![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
2 major categories of Functional disorders?
2 major categories of Quantitative defects? |
1. Problems with Chemotaxis (getting to site of infection)
2. Defects in Phagocytosis and Killing Quantitative: Neutropenia, Neutrophilia |
|
|
What are two disorders of Chemotaxis? What is their common clinical presentation?
|
1. Leukocyte Adhesion Deficiency (LAD)- AR disease, defect in B2-integrin (an adhesion molecule). Recurrent bacterial infections.
2. Lazy Leukocyte Syndrome- neutrophils don't respond to chemotactic factors. Severe bacterial infections. |
|
|
What are 3 neutrophil disorders of Phagocytosis/Killing?
|
1. CGD (Chronic Granulomatous Disease)- NADPH oxidase defect (can't form free radicals to kill ingested microbe). Form granulomas. AR disorder with recurrent infections.
2. MPO deficiency (microbicidal agent in primary granules. need both this and H2O2 to kill bugs) 3. Chediak-Higashi syndrome (vesicle trafficking disorder, can't form phagolysosome) |
|
|
How do you calculate ANC (Absolute Neutrophilic Count)?
Should an ANC of 1400 in an African American/Arab raise suspicion? |
ANC= Total #WBC x (%bands + segs)
Neutropenia is typically <1500-1800 BUT in certain ethnicities, ANC runs low ("benign ethnic neutropenia"), so it is OK. |
|
|
What is mild neutropenia? moderate? severe?
How do patients with severe neutropenia present? |
Mild= 1000-1500
Moderate= 500-1000 Severe= <500 (High risk of infection, SEPSIS) |
|
|
What is the typical clinical presentation of a neutropenic patient?
How does the presentation of a neutropenic patient with an infection differ from that of a healthy person with an infection? |
Fever & Signs/Symptoms of infection (mucous membrane, skin, genital, and peri-rectal areas)
*Neutropenic patients might not show warmth and swelling (typical signs of infection seen with neutrophil chemotaxis) |
|
|
What is the most FREQUENT cause of Neutropenia?
|
DRUG induced decreased production of neutrophils
(can also be due to aplastic anemia, cancer, and myelodysplastic disorders, etc.) |
|
|
Examples of drugs that induce Neutropenia?
|
- Chemotherapeutic agents (alkylating agents, antimetabolites, etc.). They also cause anemia/thrombocytopenia.
- Idiosynchratic rxn (may not always result in neutropenia): Chloramphenicol, SULFA drugs, Phenytoin, CBZ, Chlorpromazine (anti-psych), Gold |
|
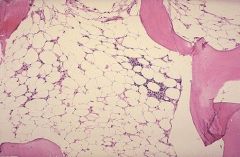
What condition is shown in this image? How do you calculate cellularity of the bone marrow?
|
Aplastic Anemia (bone marrow failure that leads to pancytopenia --> anemia, thrombocytopenia, neutropenia.
Normal % cellularity= 100-age |
|
|
What is a congenital cause of aplastic anemia?
|
Fanconi Anemia - AR disorder of DNA repair. Pancytopenia, skeletal abnormalities, Increased tumors/leukemia.
|
|
|
Majority of aplastic anemia cases are _____.
What are some secondary causes? |
Idiopathic (~70%)
Secondary= 1.Ionizing radiation 2. Chemicals (organophosphates) 3. Drugs (chemotherapeutics, SULFA, gold, psychotropics, anticonvulsants, anti-depressants) 4. Viruses (Non-ABC Hep) |
|
|
A patient with sickel cell anemia develops a virus illness and you note that they have a low reticulocyte count and anemia. What condition is the causative agent? What are you worried about in these patients?
|
Aplastic Crisis
Parvovirus B19- infects retics and can cause "APLASTIC CRISIS" in patients who have already shortened RBC survival and need high retic count to maintain their Hb. |
|
|
What is the treatment for someone with Drug induced aplastic anemia?
|
1. Remove Offending Agent!
Supportive care (blood transfusion), G-CSF, Stem cell transplant, etc. |
|
|
What is the Kostman Syndrome?
How do you treat it? |
A severe congenital disorder (AR). Defect in gene encoding Neutrophil Elastase (causes life-threatening BACTERIAL infections).
Rx. recombinant G-CSF |
|
|
What is Cyclic Neutropenia? How do you treat it?
|
AD disorder (variable expression), neutropenia occurs every 3-4 wks (for about 6 days).
Sx. include fever, illness, mouth ulcers. With age, neutropenia becomes less severe. Rx. Abx + G-CSF (mainly supportive). |
|
|
What are some conditions that can cause neutropneia due to Increased Destruction of neutrophils?
|
1. Autoimmune neutropenia
2. Splenic enlargement (can trap and destroy cells) 3. Increased peripheral utilization (SEPSIS or overwhelming infection) |
|
|
What causes an Increased number of bone marrow precursors (neutrophilia)?
What about an increased release of neutrophils from marrow stores? |
Increased number- chronic infections, tumors, myeloproliferative disorders
Increased release- endotoxemia, acute infection, hypoxia |
|
|
What is the Leukemoid Reaction? What will you see on CBC?
What malignant condition presents with identical findings on blood smear? |
Normal physiologic response to severe stress/infection.
You will see a prominent Left shift (increases in metamyelocytes, and maybe even myelocytes/promyelocyte). Distinguish from CML (9:22 chromosomal translocation, or Philadelphia chromosome) |
|
|
What causes demargination of neutrophils?
What causes decreased neutrophil entry into tissues? |
Demargination= exercise/ epinephrine
Decreased entry into tissues= glucocorticoids |
|
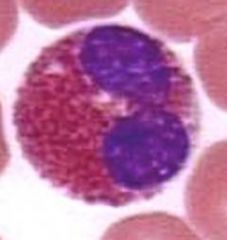
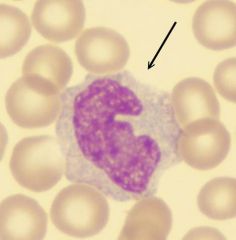
What is this cell? What is a high percentage of this cell?
|
Eosinophil, >10%= high (nl=1-4%)
NAACP= Neoplasia, Asthma, Allergic process, Collagen vascular disease, Parasite |
|
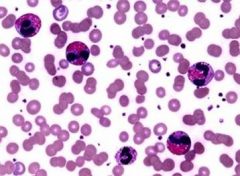
This smear shows what rare syndrome?
What organs might be affected in this person? What drug is used to treat it? |
Hypereosinophilic Syndrome (genetic defect involving fusion protein). Infiltrating eos cause multiple organ defect including HEART, SKIN, and LUNG.
Imatinib (Gleevec)- used to treat CML as well |
|
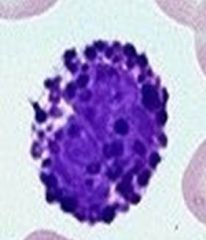
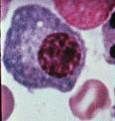
What is this cell? What is contained in the granules?
What conditions could high levels of this be seen in? |
Basophil (large purplish granule). Contains heparin sulfate, histamine, leukotriene.
Seen in CML (myeloproliferative disorders), hypersensitivity, and inflammatory rxns. |
|
What form of this cell is seen in circulation? in tissues?
High levels of this cell are seen in what condition? |
Monocyte= circulation, Macrophage = tissues (grey cytoplasm, large, looks atypical).
Monocytosis- from 1) chronic inflammatory state such as TB or endocarditis, 2) myeloproliferative disorders, 3) temporary increase after marrow-suppressive chemo |
|
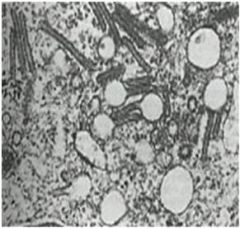
What condition is shown by this biopsy? Is it malignant or non-malignant?
Cells would be positive for what defining stain? |
Histiocytosis X or Langerhans cell Histiocytosis (non malignant). Neoplasm of macrophages.
Organelle of unknown fxn called Birbeck granule (tennis racquet shape). Stain s-100 positive (neural crest derivatives). |
|
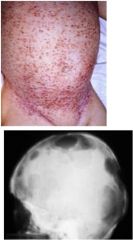
What is this condition called and how can you tell? What age group is most commonly affected?
|
Childhood/ infancy
Variable clinical presentation but you see Multiple lytic bone lesions and eczematoid skin rash. Can also involve CNS, lung, liver. |
|
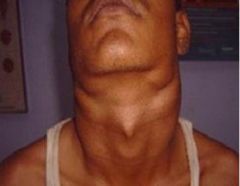
A youth with massive, painless bumps on their neck comes to see you. What do you suspect?
|
Rosai-Dorfman Syndrome = sinus histiocytosis with massive lymphadenopathy.
A type of non-langerhan cell histiocytoses. Patients have chronic, painless, cervical lymphadenopathy, fever, and weightloss. Subsides on it's own (self-limited). |
|
What is this cell called? Where should it be found?
|
Plasma cell- found in TISSUES (B -cell in circulation).
Has a golgi body (little white dot), and chunky blue cytoplasm (nucleated RBC has red cytoplasm). |
|
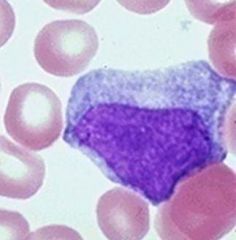
What is the most common condition in young people that presents with increase in this type of cell?
What test is used to confirm? |
Mono (lymphocytosis) -from viral infection with EBV. Fever, sore throat, lymphadenopathy.
Mono-spot test (heterophile antibody titers) are used to confirm. *note- this is an atypical lymphocyte, increases in size from a normal lymphocyte when activated |

