![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
12 Cards in this Set
- Front
- Back
|
What is CML?
What is the specific karyotypic abnormality linked to it's pathogenesis? |
CML= chronic myelogenous leukemia (an MDS in which there is clonal expansion of primitive progenitor HSC but mainly affects the myeloid lineage).
t(9;22) aka the Philadelphia Chromosome. Causes a BCR-ABL fusion protein (BCR on ch. 22, ABL on ch. 9) |
|
|
What percentage of CML cases are associated with the 9;22 translocation?
What is the role of the fusion protein in the pathogenesis of CML? |
95% (almost all of CML) have translocation. 20% of ALL have it too.
BCR-ABL does multiple things. This fusion is a tyrosine kinase with high activity, constitutitively active. Activates mitogenic pathways (RAS, MAP kinase, etc.) |
|
|
How are variants of BCR-ABL proteins formed? What variant is associated with the majority of CML?
Why does one malignant clone (leukocytes) dominate in CML? |
Variants form due to different breakpoints of BCR and ABL. P210 is associated with CML.
The mutation causes increase in growth of that one cell line but feedback mechanisms are activated that lead to suppression of other cell lines. |
|
|
What is the median age for diagnosis of CML?
What are the major symptoms at diagnosis? |
Median age= 56 (M>F)
Sxs: Fatigue, Weight loss, Abdominal fullness (from splenomegaly), Bruising/Bleeding (from thrombocytosis or thrombocytopenia). |
|
|
What are the 3 phases of CML?
|
1. Chronic phase: premalignant, fatigue, sxs of splenomegaly, etc. 3-5 years.
2. Accelerated phase: CML changing to blast crisis. Rapid doubling of WBC, increased promyelocyte and blasts in BM. 3. Blastic phase: Greater than 20% of blasts in the BM. |
|
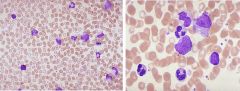
What is shown on this peripheral blood smear?
Why does CML fail to remain in the indolent chronic phase? |
This is chronic phase of CML. You can tell because mostly you see neutrophils in excess. In this phase, the patient may not progress to full sxs.
Chronic phase develops more mutations and lead to clonal evolution and myelofibrosis. |
|
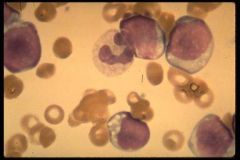
What phase is shown here? How can you tell?
(hint: think of the last two phases of CML) |
Accelerated and Blast phase. You can tell that there are more immature cells in the peripheral blood smear (promyelocytes and myelocytes).
Accelerated phase- rapidly doubling WBCs with promyelocytes. Here chronic phase --> blast crisis (block in differentiation). In order to be a BLAST phase, there must be >20% blasts in the bone marrow. |
|
|
What are different ways that you can cause "leukoreduction" in CML?
How does Interferon Alpha work? |
Luekoreduction- leukophoresis, hydroxyurea, and cytarabine
Interferon- unknown MoA but has antiproliferative effects. It is a naturally produced glycoprotein in response to antigenic stimuli. |
|
|
What are the disadvantages to using Interferon-alpha?
What about an allogenic stem cell transplant (BM)? |
Interferon- improved survival but patients feel like they have flu and it's costly.
BM transplant- they can induce complete remission in patients (non-detectable BCR-ABL) and also infusion of donor T cells can attack leukemic cells. But only a certain number of people can get it. Not as effective for accelerated or blast disease. |
|
|
What is the mechanism of action of the targeted therapy for CML?
|
Imatinib mesylate will bind the kinase pocket of BCR-ABL (I.e. ATP binding pocket), preventing phosphorylation of substrate and downstream signaling. Good in ALL phases of CML.
|
|
|
What are the major limitations to using Imatinib?
How does resistance develop? |
Resistance, Intolerance (Side effects: people get diffuse, achy joint pains, horrible rash). Very costly.
Resistance: spontaneous mutations of tyrosine kinase binding domain. |
|
|
How would you treat a patient with resistance to Gleevec?
What is the only known CURE for CML? |
- dose escalate their imatinib
- use 2nd generation kinase inhibitor (ex: Pronatimib or Dasatinib- inhibits SCR-ABL which signals downstream from BCR-ABL) Cure= Stem Cell transplant |

