![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
What are causes of pancytopenia?
|
Aplastic anemia
Myelodysplastic syndromes Bone marrow infiltration' Nutritional deficiencies Bone marrow toxins Infections Hypersplenism Systemic disorders Anorexia |
|
|
What are some bone marrow infiltrates that can cause pancytopenia?
|
Leukemia
Lymphoma Carcinoma Granulomatous disease Fibrosis Congenital storage disease |
|
|
What are some nutritional deficiencies taht can cause pancytopenia?
|
B12
Folic acid |
|
|
What are some bone marrow toxins that can cause pancytopenia?
|
Chemo
Radiation Chemical exposure Alcohol |
|
|
What are some infections that can cause pancytopenia?
|
HIV
EBV Parvovirus Hepatitis Histoplasmosis Tb |
|
|
What is the definition of aplastic anemia?
|
Peripheral blood pancytopenia
Bone marrow hypocellularity |
|
|
When can AA occur?
|
Any age!
|
|
|
What are causes of acquired AA?
|
Acquired (vs. inherited) are 80% of the AA cases
Of those: Idiopathic (50%) Also: Meds Toxins Viruses Immune disorders Others |
|
|
What are some meds that can cause acquired AA?
|
Chloramphenicol
Gold Sulfonamides NSAIDs Arsenic Antiepileptics Clopidogrel |
|
|
What are some toxins that can cause acquired AA?
|
Benzene
Alcohol Chemo Radiation |
|
|
What are some viral infections that can cause acquired AA?
|
EBV
Non-A, B, C hepatitis HIV Parvovirus B19 |
|
|
What are some immune disorders that can cause acquired AA?
|
SLE
Transfusion associated graft vs. host disease Eosinophilic fascitis |
|
|
What are some other causes of acquired AA?
|
Paroxysmal nocturnal hemoglobinuria
Thymoma Pregnancy |
|
|
What are the characteristics of inherited AAs?
|
In the context of other symptoms
Early onset |
|
|
What's the clinical presentation of AA?
|
Anemia:
Neutropenia Thrombocytopenia |
|
|
What are some of the signs and symptoms of anemia?
|
Pallor
Fatigue Chest pain SOB Headache |
|
|
What are some of the symptoms of neutropenia?
|
Fever
Infections |
|
|
What are some of the symptoms of thrombocytopenia?
|
Bruising
Petechiae Epistaxis Gingival bleeding Menorrhagia |
|
|
What labs should you order in the context of aplastic anemia?
|
CBC
Reticulocyte count (is the bone marrow working?) Bone marrow biopsy: look for the hypocellularity Work them up to look for other potential causes |
|
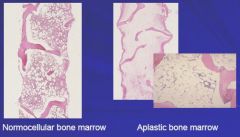
Take a look at this:
|
In AA, there is essentially NOTHING in the marrow.
|
|
|
What are the grades of AA?
|
Nonsevere: <30% marrow cellularity; absence of pancytopenia
Severe: Marrow < 25% OR <50% with few hematopoietic cells and pancytopenic signs Very severe: see severe, but with ANC <.2E9 |
|
|
What's the pathogenesis of aplastic anemia?
|
Damage/destruction/suppression of the hematopoietic stem cell leads to a depletion of the stem cell pool-->marrow failure-->AA
|
|
|
What are the mechanisms by which the pathogenesis of AA can happen?
|
Direct toxic effects to the hematopoietic stem cells
Immune mediated suppression of the hematopoietic stem cell |
|
|
What's the supportive treatment for AA?
|
Supportive care:
-Transfusions -Iron chelating agents -Antibiotics -Growth factor support: GCSF, EPO |
|
|
What's the curative treatment for AA?
|
Hematopoietic stem cell transplantation
Immunosuppressants |
|
|
What ages do you do a hematopoietic stem cell transplant for if they have AA?
|
Under 45.
Try and get a matched sibling donor; otherwise you can use an unmatched. |
|
|
What's the prophylaxis used for GvHD in allogenic hematopoietic stem cell transpant (HSCT)?
|
Methotrexate/cyclosporine
|
|
|
What are the meds that you give to someone before a HSCT to prepare them?
|
Cyclophosphamite
Antithymocyte globulin HSC infusion |
|
|
What's the prognosis for someone who gets a HSCT with AA?
|
88% survival at 8 years
32% with chronic GvHD 4% graft failure |
|
|
What are the complications following HSCT?
|
Graft failure
GvHD (more common with unrelated donors) Malignancy |
|
|
What are some complications to the immunosuppression for HSCT to cure AA?
|
Serum sickness
Renal failure HTN Late malignancies (MDS/AML) |
|
|
How long after HSCT does it take to see a response?
|
3-4 months
|
|
|
What cells go awry in myelodysplastic syndrome?
|
Clonal hematopoietic stem cells
|
|
|
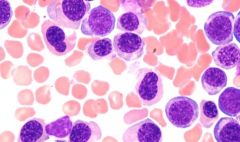
What are the findings in myelodysplastic syndrome?
|
Peripheral blood cytopenias
Hyperplastic (uaully) bone marrow with dysplasia |
|
|
What are the symptoms found in myelodysplastic syndrome?
|
Anemia
Neutropenic symptoms Thrombocytopenic hemorrhage, easy bruising Symptomatic organomegaly/LAD Bone/joint pains Weight loss Night sweats No lymphadenopathy |
|
|
What are some of the findings in the RBCs in myelodysplastic syndromes?
|
Macrocytic
Nucleated RBCs Poikilocytosis: abnormally shaped RBCs Anisolytosis: variance in size |
|
|
What are some WBC findings in myelodysplastic syndromes?
|
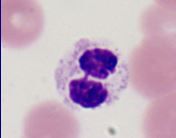
Pelger-Huet neutrophils; neutrophils whose nuclei are hyposegmeneted
|
|
|
What is the hallmark of myelodysplastic syndrome in the RBC precursor in bone marrow?
|
Megaloblastic maturation in RBC precursors: the nuclei and the cytoplasm mature at different rates; nuclei lags behind
|
|
|
What are the pathologic changes in megakaryocyte development in the bone marrow in myelodysplastic syndrome?
|
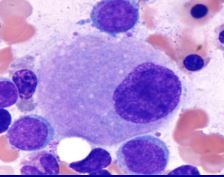
Multiple separate nuclei
Unilobate megakaryocytes (instead of many-lobed) Small platelets |
|
|
Cytogenetically, how do you differentiate between myelodysplastic syndrome and aplastic anemia?
|
MDS: typically show more chrosomal abnormalities
Commonly deletions/duplications; lack of translocations -Some are better than others; some are worse |
|
|
When does myeloblastic syndrome typically occur?
|
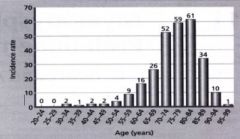
It starts showing up at around 60, peaks at 75-85
|
|
|
What are some important concepts underlying myelodysplastic syndrome classification?
|
Cell morphology
Blast percentage in the peripheral blood/marrow Cytogenetic information Different subtypes give a different prognosis |
|
|
What's the international prognosis scoring system?
|
Commonly used scoring system for MDS.
Based on blast percentage, cytopenias, and karyotype information |
|
|
People who have a higher IPSS scores show what findings?
|
Less survival
More progression to AML |
|
|
What are common causes of therapy-related MDS?
|
Alkylating agents
Radiation exposure |
|
|
What conditions are associated with alkylating agents and radiation exposure? How long do these take to develop?
|
MDS
AML 5-7 years |
|
|
What are the changes that happen in therapy-related MDS?
|
Deletion/loss of chromosome 5 and/or 7
|
|
|
What's the prognosis for therapy-related MDS?
|
Very poor; they're going to die.
|
|
|
What are the findings in chronic myelomonocytic leukemia?
|
Peripheral blood:
-Absolute monocytosis > 1E9 -BCR/ABL negative -< 20% blasts Bone marrow: -Dysplasia in 1 or more lineages - < 20% blasts |
|
|
What is 5q clinical syndrome?
|
Happens to females
70 years old Isolated macrocytic anemia; quiet. |
|
|
What is the prognosis for 5q clinical syndrome?
|
Great!
|
|
|
What are the cellular findings in 5q clinical syndrome?
|
Normal-elevated platelet counts
bone marrow erythroid hyperplasia Hypolobulated megakaryocytes |
|
|
What are the treatments for MDS?
|
Observation
Allogenic HSCT (too old, usually!) Intensive chemotherapy Supportive care/hematopoietic growth factors Immunosuppression DNA methyltransferase inhibitors IMiDs (antiapoptosis agents) Clinical trials |
|
|
How do you minimize transfusions in myelodysplastic syndrome?
|
Erythropoiesis stimulating agents
A certain subset are more likely to respond -Low endogenous EPO -Low existing transfusion requirements -Bone marrow blasts <10% |
|
|
What's the use of chelation therapy in MDS?
|
Remove the iron from MDS patients who are being transfused often
Only used in patients who have a long life expectancy, anyways. |
|
|
What are some hypomethylating agents used in MDS?
|
Azacitidine
Decitabine |
|
|
How do the hypomethylating agents work in MDS treatment?
|
Stop methylation of the chromosome --> allow transcription of important genes
|
|
|
What are indications for hypomethylating agents?
|
Transfusion dependence
Neutropenic Systemic symptoms Large blast burden |
|
|
What are the results of using hypomethyating agents in MDS?
|
50% response rate
Just prolongs life, increases quality of life |
|
|
What are the toxicities of the hypomethylating agents?
|
Infection risk
Suppression of the marrow Renal, liver toxicity |
|
|
What are indications for the immunomodulatory agents in MDS?
|
Severe disease
|
|
|
What are the special uses for immunomodulatory agents in MDS?
|
5q deletion (think the old ladies with the indolent course) --> this is very good for them!!!
|
|
|
What are the responses to the immunomodulatory agents?
|
50%
Prolong life; decrease transformation to AML |
|
|
What is the response to some of the hypomethylating drugs?
|
Very slow. You need to give the drug in 3-4 month cycles to assess responses.
|
|
|
What are the hypomethylating agents for MDS?
|
Azacitidine
Decitabine |
|
|
What are some of the the non-curative agents for myelodysplastic syndrome?
|
DNA methltransferase inhibitors
Immunomodulatory agents Chelating agents EPO stimulators All help with the symptoms secondary to MDS |
|
|
If someone has MDS, what should you do?
|
Recommend them for a clinical trial!
|

