![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
What is type 1 hypersensitivity? |
an immediate type hypersensitivity (exaggerated or inappropriate immune response) IgE - mediated Hypersensitivity |
|
|
What happens with IgE in Type 1 hypersensitivity? |
Antigen (Ag) induces crosslinking of IgE bound to mast cells and basophils - with release of vasoactive mediators. |
|
|
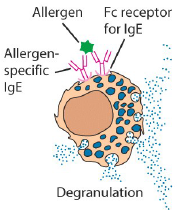
Cell is mast cell or basophils. This is Type 1 hypersensitivity |
|
|
How are antigens delivered to IgE? |
Delivered through mucous membranes (intestine, lung) or skin. |
|
|
What do animals make IgE against usually? |
For parasites! |
|
|
What does anaphylactic mean? |
Acute allergic reaction to antigen to which the body has become hypersensitive. |
|
|
The type 1 hypersensitivity reaction basic? |
First exposure to allergen Antigen activation of TH2 cell and stimulation of IgE class switching in B cells. Produce IgE Binding of IgE to FcE R1 on mast cells. NOW A REPEATED EXPOSURE Ag cross links onto Fc receptors with IgE on mast cells = degranulation |
|
|
What happens after degranulation? |
1 Vasoactive amines, lipid mediators = immediate hypersensitivity. (Leukocyte recruitment, particularly eosinophils)
2. Cytokines = late phase reaction. (2-4 hours after) |
|
|
What is FcE receptor? |
A receptor on mast cells and basophils which bind to the Fc portion of the IgE. |
|
|
How do you get TH2 cells (T helper cells) |
Naive T cells must encounter antigen in presence of IL-4 |
|
|
What do the TH2 cells do? |
They interact with antigen specific B cells - switching antibody isotype to IgE by secreting IL-4 and expressing CD40L |
|
|
What is released from the mast cells/basophils via granule exocytosis? |
Vasoactive amines = vascular dilatation, smooth muscle contraction. Proteases = Tissue damage |
|
|
What is released by mast cells / basophils via secretion? |
Prostaglandins, leukotrienes, Cytokines. (TNF) (tumor necrosis factor) |
|
|
What are the two main anaphylotoxins called? And what do they do? |
C3a and C5a incr. vascular permeability attract phagocytes - neutrophils in particular! so local leakiness |
|
|
Activated mast cell (or basophil) releases what that do what? |
Biogenic amine (histamine) - vascular leak) Lipid mediators (PAF, PGD2, LTC4) = broncho-constriction and intestinal hypermotility Cytokines (TNF) - inflammation Lipid mediators also do inflammation Enzymes (tryptase) = tissue dmg |
|
|
Mast cell acts in different ways at different sites? GI tract? Airways? Blood vessels? |
Gi = incr. fluid secretion, incr. peristalsis Airways - decr. diameter - incr. mucus Blood vessels - incr blood flow, incr perm |
|
|
mast cells at "" consequences GI Airways Blood vessels |
Gi - expulsion. diarrhoea, vomiting Airways - congestion "wheezing, coughing, phlegm. swelling and mucus secretion in nasal passages Blood vessels - incr. fluid i ntissues. incr. cells and protein in tissues. Increased effector response in tissues |
|
|
Why animals respond differently to similar antigens? |
atopic individuals may have more circulating IgE and higher eosinophil levels than normal counterparts. May be more efficient at switching on genes encoding for IgE (Il-4 & IL-5 and GMCSF) also may be linked to MHC2 alleles which may favor a strong TH2 response. |
|
|
how to stop IgE response. |
Administer small amounts of antigen to try and shift the response from IgE to IgG. |

