![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
108 Cards in this Set
- Front
- Back
|
Collagen cells are called
|
chondrocytes
|
|
|
Chondrocytes: abundance, lifespan and purpose
|
5% of total collagen; "long-lived;" elaborate and maintain extracellular matrix (the other 95% of collagen volume) and retain the capacity for growth and division; they produce, maintain and repair the matrix
|
|
|
Extracellular Matrix
|
Composed of extracellular fibers; gel-like, hydrated ground substance
|
|
|
Four common features of collagenous tissues
|
Highly hydrated extracellular matrix ground substance; this ground substance is reinforced by various types of Collagen Type II; cells are walled off in separate lacunae; no vasculature or lymphatic networks
|
|
|
Describe the architecture of cartilage that gives it its resiliency
|
Individual chondrocytes surrounded by a matrix of a fibrous network of collagen and gelatinous ground substance of negatively charged GAG's that attracts and holds a lot of water
|
|
|
Chondrocytes and mitochondria
|
They have a lot of mitochondria since they are very metabolically active
|
|
|
Extracellular Matrix Components
|
60-80% water; 9% proteoglycans; 5% is multiadhesive glycoproteins
|
|
|
Extracellular Matrix: Collagen Types
|
Usually Type II, but in fibrocartilage it is mostly Type I
|
|
|
Glycosaminoglycans of the ECM
|
long, neg. charged polysaccharide chains that attract water that covalently link to core proteins to form proteoglycans
|
|
|
In collagen, proteoglycans are
|
highly sulfated with groups such as chondroitin sulfate or keratin sulfate to increase attraction of water
|
|
|
How to form a proteoglycan aggregate
|
A proteoglycan attaches to hyaluronan via link proteins
|
|
|
An especially important proteoglycan for hyaline cartilage
|
aggrecan: attracts large amounts of water; also found in elastic cartilage; 100 chondroitin sulfate chains + 60 keratin sulfate chains
|
|
|
Important proteoglycan in fibrocartilage
|
Versican
|
|
|
Proteoglycans joining to hyaluronan makes 2 things happen
|
limits mov't of large molecules & allows metabolites and small molecules to pass via diffusion to keep the collagen well hydrated while being avascular
|
|
|
Capsular Matrix
|
highest concentration of collagen type IV fibers that form a tightly woven enclosure around each chondrocyte; highest conc. of sulfated proteoglycans, which gives it the highest amount of basophilia in H&E stains; the type IV collagen will bind to integrin receptors on the cell surface
|
|
|
Territorial Matrix
|
less SP's; a randomly arranged network of Type II fibers; surrounds isogenous groups
|
|
|
Interterritorial Matrix
|
least SP's and least basophilic in stains (stains the lightest); surrounds the territorial matrix and fills space between groups of chondrocytes;
|
|
|
Hyaline cartilage
|
flexible support and relative rigidity and compressibility; found on surfaces of synovial joint; most common; deep blue on H&E; prominent lacunae and chondrocytes shrink during processing, leaving artifacts; isogenous groups centrally; have perichondrium except on articular surfaces
|
|
|
Elastic cartilage
|
flexible support and elasticity;
|
|
|
Fibrocartilage
|
flexible support and tensile strength
|
|
|
What happens to injured collagen?
|
It can calcify and become bone-like, which can cause joint problems. Repair is possible sometimes, but normally involves forming Type I collagen and doesn't function as well as the original Type II
|
|
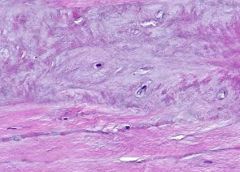
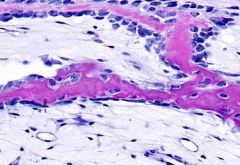
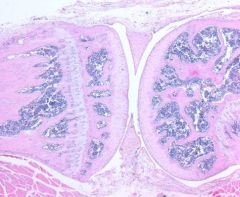
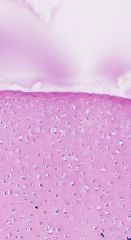
What type of cartilage is this?
|
Fibrocartilage
|
|
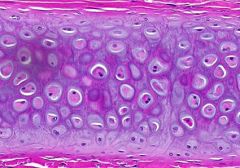
What type of cartilage is this?
|
Elastic
|
|
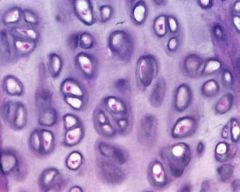
What type of cartilage is this?
|
Hyaline
|
|
|
A list of things Hyaline cartilage is involved in
|
fetal skeleton; epiphyseal plates; synovial articular surfaces; costal cartilage; nasal cartilage; larynx; trachea; bronchii
|
|
|
Perichondrium is involved in ____ growth
|
apositional
|
|
|
Three prominent organelles of chondrocytes
|
rough ER, golgi, secretory vesicles
|
|
|
Slide differences between hyaline and elastic cartilage
|
Elastic has fewer isogenous groups and more single cells visible; elastic fibers might hide territorial/interterritorial matrix, elastic cartilage has branching fibers in the ECM
|
|
|
Where is elastic cartilage?
|
external ear, auditory tube, epiglottis/some laryngeal cartilages
|
|
|
Fibrous cartilage: appearance on slide
|
highly fibrous, relatively parallel array of Type I fibers; no perichondrium (so no appositional growth); visible isogenous groups (so interstitial growth occurs)
|
|

The arrows are pointing to
|
isogenous groups in fibrocartilage
|
|
|
A list of where fibrocartilage is found
|
Tendon insertions to bone, intervertebral discs, pelvic symphysis, temperomandibular articular disc, stifle meniscus, palmar carpal ligament
|
|
|
Molecules that regulate chondrogenesis
|
matrix proteins, transcription factors, ligands, nuclear receptors and adhesion molecules
|
|
|
Describe embryonic cartilage dev't
|
aggregates of mesenchymal cells form condensed masses of round, closely apposed cells. Transcription factor SOX-9 is released and directs the differentiation of these cells into chondroblasts.
|
|
|
Describe appositional growth
|
"growth from the edges;" done by hyaline and elastic cartilage; chondroblasts deposit new matrix on existing cartilage; these chondroblasts differentiate on the inner layer of the perichondrium
|
|
|
Describe interstital growth
|
"things divide and push apart internally;" chondrocytes divide within their lacunae and form isogenous groups; all cartilages do this
|
|
|
How do nutrients get into bone?
|
gap junctions; there is no diffusion into/out of bone
|
|
|
Bone serves as a storage site for
|
Ca and Phosphorous
|
|
|
Compact bone
|
forms thick outer walls of bones, especially in diaphyseal walls of long bones
|
|
|
Cancellous bone
|
aka spongey bone; forms "marrow cavities," especially near metaphyseal site in mature bones and epiphyses
|
|
|
Long bone regions, from terminal end to more proximal
|
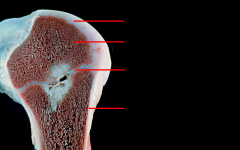
Epiphysis (above growth plate); physis (hyaline cartilage growth plate); epiphyseal line; metaphysis; diaphysis; marrow cavity on inside
|
|
|
How do blood & nutrients enter bone?
|
via nutrient and epiphyseal arteries that travel through nutrient foramina
|
|
|
How does blood leave bone?
|
through periosteum
|
|
|
Major route of entry for arteries into compact bone?
|
Volkmann's Canals
|
|
|
Bone tissue lacks these vessels
|
lymphatic
|
|
|
Fundamental unit of compact bone
|
osteon, aka Haversian System; composed of concentric lamellae around a central neurovascular (Haversian) canal; between osteons are wedges of bone called interstitial lamellae;
|
|
|
Outer vs. inner circumferential lamellae
|
outer: encircle compact bone tissue under outer capsule (periosteum); inner cover medullary surface of bone tissue beneath a thin endostium
|
|
|
Haversian canals and Volkmann's canals
|
Haversian normally run longitudinally and are transected by Volkmann's canals
|
|
|
Periosteum vs. endosteum
|
Endosteum: inner layer of bone; periosteum: outer bone capsule
|
|
|
Processing (clean/wash/bleach/dry) for histology removes all living tissue from bone, including
|
periosteum; osteocytes; blood vessels, Haversian Canal components; Volkmann Canal components; endosteum
|
|
|
Why do osteocytic lacunae, Haversian or Volkmann Canals and canaliculi look black on slides?
|
Air has a lower refractive index than the medium used for ground bone
|
|
|
What are canaliculi?
|
On a slide, they are thin wavy lines that connect lacunae
|
|
|
Interstitial lamellae
|
are fragments of previously laid down osteon lamellae which were superseded by newer osteons laid down during compact bone remodeling. They occupy angular regions between adjacent osteons. They contain lacunae and canaliculi, but lack central canals
|
|
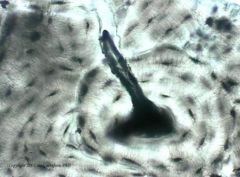
Describe what is shown here
|
This is a Volkmann Canal protruding from a Haversian Canal, demonstrating how they transect and run perpindicular to each other
|
|
|
Differences in appearance of cancellous and compact bone
|
Cancellous bone has no osteons, osteon concentric lamellae, interstital lamellae, but it does have unique bony trabeculae, bony trabecular lamellae, bony canaliculi, and osteocytes
|
|
|
Spongey bone is made of
|
anastomotic trabeculae, which are apposed lamellae layers
|
|
|
How do oxygen and nutrients get into cancellous bone?
|
diffuse through canalicular openings at the bone tissue/marrow interface
|
|
|
Woven bone vs. Mature bone
|
the inner part of woven bone is actually mineralized cartilage, not yet calcified bone; in woven bone you can see the clear pattern of laid down osteoid; in mature bone, this pattern has been digeted away and replaced with concentric lamella
|
|
What type of bone is this?
|
Mature (lamellar)
|
|
What type of bone is this?
|
Immature (woven)
|
|
|
Mesenchymal cells can differentiate into these bone cells
|
osteoprogenitor (become osteoblasts when triggered by transcription factor CBFA-1), osteoblasts (mineralize bone matrix, secrete type I collagen in osteon), osteocytes (maintain matrix in mature bone), bone lining cells (cover bone that isn't being remodeled)
|
|
|
Bone lining cells
|
form periosteum on outside of bone and endosteum on inside of bone
|
|
|
Where do osteoclasts come from?
|
arise from hemopoetic progenitor cells
|
|
|
The key factor of triggering osteoprogenitor cells to become osteoblasts
|
Core Binding Factor Alpha 1 (CBAF1)
|
|
|
Three parts of the bone matrix secreted by osteoblasts
|
Type I Collagen (90% of protein in bone); bone matrix protein (Ca-binding proteins, multiadhesive glycoprotiens, proteoglycans) and Matrix vesicles (rich in alkaline phosphatase, which is involved in Ca and Pi depositing as hydroxapatite crystals)
|
|
|
When does an osteoblast become an osteocyte?
|
When it is completely surrounded by bone matrix or osteoid
|
|
|
Bone lining cells are thought to do what?
|
Regulate movement of Ca and Pi in and out of bone; maintenance and nutritional support of osteocytes
|
|
|
What forms the callus at fracture sites?
|
bone lining cells
|
|
|
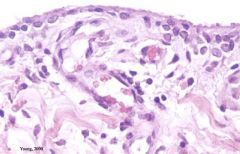
What are osteoclasts?
|
multinucleate giant macrophages that are members of the mononuclear phagocyte system (MPS); they are resorptive cells that remodel bone and bind to bone via integrins and form remodeling bays called Howship's lacuna; they secrete enzymes to break down bone matrix and decalcify bone
|
|
|
Osteoclasts: derived from
|
fusion of blood monocytes
|
|
|
Osteoclasts and H&E stain
|
eosinophilic cytoplasm due to acid phosphatase-containing lysosomes
|
|
|
Osteoclast: structure
|
Ruffled border: portion of cell in direct contact with bone; has multiple in-foldings of the cell membrane that allows a large surface area for the generation of protons for acidification and for exocytosis of digestive enzymes for both mineral dissolution and matrix digestion
Clear zone: a ring-like perimeter (sealing zone) of cytoplasm adjacent to the ruffled border that demarcates the area being resorbed. It provides a tight seal between the plasma membrane and the mineral matrix of the bone. |
|
|
Osteoclast: function in steps
|
first, decalcify bone via acidification; then lysosomes release hydrolytic enzymes to degrade collagen and other bone matrix proteins
|
|
|
Osteogenesis: two ways
|
Endochondral ossification: bone forms on a hyaline cartilage model/framework; growth is all at ends of bones from endochondrium only
Intramembrous ossification: no cartilage frame, osteoblasts develop directly from mesenchyme within a membrane of condensed mesenchyme cells, and osteoid is deposited into mesenchyme itself; growth increases bone width and includes perichondrium and endochondrium |
|
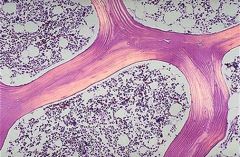
What is this a sample of?
|
mature cancellous bone
|
|
What is this a sample of?
|
immature cancellous bone
|
|
|
How are Haversian Canals formed?
|
Maturing bone entraps blood vessels
|
|
|
What does mature cancellous bone NOT have?
|
Haversian Canals
|
|
|
Where is cancellous bone re-absorbed?
|
trabecular surface (whether mature or immature)
|
|
|
Resorption canals: orientation
|
same axis as Haversian Canals
|
|
|
All bone starts as
|
spongey bone
|
|
|
Bone tissue that is growing by intramembranous ossification behaves ___ in stains
|
eosinophilic (no basophilic cartilage is around), and appear more-so if they enlarge and secrete more matrix
|
|
|
Bones that grow by intramembranous ossification
|
calvaria components (frontal, parietal, temporal, part of occipital), facial bones, part of mandible, clavicles
|
|
|
Bones that form by intramembranous ossification grow how?
|
appositional growth
|
|
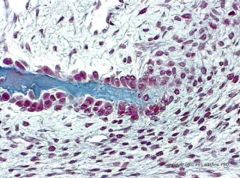
What kind of stain is this and what is it showing?
|
Trichrome; intramembranous growth of bone
|
|
|
Non-developing bones can only grow via
|
appositional growth
|
|
|
Endochondral ossification is seen in what bones?
|
Long bones, pelvis, base of skull
|
|
|
Trace the steps of endochondral ossification
|
A collagenous framework is formed with the periosteum; cartilage is calcified in the diaphyseal region as chondroblasts form a collar of bone, while on the inner part chondroblasts secrete alkaline phosphatase to calcify the structure; this calcification inhibits nutrient entry and the marrow space forms; the first structures to calcify will also provide the first places for appositional growth
|
|
|
Primary vs. Secondary Ossification Center
|
primary: forms from osteoblasts that are located on the first bone collar, at the same location where blood vessels penetrate the collar; secondary: form at ends of long bones/physes (growth plates)
|
|
|
5 zones of endochondral bone growth cartilage
|
1. Zone of Reserve cartilage: chondrocytes in this region are inactive with no matrix production.
2. Zone of proliferating cartilage – chondrocytes enlarge, start dividing and align in distinct cell columns. 3. Zone of cartilage hypertrophy – chondrocytes enlarged further, produce types I & X cartilage in addition to VEGF which initiates vascular invasion. 4. Zone of calcified cartilage – hypertrophied chondrocytes die by apoptosis as cartilage matrix becomes calcified. 5. Zone of resorption – calcified cartilage is invaded by blood vessels resulting in parallel spicules of calcified cartilage. Osteoblasts attach to these spicules and begin depositing osteoid which become calcified to form bone |
|
|
Explain growth at the physis
|
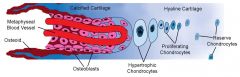
Blood vessels from the metaphysis reach out to this region, bringing osteoblasts that will lie down osteoid and new bone on the calcified cartilage core
|
|

What is the red arrow pointing to?
|
An osteoclast (pictured is endochondral bone forming)
|
|

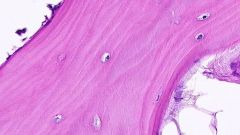
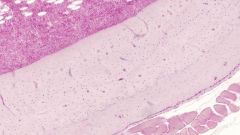
Describe what is pictured here
|
Farthest right: periosteum; farthest left: marrow space (medullary cavity) full of blood cells (purple); the dark spots inside the shaft (middle region) are Haversian Canals
|
|

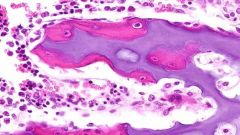
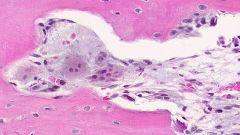
Describe what is pictured here
|
An osteocyte; the two projections to the left are fine cytoplasmic processes penetrating the canaliculi and "synapse" with other osteocytes via gap junctions; the white region surrounding is un-mineralized collagenous matrix
|
|
|
Remodeling: diaphyseal and metaphyseal region
|
Diaphyseal: bone is formed on periosteal surface and resorbed on endosteal surface
Metaphyseal: bone is formed on endosteal surface and resorbed on periosteal surface |
|
What is pictured here?
|
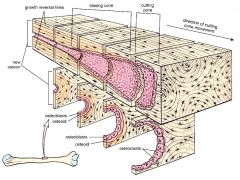
a cutting cone of a Haversian Canal (the widest part of the canal)
|
|
What is pictured here?
|
Another cutting cone of a Haversian Canal
|
|
|
Three joint types
|
Same as in gross anatomy...
1. Fibrous joints (little to no mobility) – bones held together by collagenous or dense elastic connective tissue. Examples: flat bones of the skull; fibrous articulation between the radius and ulna. 2. Cartilaginous joints (limited mobility) – bones connected by cartilage. Examples: intervertebral disks, pelvic symphysis and the physis of growing endochondral bone. 3. Synovial joints (free motility) – characterized by a hyaline cartilage cap on the opposing bone surfaces in addition to a lubricating synovial fluid enclosed within a joint cavity by a joint capsule. |
|
|
Articular cartilage: 3 interesting things
|
No perichondrium; made of hyaline cartilage; nutrients are gained by diffusion from synovial fluid
|
|
What kind of joint is this and what kind of cartilage is here?
|
Synovial; articular (hyaline)
|
|
What is this a sample of? (hint: in a joint)
|
Synovial membrane
(has type A cells that are phagocytic and type B that secrete synovial fluid, but we don't need to identify them on a slide) |
|
What is pictured here?
|
Fetal articular cartilage
|
|
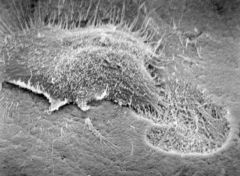
This is an ECM scan of what?
|
an osteoclast
|
|
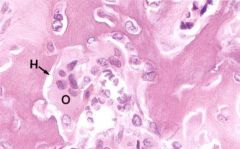
What is H, and what is O?
|

O: osteoblast; H: Howship's Lacunae
|
|

What kind of bone is this?
|
Mineralized compact
|
|
What is this a sample of?
|
Demineralized compact bone
|
|
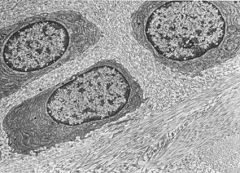
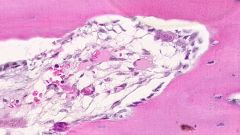
What are these called?
|
Isogenous groups (inside a proteoglycan globule rich matrix and packaged inside Type I collagen bundles)
|
|
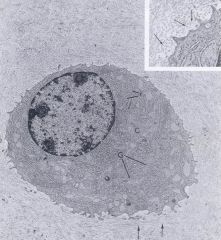
What is this cell, what is labeled as G and what is labeled as r?
|
This is a chondrocyte; G is the well-developed Golgi and r is the rough ER. The arrows point to the globular appearance of hyaluronan and proteoglycans in EM scans
|

