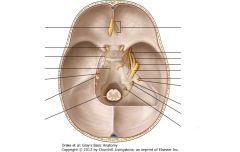
Identify the boundaries of the anterior cranial fossa and its foramen.
|
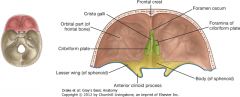
Boundaries:
---formed from parts of: ---frontal (anterior/lateral) ---ethmoid (midline): has crista galli and cribiform plate ---sphenoid bones (posterior) ---above the nasal cavity and orbits Foramen: ---Anterior/posterior ethmoidal foramen (foramen cecum): for anterior/posterior ethmoidal vessels and nerves ---Olfactory foramina in cribiform plate: for olfactory nerves (CN I) |
|
|
Identify the boundaries of the middle cranial fossa and its foramina.
|

Boundaries:
---anterior and middle fossa divided by the anterior edge of chiasmatic sulcus (smooth groove between optic canals in body of sphenoid; lesser wings of sphenoid create lateral boundaries ---formed by parts of: ---sphenoid (midline): sella turcica, indentation that contains pituitary gland ---temporal bones: forms posterior boundary near the pterion Foramina: ---superior orbital fissure: ---ophthalmic veins ---oculomotor nerve (CN III) ---trochlear nerve (CN IV) ---ophthalmic nerve (CN V1) ---abducens nerve (CN VI) ---optic canal: ---optic nerve (CN II) ---ophthalmic artery ---foramen rotunda ---maxillary nerve (CN V2) ---foramen ovale ---manibular nerve (CN V3) ---foramen spinosum ---middle meningeal vessels ---recurrent (meningeal) branch of mandibular nerve ---carotid canal ---internal carotid artery ---internal carotid venous plexus ---internal carotid nervous plexus (sympathetic) ---hiatus of facial canal ---greater petrosal nerve ---petrosal branch of middle meningeal artery |
|
|
Identify the boundaries of the posterior cranial fossa and its foramina.
|
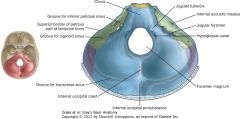
Boundaries:
---formed from parts of: ---temporal bones (lateral) ---occipital bone (posterior) ---small contributions from sphenoid and parietal bones ---contains the brainstem (midbrain, pons, medulla) and cerebellum Foramen: ---internal acoustic meatus ---internal auditory vessels ---facial nerve (CN VII) ---vestibulocochelar nerve (CN VIII) ---jugular foramen ---sigmoid sinus ---inferior petrosal sinus ---glossopharyngeal nerve (CN IX) ---vagus nerve (CN X) ---accessory nerve (CN XI) ---meningeal branches of occipital and ascending pharyngeal arteries ---hypoglossal canal ---hypoglossal nerve (CN XII) ---foramen magnum ---vertebral arteries ---accessory nerves (spinal contribution to CN XI) ---medulla oblongata and meninges ---anterior/posterior spinal arteries ---spinal cord |
|
|
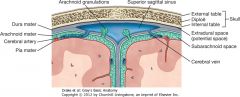
Describe the three layers of cranial meninges and its nerve supply.
|
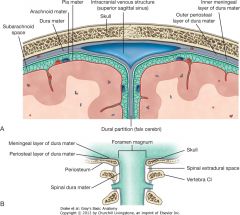
Dura mater:
---tough, outer layer, composed of two parts ---periosteal layer: (outer) firmly attached to skull (periosteum); contains meningeal arteries ---meningeal layer: (inner) close contact with arachnoid mater ---separations between the two layers create dural partitions (project inward and incompletely separate parts of the brain) and cranial venous sinuses ---dural partitions: falx cerebri (between two hemispheres); tentorium cerebelli (separates cerebellum); falx cerebelli; diaphragma sella (covers pituitary gland) Arachnoid mater: ---delicate middle layer; avascular; does not enter grooves of brain, except for longitudinal fissure between hemispheres Pia mater: ---inner layer firmly attached to surface of the brain; enters grooves and fissures, is closely applies to roots of cranial nerves Innervation: ---of dura mater: small meningeal branches of all three divisions of trigeminal nerve (CN V), vagus nerve (CN X) and first, second, sometimes third cervical nerves |
|

Identify which type of intracranial hemorrhage this is, its likely causes and its characteristics on CT imaging.
|
Epidural (extradural) hemorrhage:
---lies in potential space between bone and dura mater ---caused by arterial damage and results from tearing of branches of middle meningeal artery (in pterion); blood ---blood collects between periosteal layer of dura mater and calvaria, expanding under arterial pressure Causes: ---blow to the head (usually sports activity); produces minor loss of consciousness, with following lucid interval and subsequent unconsciuosness, which may lead to death |
|
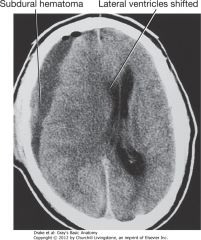
Identify this intracranial hemorrhage, its likely causes and characteristic CT imaging.
|
Subdural hemorrhage:
---occurs within the dural border cells layer, in the innermost lining of the meningeal dura (doesn't truly exist, only during trauma) ---results from venous bleeding, usually from torn cerebral veins where they enter the superior sagittal sinus Causes: ---most at risk are young and elderly, usually following trivial injury, with insidious loss of consciousness or alteration of personality |
|
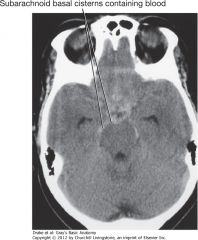
Identify the intracranial hemorrhage, its likely causes and characteristics of CT imaging.
|
Subarachnoid hemorrhage:
---deep to arachnoid mater before pia mater, filled with CSF ---typically results from ruptured intracerebral aneurysm arising from vessels supplying and around the arterial circle of Willis, but may occur in patients who have undergone significant cerebral trauma |
|
|
Identify the intracranial hemorrhage and its likely causes and characteristics of CT imaging.
|

Intraparenchymal hemorrhage:
---arterial bleeding from the intraparenchymal cerebral artery ---usually due to hemorrhage trauma ---CT scan shows hyperdensity within the substance of the brain |
|
|
Describe the circle of Willis, the contributing vessels and the distribution of its branches to the brain.
|
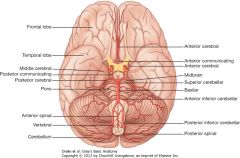
Major contributing vessels:
---Internal carotid: enters skull via carotid canal and proceeds superiorly along either side of the hypophyseal fossa ---Branches: 1. Middle cerebral artery*: supplies lateral aspect of frontal, parietal and superior temporal lobes (isn't actually part of Circle of Willis, just receives supply from the circle) 2. Anterior cerebral artery: supplies medial aspect of frontal and parietal lobes; deep internal structures and choroid plexus of lateral ventricles 3. Posterior communicating artery: anastomosing branch of arterial circle of Willis ---Vertebral/basilar arteries: enters skull through foramen magnum and run superiorly alongside the medulla; fuse together to form the basilar artery, which runs superiorly along the surface of the pons ---Branches: 1. Anterior spinal artery: supplies anterior 2/3 of spinal cord 2. Posterior inferior cerebral artery: supplies inferior surface of cerebellum and portion of brain stem 3. Anterior inferior cerebellar arterie: anterior portions of the inferior surface of cerebellum 4. Superior cerebellar artery: superior surface of cerebellum 5. Posterior cerebral artery: medial and inferior surfaces of occipital and temporal lobes and portions of midbrain and brain stem ---anterior communicating artery connects left/right anterior cerebral arteries Normally little to no blood flow around circle, but if one of the major vessels becomes occluded within/proximal to circle, communicating arteries allow anastomotic flow to prevent neurological damage |
|
|
Describe the dural venous sinuses and the pattern of their blood flow.
|
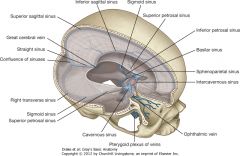
Dural venous sinuses:
---endothelial-lined spaces between the outer periosteal and inner meningeal layers of dura mater, leading to internal jugular veins Venous drainage: ---starts internally as networks of small venous channels that lead to larger cerebral veins, cerebellar veins and veins from the brainstem, all draining into the venous sinuses; also have diploic and emissary veins draining in Sinuses: ---superior sagittal sinus: in superior border of falx cerebri; begins at foramen cecum and ends in the confluence of sinuses (right transverse sinus); communicates with lateral extensions of the sinus containing arachniod granulations ---inferior sagittal sinus/straight sinus: in inferior margin of falx cerebri; receives few cerebral veins and ends at anterior edge of tentorium cerebelli; is joined by great cerebral vein and forms straight sinus - continues along junction and ends in confluence of sinuses (left transverse sinus) ---confluence of sinuses, transverse and sigmoid sinuses: superior sagittal/straight sinuses and occipital sinus (in falx cerebri) empty into confluence of sinuses; drained by left/right transverse sinuses - extend in tentorium cerebelli and as leave surface of occipital, become sigmoid sinuses to end at internal jugular veins ---cavernous sinuses: paired, against lateral aspect of sphenoid body; receive blood from cerebral veins, ophthalmic veins and emissary veins (pterygoid plexus); connected by intercaverous sinuses ---passing through: internal carotid artery and abducens nerve (CN VI) ---passing laterally (sup>inf): oculomotor nerve (III), trochlear nerve (IV), ophthalmic nerve (V1), maxillary nerve (V2) ---vulnerable to injury by inflammation; infections can pass extracranial to intracranial through sinus ---superior/inferior petrosal sinuses: drain cavernous sinuses into transverse sinuses ---basilar sinuses: connect inferior petrosal sinuses to each other and to vertebral plexus of veins |
|
|
Where is cerebrospinal fluid formed, how does it circulate around the brain and where does it drain?
|
Formation:
---produced by choroid plexus, primarily in the ventricles of the brain Circulation: ---circulates through the subarachnoid space around brain/spinal cord Drainage: ---returns to venous system through arachnoid villi, which project as clumps (arachnoid granulations) into the superior sagittal sinus and its lateral extensions (lateral lacunae) |
|
|
Describe the location of the parotid gland, its sensory and autonomic innervation and the route of its secretions from gland to mouth.
|
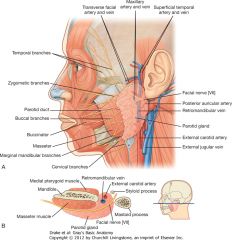
Location:
---largest of main salivary glands, anterior to and below the lower half of the ear, stretching between the lower border of the mandible to the zygomatic arch Innervation: ---sensory: ---auriculotemporal nerve: branch of mandibular nerve (V3) - existed skull through foramen ovale ---autonomic: ---auriculotemporal nerve carries secretomotor fibers (postganglionic parasympathetic) to gland - originate in otic ganglion associated with mandibular nerve (V3) ---preganglionic parasympathetic fibers to otic ganglion come from glossopharyngeal nerve (IX) Pathway: ---parotid duct leaves the anterior edge of gland midway between zygomatic arch and corner of mouth; crosses the face in transverse direction, over the masseter muscle and turns deeply into buccal fat pad to pierce buccinator muscle; opens into oral cavity near second upper molar |
|
|
Describe the olfactory nerve, the types of nerve fibers it carries and the foramen it passes through.
|
Cranial nerve I: for sense of smell
---carries special afferent fibers ---sensory neurons have peripheral processes that act as olfactory receptors in the nasal mucosa and central processes to transmit info to the brain ---central processes terminate by synapsing with secondary neurons in the olfactory bulbs ---Exit through the cribiform plate plate of ethmoid bone |
|
|
Describe the optic nerve, the nerve fibers it carries and the foramen through which it exits the skull.
|
Cranial nerve II: vision
---carries special afferent ---fibers return info to the brain from photoreceptors in the retina ---Exit skull from optic canal |
|
|
Describe the oculomotor nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve III:
---General somatic efferent: innervate most of extra-ocular muscles (levator palpebrae superioris, superior rectus, inferior rectus, medial rectus and inferior oblique) ---General visceral efferent: parasympathetic - innervates sphincter pupillae for pupillary constriction; ciliary muscles for accommodation of the lens for near vision ---Exits skull through superior orbital fissure |
|
|
Describe the trochlear nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve IV:
---General somatic afferent: innervates superior oblique muscle ---exits skull through superior orbital fissure |
|
|
Describe the trigeminal nerve, its nerve fibers and the foramina through which it exits the skull.
|
Cranial nerve V: major sensory nerve of head, muscles of lower jaw
---General somatic afferent: three divisions 1. ophthalmic (V1): eyes, conjunctiva, orbital contents, nasal cavity, frontal sinus, ethmoidal cells, upper eyelid, dorsum of nose, anterior part of scalp, dura in anterior cranial fossa, superior part of tentorium cerebelli 2. maxillary (V2): dura in middle cranial fossa, nasopharynx, palate, nasal cavity, upper teeth, maxillary sinus, skin covering side of nose, lower eyelid, cheek, upper lip 3. mandibular (V3): skin of lower face, cheek, lower lip, anterior part of external ear, part of external acoustic meatus, temporal fossa, anterior 2/3 of tongue, lower teeth, mastoid air cells, mucous membranes of cheek, mandible, dura in middle cranial fossa ---branchial efferent: innervates temporalis, massetter, medial/lateral pterygoids, tensor tympani, tensor veli palatini, anterior belly of digastric and mylohyoid muscles Exits: ---V1: superior orbital fissure ---V2: foramen rotundum ---V3: foramen ovale |
|
|
Describe the abducent nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve VI:
---general somatic efferents: innervate lateral rectus muscle (orbit) Exit: superior orbital fissure |
|
|
Describe the facial nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve VII:
---General somatic afferent: sensory from part of external acoustic meatus and deep parts of auricle ---special afferent: taste from anterior 2/3 of tongue ---General visceral efferent: innervates lacrimal gland, submandibular and sublingual salivary glands and mucous membranes of nasal cavity, hard/soft palates ---branchial efferent: innervates muscles of face (facial expression) and scalp (derived from second pharyngeal arch), stapedius, posterior belly of digastric, stylohyoid muslces Exit: ---stylomastoid foramen: leaves cranial cavity through internal acoustic meatus, branches in facial canal of temporal bone before exiting foramen |
|
|
Describe the vestibulocochlear nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve VIII:
---special afferent: two divisions 1. vestibular: for balance 2. cochlear: for hearing Exit: ---through internal acoustic meatus |
|
|
Describe the glossopharyngeal nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve IX:
---general visceral afferent: sensory from carotid body and sinus ---special afferent: taste from posterior 1/3 of tongue ---general somatic afferent: posterior 1/3 of tongue, palatine tonsils, oropharynx, mucosa of middle ear, pharyngotympanic tube, and mastoid air cells ---general visceral efferent: parasympathetic - innervates parotid salivary gland ---branchial efferent: innervates stylopharyngeus muscle Exit: through jugular foramen |
|
|
Describe the vagus nerve, its nerve fibers and the foramen through which its exits the skull.
|
Cranial nerve X:
---general somatic afferent: larynx, laryngopharynx, deeper parts of auricle, part of external acoustic meatus and dura in posterior cranial fossa ---general visceral afferent: aortic body chemoreceptors and aortic arch baroreceptors, esophagus, bronchi, lungs, heart and abdominal viscera of foregut/midgut ---special afferent: taste from epiglottis and pharynx ---general visceral efferent: parasympathetic - innervates smooth muscle and glands of pharynx, larynx, thoracic viscera and abdominal viscera of foregut/midgut ---branchial efferent: innervates one tongue muscle (palatoglossus), muscles of soft palate (except tensor veli palatini), pharynx (except stylopharyngeus) and larynx Exit: ---jugular foramen |
|
|
Describe the accessory nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve XI:
---general somatic efferent: innervates sternocleidomastoid and trapezius muscles Exit: ---jugular foramen |
|
|
Describe the hypoglossal nerve, its nerve fibers and the foramen through which it exits the skull.
|
Cranial nerve XII:
---general somatic efferent: innervates hypoglossus, genioglossus and styloglossus muscles and all intrinsic muscles of tongue Exit: ---hypoglossal canal |
|
Identify the nerves and the foramen through which they exit the skull.
|
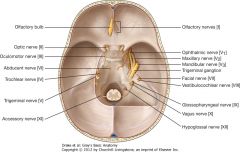
Olfactory (I): cribiform plate
Optic (II): optic canal Oculomotor (III): superior orbital fissure Trochlear (IV): superior orbital fissure Trigeminal (V): ---ophthalmic (V1): superior orbital fissure ---maxillary (V2): foramen rotundum ---mandibular (V3): foramen ovale Abducent (VI): superior orbital fissure Facial (VII): stylomastoid foramen (internal acoustic meatus) Vestibulocochlear (VIII): internal acoustic meatus Glossopharyngeal (IX): jugular foramen Vagus (X): jugular foramen Accessory (XI): jugular foramen Hypoglossal (XII): hypoglossal canal |
|
|
Describe the course of the facial nerve in the head and superficial face, its relationship to the parotid gland and the functions of its major branches.
|
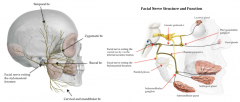
Course:
---leaves cranial cavity through internal acoustic meatus, enlarges as the geniculate ganglion in facial canal of petrous part of temporal bone, gives off branches ---exits the skull through stylomastoid foramen, then passes into the parotid gland Parotid relationship: ---passes through, branches into upper/lower trunks with 5 terminal branches (parotid plexus) 1. temporal: supply muscles in area of temple, forehead and supra-orbital region 2. zygomatic: supply muscles in area of infraorbital region, lateral nasal area and upper lip 3. buccal: supply muscle in cheek, upper lip and corner of mouth 4. cervical: supply platysma muscle 5. marginal mandibular: supply muscles of lower lip and chin Additional branches: ---greater petrosal nerve: preganglionic parasympathetic synapse in pterygopalatine ganglion (general visceral efferent) - postganglionic innervate: lacrimal gland, mucous glands of nasal cavity, maxillary sinus, palate ---chorda tympani: ---carries taste (special afferent) - anterior 2/3 tongue ---preganglionic parasympathetic synapse in submandibular ganglion (general visceral efferent) - postganglionic innervation of submandibular/sublingual glands ---motor to stapedius ---sensory nerve branches: auricle of ear, auditory canal and external surface of tympanic membrane |
|
|
Describe the sensory innervation of the face and the pathway the nerves take to reach their target areas.
|
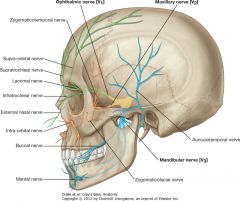
Trigeminal nerve (V):
---most cutaneous innervation is by the three branches, but area of angle/lower border of mandible and parts of ear are innervated by: trigeminal, facial, vagus and cervical nerves Ophthalmic (V1): exits superior orbital fissure and branches - ---supra-orbital and supretrochlear: leave orbit superiorly, innervate upper eyelid, forehead and scalp ---infratrochlear: extis orbit in medial angle, innervates medial half of upper eyelid, skin of middle angle and side of nose ---lacrimal: exits orbit in lateral angle, innervates lateral half of upper eyelid and skin of lateral angle ---external nasal: supplies anterior part of nose Maxillary (V2): exits foramen rotundum and branches - ---zygomaticotemporal: exits zygomatic bone, supplies anterior temple above arch ---zygomaticofacial: exits zygomatic, supplies area over bone ---infra-orbital: exits maxilla, divides into branches to supply lower eyelid, cheek, side of nose and upper lip Mandibular (V3): exits foramen ovale and branches - ---auriculotemporal: enters posterior to temporomandibular joint, supplies external acoustic meatus, surface of tympanic membrane and temple ---buccal: on surface of buccinator muscle, supplies cheek ---mental: exits mental foramen, divides and supplies skin and mucous membrane of lower lip and chin |
|
|
Describe the origin and distribution of the major arterial supply of the superficial face.
|
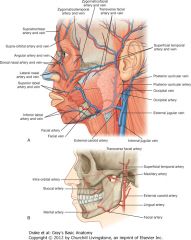
Arterial: primarily from branches of external carotid artery, limited internal carotid artery
Facial artery: ---major artery supplying face, anterior branch of external carotid; passes along mandible, runs up along side of nose and terminates in medial corner of eye as angular artery ---branches: inferior/superior labial branches supply lower/upper lip and nasal septum, anastomose with companion arteries on other side of face; lateral nasal branch supplies lateral/dorsum of nose Transverse facial artery: ---branch of superior temporal artery (from external carotid); crosses face transversely, between zygomatic arch and parotid duct Maxillary artery: ---terminal branch of external carotid ---branches: infra-orbital artery supplies lower eyelid, upper lip and area between; buccal artery supplies area around buccinator; mentar artery supplies chin Ophthalmic artery: ---branch of internal carotid ---branches: zygomaticofacial/zygomaticotemporal arteries supply area over zygomatic; dorsal nasal artery supplies dorsum of nose; other branches supply anterior scalp |
|
|
Describe the origin and distribution of major venous supply of the superficial face.
|
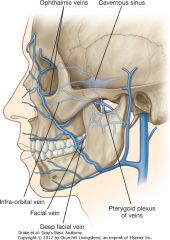
Venous: most return is back to the internal jugular vein, with some important connections with cavernous sinus
Facial vein: major vein draining face ---originates in medial corner of orbit, follows artery posteriorly, then drains into internal jugular Transverse facial vein: ---small, accompanies artery, drains into superficial temporal vein in parotid gland Intracranial venous collections: ---facial vein has connections with venous channels ---ophthalmic veins in medial corner of orbit ---veins passing into infra-orbital foramen in cheek ---deep facial vein/pterygoid plexus of veins ---all connect to cavernous sinus through emissary veins (no valves, so blood can move in any direction - danger zone - easy to pass infection) |
|
|
Describe the structure and organization of the conjuctiva of the eye.
|
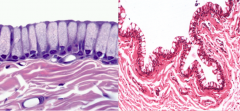
Composed of two layers which cover inner eyelids and exposed sclera:
---palpebral: located on posterior eyelids ---bulbar: located on sclera, blends with cornea Structure: ---stratified columnar epithelium, with numerous goblet cells in the superficial layer and melanocytes in the basal layer ---well-vascularized lamina propria ---at junction with cornea, becomes squamous and continuous with corneal epithelium |
|
|
Describe the structure and organization of the cornea.
|
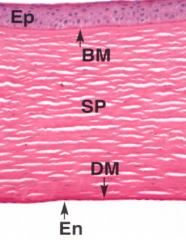
Forms anterior 1/6 of fibrous tunic; 5-layers
---epithelium (EP): stratified squamous, 5-7 layers; turnover every 7 days ---basement membrane (BM): anterior basement membrane ---stroma/substantia propria (SP): fibroblasts, layers of type I and V collagen forming lamellae and arranged in regular lattice ---DM: posterior basement membrane ---endothelium (EN): simple squamous, important in fluid control ---Transparent: due to fiber arrangement and lack of vessels ---Avascular: easily transplanted, no immune cells ---Sensitive: afferents in CN V1, run in stroma |
|
|
Describe the structure and organization of the sclera.
|

Forms white 5/6 of fibrous tunic; 3 layers: deep side in contact with choroid, superficial side in contact with muscle attachments
---outer: episclera - loose connective tissue ---middle: substantia propria (tenon's capsule) - dense collagen ---inner: suprachoroid lamina - thin collagen, elastic ---composition is similar to cornea, but the arrangement of the fibers is more irregular, so not transparent; also vascularized |
|
|
Describe the structure and organization of the choroid of the eye.
|
Posterior portion of the vascular tunic; deep portion in contact with retina, superficial portion in contact with sclera; 3 layers:
---outer: stromal - large vessels, collagen/elastic, melanocytes ---middle: choriocapillary - small vessels serving retina ---inner: Bruch's membrane - collagen/elastic, basal lamina |
|
|
Describe the structure and organization of the ciliary body.
|
Middle part of vascular tunice; composed of ciliary processes and ciliary muscle
---processes: bi-layered cuboidal, with heavily pigmented deep layer and well vascularized stroma ---produces aqueous humor, secretes it into the posterior chamber of the anterior cavity ---ciliary muscles: attach to lens via suspensory ligaments and change the shape of lens for focus; when muscles contracts, ligaments relax (innervated by CN III) |
|
|
Describe the iris and pupil and importance of the canal of Schlemm.
|
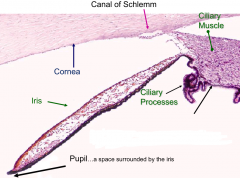
Parts of vascular tunic:
Iris: loose connective tissue with melanocytes (dense posteriorly); contains dilator pupillae muscle along the posterior side and sphincter pupillae muscle near the pupillary margin ---pupil: space surrounded by the iris Canal of Schlemm (sclera venous sinus): drains aqueous humor and spiscleral veins |
|
|
Describe how the muscles of the iris function and their innervations.
|

Dilator pupillae muscle: myoepthelium, forms striations
---sympathetic stimulation cause radial muscles to contract and dilate the pupil Sphincter (constrictor) pupillae muscle: smooth muscle fibers, circles pupil ---parasympathetic (oculomotor CN III) stimulation causes circular muscles to contract, constricting the pupil |
|
|
Describe the structure and organization of the lens of the eye.
|
Anterior epithelium: simple cuboidal
---no posterior epithelium; has outer capsule, which is basement membrane-like ---transparent Lens substance: fibers, consists of elongated anuclear epithelial cells which are produced throughout life ---avascular ---hexagonal Shape change: accomodated by tension on the zonular ligaments by ciliary muscles, changing focal length of light rays allowing discrimination of near/far objects |
|
|
Describe the difference between myopia and hyperopia and how they can be corrected.
|

Myopia: near-sightedness
---length of eye is larger than usual, so ray doesn't reach the focal point, distorting far distances ---can be corrected by concave lens in front Hyperopia: far-sightedness ---length of eye is shorter than usual, putting the ray past the focal point, distorting near objects ---can be corrected by concave lens in front |
|
|
Describe the structure and organization of the retina.
|

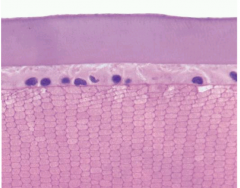
Part of nervous tunic:
---(P) pigmented layer: next to choroid, simple cuboidal epithelium ---phagocytosis of discs of rods/cones ---produces melanin - acts as absorptive, anti-reflection mechanism ---tight junctions create blood-retinal barrier: regulates movement between sensory neurons and choroid, maintains ionic environment and prevents leucocytes from entering retina ---(PR) photoreceptor nuclei: contains rod and cones ---(I) integrating nuclei: bipolar, amacrine, horizontal ---(G) ganglion cell nuclei: carry signal to brain via optic tract |
|
|
Describe the difference between rods and cones.
|
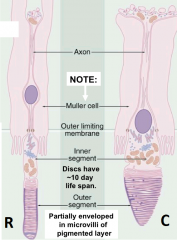
Rods: ~120 million, very sensitive and operate in low light; process visual information in black/white; less acute
---many rods converge on single ganglion cell Cones: ~6-7 million, less sensitive, process visual information in color; blue, red and green cones correspond to different wave lengths of light; more acute ---few to one cone per ganglion cell |
|
|
Describe the structure and function of the fovea centralis.
|
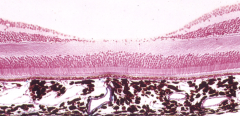
Specialized area of the retina: lies on temporal side of optic disc; area of greatest visual acuity
---has all cones, lacks integrating layer of cell bodies ---one-to-one ration of photoreceptors to cell bodies ---no retinal vessels, dependent on choroid Surrounding by macula lutea, where all the layers of the retina are present; help protect fovea from damaging short-wavelength light |
|
|
Describe the structure and organization of the optic disc.
|
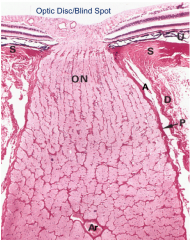
Blind spot in the retina, devoid of photoreceptors, where the optic nerve leaves the retina
Layers: ---S: sclera - disc blends into sclera ---D: dura mater ---A: arachnoid mater with CSF in subarachnoid space ---P: pia mater ---ON: optic nerve tract ---AR: central artery of retina |
|
|
Identify and describe an optic disc papilledema.
|
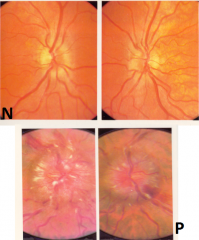
Papilledema: endocranial pressure forces CSF against disc, which causes a nipple-like swelling
|
|
|
Describe the circulation of aqueous humor.
|
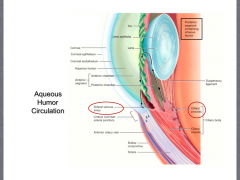
Produced in ciliary process, secreted into posterior chamber of the anterior cavity, passes through pupil into the anterior chamber and is eventually drained by the scleral venous sinus (canal of schlemm)
|
|
|
What are cataracts?
|
Clouding of the lens
|
|
|
Describe the organization of the ear.
|
Outer ear and middle ear are involved with collection, conduction and amplification of sound waves; inner ear contains organs which transduce these waves into afferent action potential as well as organs concerned with sense of equilibrium, balance and acceleration
---Outer: has auricle/pinna to collect sound waves which are passed to the external acoustic meatus ---Middle: passes through tympanic membrane to reach ossicle (malleus, incus and stapes) which lie within the epitympanic recess above bones and tympanic cavity below (lined with mucous membrane); surrounded by mastoid air cells in bone; has pharyngeotympanic (eustachian) tube the extends out the bottom to maintain pressure ---Inner: lies within petrous temporal bone; contains cochlea, vestibule and semicircle canals |
|
|
Describe the tympanic membrane.
|
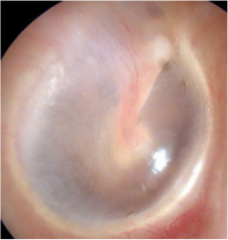
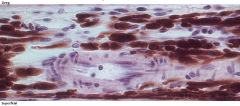
It is tri-layered:
---external: very thin skin, with epidermis of ~10 cells thick and very narrow dermis ---middle: fibrous with radiating fibers externally and circumferential fibers deep ---internal: simple squamous to squat cuboidal mucous membrane (lines middle ear) generally repairs easily |
|
|
Describe the function of the ossicles.
|
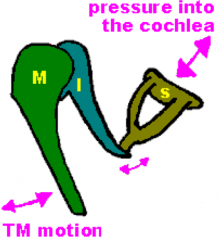
Sound waves caught by pinna travel along external meatus to tympanic membrane, where they physically displace the membrane and push in malleus, which pushes the incus, which pushes the stapes
---stapes pushes against connective tissue covered opening to inner ear (oval window); this displaces perilymph in inner ear ---because surface area of membrane is 17-20 times that of oval window, force of sound wave is significantly increased |
|
|
Describe the function of the stapedius and tensor tympani muscles.
|
When physical force created by loud noises is transduced, it can damage the delicate inner ear; muscles attached to ossicle decrease the force but can take about 25 milliseconds to contract to dampen sound wave, which is sometimes too slow
---stapedius: attaches to stapes, innervated by CN VII ---tensor tympani: attaches to malleus, innervated by V3 |
|
|
Describe the inner ear.
|
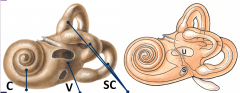
Bony labyrinth: cavern inside bone
Membranous labyrinth: soft tissue suspended inside bone, surrounded by fluid (perilymph) and filled with endolymph Cochlea: 2 1/2 coils, for hearing Vestibule: middle portion with saccule and utricle, for acceleration and position Semicircle canals: for equilibrium and position Boney core: modiolus Boney extensions: spiral lamina |
|
|
Describe the components of the cochlea and how it is affected by sound waves.
|
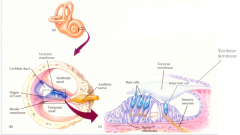
---Scala vestibuli: outer layer filled with perilymph; force of stapes pushing on oval window creates waves in perilymph as it travels along canal
---cochlear duct: filled with endolymph; displaced by waves (bounce) of perilymph; is tonotopic - each part is sensitive to particular frequency (tone); high notes proximal, low notes distal; organ of Corti - inside duct - transduces perilymph wave ---frequency determines where waves bounce ---amplitude determines force of bounce ---vestibular membrane: separates the scala vestibuli (vestibular canal) from the cochlear duct; fine, fibrous and epithelial lined ---basilar membrane: separates cochlear duct from scala tympani (tympanic membrane); thicker Effect of sound waves: ---bounce of perilymph displaces vestibular membrane inferiorly > displaces endolymph > forces basilar membrane inferiorly > organ of Corti transduces the physical energy into an action potential > eventually becomes sound |
|
|
Describe transduction in the ear.
|
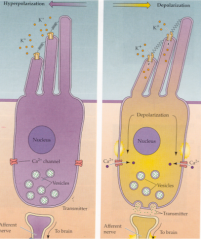
Takes place in specialized, polar epithelial cells with stereocilia and kinocilia (in vestibule/semicircle canals) - hair cells
---is mechanotransduction; physical energy moves hairs (in direction of longest cilia) to physically open cation gates, causing depolarization of cells ---opens calcium gates at opposite pole of cell and causes the release of neurotransmitter ---causes depolarization of dendritic end of bipolar vestibulocochlear nerves |
|
|
Describe the different hair cells.
|
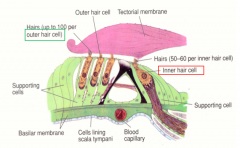
Inner: one row, ~10,000 of them, are cells we "hear" with; stereocilia are in contact with gelatinous tectorial membrane - physically bent to open cation channels
Outer: three rows, ~30,000 of them, not directly involved with hearing transduction but enhance frequency discrimination |
|
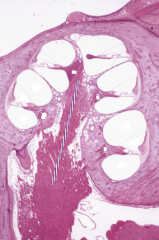
Identify the different components.
|

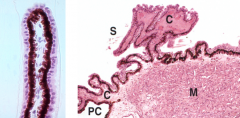
SV: scala vestibuli
SM: scala media (cochlear duct) ST: scala tympani G: ganglia ------ modiolus (spongy bone with ganglion) |
|
Identify the different components of the cochlea.
|
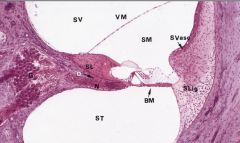
VM: vestibular membrane
BM: basilar membrane O: osseous spiral lamina (part of modiolus) G: spiral ganglion SL: spiral ligament SVasc: stria vascularis (site of endolymph formation SV: scala vestibuli SM: scala media (cochlear duct) ST: scala tympani |
|

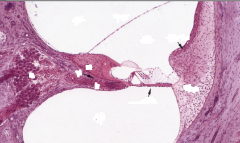
Identify the components of the cochlea.
|

TM: tectorial membrane
SM: scala media (cochlear duct) OSC: outer sensory (hair) cells ISC: inner sensory (hair) cells SL: spiral ligaments ***neurons are bipolar*** |
|
|
Describe the vestibule.
|

Composed of saccule and utricle
---fibrous sacs filled with endolymph, attached to periosteum ---each has specialized region (macula) ---sense movement of head, effects of gravity and acceleration Has columnar hear cells embedded in gelatinous avascular matrix (otolithic membrane) ---density of membrane is increased by small pieces of calcium carbonate (otoliths) |
|
|
Describe the semi-circular canals.
|
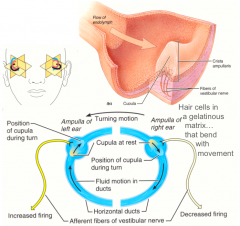
Filled with endolymph, three canals oriented in three planes
---each has dilated ampulla with sensory mechanism (crista ampullaris); sense rotational movements and head/body |

