![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
12 Cards in this Set
- Front
- Back
|
What happens in Aplastic Anemia?
|
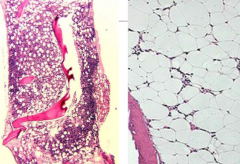
Too few Hematopoietic Progenitor Cells / BM Failure:
- Don't have enough RBCs (pale, fatigued) - Don't have enough WBCs (infections) - Not enough platelets (bruising, nose bleeds) (Healthy on L and aplastic on R) |
|
|
What are the well recognized inherited BM Failure Syndromes to know for the exam?
|
- Diskeratosis Congenita
- Fanconi Syndrome |
|
|
What causes Diskeratosis Congenita?
|
- *BM INHERITED* disorder of poor telomere maintenance
- Telomerase enzyme is supposed to keep the ends of chromosomes longer - In Diskeratosis Congenita you have *SHORT TELOMERES* early in life (assess w/ qPCR) |
|
|
What causes Fanconi Syndrome?
|
Defect of DNA Repair
|
|
|
What do you need to ensure before you give a patient chemo?
|
**Make sure they don't have FANCONI ANEMIA because they WILL NOT BE ABLE TO REPAIR THEIR DNA** (Deb Test??!)
|
|
|
What is the presentation of a patient with Inherited BM Failure Disorder?
|
- 2/3 will have changes such as to bones, very short, extra thumb, very small head etc
***** 1/3 will have a NORMAL physical exam - THIS DOES NOT MEAN THEY CAN'T HAVE BM FAILURE ***** |
|
|
EXAM: Your best friend's daughter is <25 years old and has a HLA matched sibling from which she is going to get a BM Transplant. What test must you do first before you give the BMT?
|
DEB Test(?) to assess for Fanconi Anemia because if you give her chemotherapy to prevent her from GVHD or rejection, she may die from not being able to repair her DNA (Fanconi Anemia causes a DNA repair defect)
|
|
|
On which chromosome are the HLA major antigens? What are they?
|
Chromosome 6:
- HLA Class I - A, B, C - HLA Class II - DR, DQ, DP |
|
|
What are the chances of a sibling being a matched donor?
|
1/4
|
|
|
What are the criteria for diagnosing Severe Aplastic Anemia?
|
Peripheral blood (requires 2/3):
- Neutrophils < 500/µL - Platelets < 20,000 / µL - Reticulocytes < 20,000 / µL (corrected reticulocyte <1%) Bone Marrow: - Marked hypocellularity w/ < 65% of residual BM cells being non-hematopoietic |
|
|
**How do you treat an acquired BM failure?
|
- Best: Matched sibling BMT (<25 yo) (>90% success)
***** If no matched sibling, Best: Intensive Immunosuppressant Therapy (>80% success) - Next best: Unrelated Donor BMT (~90% success) |
|
|
What is the best course of treatment for a patient with acquired BM failure if they don't have an HLA matched sibling?
|
Intensive Immunosuppressant Therapy:
- ATG (horse and rabbit antibodies against human T cells) - Cyclosporine A (CSA) - calcineurin inhibitor) - Prednisone (80% success rate, but 30% will relapse over time) |

