![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
Simple Squamous Epithelium
|
|
|
Stratified Squamous
|
|
|
Simple Cubodial
|
|
|
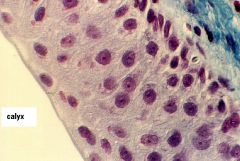
Stratified Cubodial
|
|
|
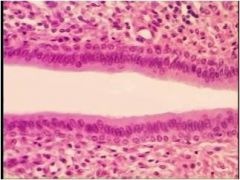
Simple Columnar
|
|
|
Stratified Columnar
|
|
|
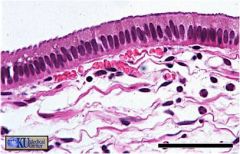
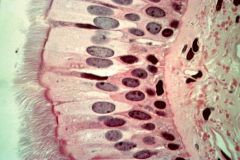
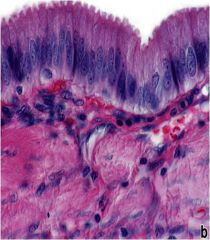
Ciliated Pseudostratified Columnar
|
|
|
Transitional epithelium
|
|
|
secretory product is released in apical portion of cell surrounded by a thin layer of cytoplasm and plasma membrane
|
Aprocrine gland
|
|
|
secretory product accumulates within maturing cell, and is released into lumen of the gland when the cell undergoes apotosis.
|
holocrine gland
|
|
|
layer of variable thickness next to the basal surface
|
basement membrane
|
|
|
anchors the cell to extracellular matrix
|
Cell-to-extracellular matrix junctions
|
|
|
increase surface area & facilitates morphologic interations between adjacent cells
|
Plasma membrane inflodings
|
|
|
Ectoderm derivatives
|
- Epidermis
- Cornea & Lens Enamel Components of Inner Ear Anterior Lobe of Pituitary |
|
|
Mesodermal derivatives
|
Epithelium of Kidney & Gonads
Mesothelium (epithelium lining the pericardial, pleural, and peritoneal cavites) Endothelium (epithelium lining the cardiovascular and lymphatic vessels) Adrenal Cortex Seminiferous & Genital duct epithelium |
|
|
Endodermal derivatives
|
Respiratory System Epithelium
Alimentary Canal Epithelium Extramural Digestive Gland Epithelium Epithelium of tympanic cavity & auditory tubes |
|
|
Types of anchoring junctions
|
zona adherens and macula adherens
|
|
|
Communicating junctions
|
Direct communication by diffusion of small molecules (gap junctions)
|
|
|
Occluding junctions
|
Impermeable (tight junctions)
|
|
|
specialized site that joins epithelial cells & acts as a barrier to the diffusion of substances
|
Junctional Complex
|
|
|
Long, immotile microvilli
Most found in organ of corti |
stereocilia
|
|
|
Domain with special Structural Surface Modifications
|
Apical Domain
|
|
|
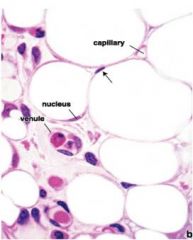
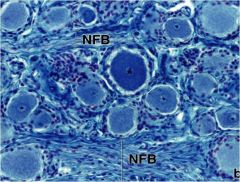
White Adipose Tissue
|
|
|
How would you characterize adipose tissue structure?
|
Isolated adipocytes are spherical but appear polyhedral or oval in the tissue
|
|
|
Functions of white adipose tissue
|
Storage of excess carbohydrates and triglycerides
Insulation Cushioning of internal organs Synthesis and production of leptin |
|
|
What does adipose tissue originate from and how does it develop?
|
Derived from mesoderm mesenchyme
Mesenchymal cells differentiate into lipoblasts and form lipid droplets in cytoplasm |
|
|
What regulates white adipose tissue?
|
Leptin gene controls amount of leptin produced by mature adipocytes
|
|
|
What is metabolism in terms of adipose tissue regulation?
|
Break down of triglycerides so they can be transported in the bloodstream
|
|
|
What is disposition in terms of adipose tissue regulation?
|
Uptake of glycerol and fatty acids to form triglycerides for storage
|
|
|
What protein causes the brown adipose tissue to be brown?
|
Cytochrome oxidase from mitochondria
|
|
|
What is the function of brown adipose tissue?
|
Thermogenesis,
|
|
|
Where in adults is brown adipose tissue found?
|
Adrenal glands
Aorta Neck |
|
|
Explain the pathophysiology of cellulite
|
Adipose cell chambers swollen --> Restriction of circulation --> Reduces oxygen supply --> decreased metabolism --> trapped water and solutes as a result of softer connective tissue bands --> pinching tiny nerve fibers --> pain
|
|
|
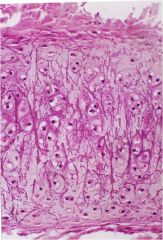
What is hyaline cartilage made up of?
|
Type II cartilage fibers, proteoglycans, hyaluronic acid
|
|
|
What is elastic cartilage made up of?
|
Type II cartilage fibers, proteoglycans, hyaluronic acid, elastic fibers, and elastic lamellae
|
|
|
What is fibrocartilage made up of?
|
Type I & II cartilage fibers, proteoglycans, and hyaluronic acid
|
|
|
What does the matrix of hyaline cartilage consist of?
|
Collagen, proteoglycans, glycoproteins, and noncollagenous proteins
Contains chondrocytes |
|
|
Function of hyaline cartilage
|
Reducing friction
Lubricating joints Distributing forces applied to bone |
|
|
Type II collagen
|
Forms the bulk of the fibril
|
|
|
Type X collagen
|
organized collagen fibrils into 3-D Lattice
|
|
|
Type IX collagen
|
facilitates fibril size and interacts with the matrix proteoglycans
|
|
|
Type XI collagen
|
Regulates fibril size
|
|
|
Type V collagen
|
Located in the periphery of the chondrocyte, it attaches the collagen types to the framework
|
|
|
3 glycosaminoglycans present in proteoglycans
|
Hyaluronic acid, chondroitin sulfate, keratan sulfate
|
|
|
Noncollagenous proteins
|
Regulatory and structural proteins that influence the interactions between chondrocytes and the matrix
|
|
|
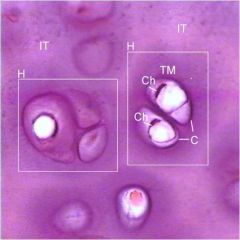
Hyaline cartilage
isogenous groups interterritorial matrix |
|
|
Elastic Cartilage
|
|
|
Dense connective tissue that surrounds most hyaline cartilage
|
Perichondrium
|
|
|
Where is hyaline cartilage present?
|
Trachea, larynx, bronchi, nose, e
|
|
|
Where is elastic cartilage present?
|
External ears, walls of external acoustic meatus, Eustachian tube, epiglottis
|
|
|
Appositional growth for cartilage
|
Forms new cartilage at the surface of existing cartilage (near perichondrium) via chondroblasts.
|
|
|
Interstitial growth for cartilage
|
Division of chondrocytes within lacunae
|
|
|
Why can't cartilage heal itself when it is damaged?
|
No blood vessels, No mobility for chondrocytes, and limited proliferativity for mature chondrocytes
|
|
|
Pathophys of Osteoarthritis
|
Thinning of cartilage --> bones rub together --> loss of movement of joints
aging, obese, previous injured patients effected |
|
|
DDH - developmental dysplasia of the hip pathophysiology
|
Hip joint not formed properly
Allows femoral head to slip in & out of pocket |
|
|
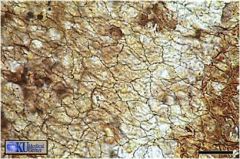
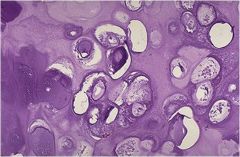
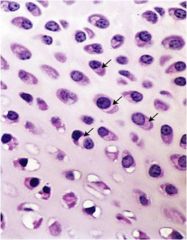
Chondrosarcoma
|
pleomorphic condrocytes piled together in a haphazard arrangement
|
|
|
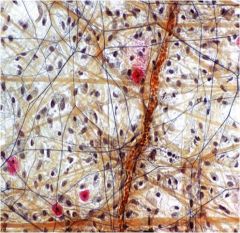
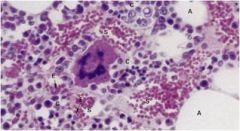
Chondrosarcoma
|
|
|
Loose connective tissue
|
|
|
Simple Columnar
|
|
|
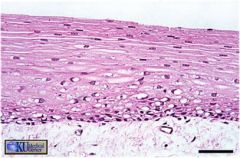
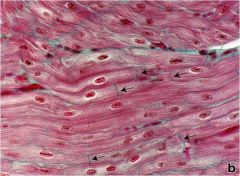
Dense connective tissue (Collagen)
|
|
|
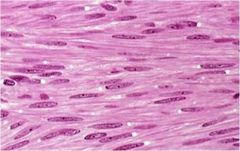
Cardiac muscle tissue
|
|
|
Nervous tissue
|
|

|
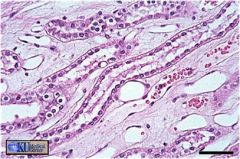
Bone
|
|
|
Red Bone Marrow
|
|

|
Yellow Bone Marrow
|
|
|
What does yellow bone marrow contain?
|
Fat, connective tissue, some white blood cells
|
|
|
What occurs during endochronal ossification
|
Perichondrial cells --> osteoblasts (periosteum cells)
Bone cuff is formed Chondrocytes become hypertrophic and cease production of collagen and secrete alkaline phosphatase (for mineral deposition) Matrix is calcified. Periosteal bud invades cavity left by chondrocytes Blood vessels invade proximal epiphyseal cartilage |
|
|
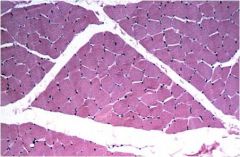
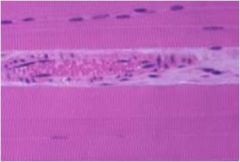
perimysium
|
|
|
Smooth muscle tissue
|
|
|
Blood vessel
|
|
|
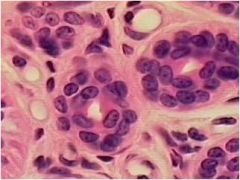
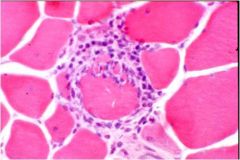
Muscle fiber attacked by lymphocytes
|
|
|
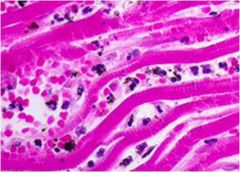
Necrotic cardiac tissue with a hemorrhage in the interstitum
|
|
|
these cells are derived from mesenchymal stem cells and give rise to osteoblasts.
|
Osteoprogenitor cells
|
|
|
secrete extracellular matrix and are responsible for new bone formation. Once the osteoblast is finished filling in a cavity the cell becomes flattened and line the surface of the cell. They are now called lining cells
|
Osteoblasts
|
|
|
bone-resorbing cells that are responsible for “dissolving” the bone when the bone is being removed, reorganized, or where the bone is damaged. These cells are the result of more than one cell fusing, and therefore, usually have more than one nucleus
|
Osteoclasts
|
|
|
these cells are derived from osteoblasts. When new bone is being formed some of the osteoblasts are surrounded with its secreted matrix and form osteocytes. These cells develop long branches in order to avoid isolation.
|
Osteocytes
|

