![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Name the key growth factor for megakaryopoiesis and the primary bone marrow cell it affects
|
TPO acts on megakaryocytes in the bone marrow to increase production of platelets
|
|
|
Know the average platelet lifespan in circulation and the typical proportion of platelet mass sequestered in the spleen
|
avg platelet lifespan = 7-10 days
1/3 of platelet mass is sequestered in spleen |
|
|
Know the main structural platelet components, including dense granules, alpha granules, and phosholipids and their role in platelet plug formation
|
1. alpha granules (contain vWF, fibrinogen, factor 5, etc) - fxn mainly for adhesion/aggregation of platelets
2. dense granules (containing ADP, ATP, serotonin, Ca, etc) - fxn mainly for secretion and activation of platelets 3. phospholipid contains Phosphatidylserine on internal platelet bilayer. with activation, it gets exposed. This is responsible for increasing the activity of 10ase and prothrombin (to make thrombin). and thrombin increases fibrin product to make mature thrombus with fibrin meshwork |
|
|
what is GP Ib-IX-V role in platelet plug formation?
|
von Willebrand factor receptor: important for platelet ADHESION to the exposed subendothelial layer/collgaen
|
|
|
what is GP IIb-IIIa role in platelet plug formation
|
fibrinogen receptor: mediates platelet AGGREGATION
|
|
|
What's the general order of platelet plug formation?
|
1) adhesion (via GP Ib-IX-V)
2) activation of platelets starting with shape change - activation will activate 2b/3a as an active fibrinogen receptor for platelet aggregation - activation of platelets will release contents of granules - phospholipid will accelerate processes that increase thrombin (to form fibrin meshwork) |
|
|
Identify common contributors to acquired platelet dysfunction
|
-aspirin (#1 cause with irreversible effect)
-renal failure/liver dz |
|
|
Understand in general terms the relationship between platelet count, platelet function and bleeding risk
|
if platelet count goes down, you can't clot blood to stop bleeding and so you increase your risk of pathological bleeding
|
|
|
what types of bleeding sx's typically characterize platelet disorders?
|
mucocutaneous bleeding (menorrhagia, epistaxis, bruising (echymosis), GI bleed, hematuria
|
|
|
Know 3 mechanisms that can lead to thrombocytopenia and examples of each
|
1) increased destruction (immune-mediated, DIC, MAHA)
2) decreased production (alcohol, chemotherapy) 3) sequestration (hypersplenism) |
|
|
Recognize common treatment strategies employed for ITP and TTP
|
ITP = steroids, IVIG and anti-D Ig, TPO mimetic
TTP= plasma exchange; but DON'T DO PLATELET TRANSFUSION |
|
|
Know at least 2 thrombocytopenic conditions in which platelet transfusion is contraindicated
|
HIT(heparin induced thrombocytopenia), TTP, "ITP"
|
|
|
situation where platelet count "seems" low due to artifact of EDTA
|
pseudothrombocytopenia
|
|
|
above ______ for platelet count, you don't need to worry about bleeding problems. below it, though, you need to get concerned about UNSTOPPABLE bleeding with trauma or transfusions, etc.
|
50,000 (although nl platelet count is 150,000-400,000)
|
|
|
Ab-mediated (mainly IgG) process against your own platelets (then they get eaten up by macrophages)
|
immune thrombocytopenia (ITP) - most common ITP is in children as a response to therapy; it can be treated and does not recur afterwards)
|
|
|
name one drug that can induce ITP
|
heparin
|
|
A 40-year old school teacher notices that she can’t find words when she is working at the black board. At home she is found to be confused. In the emergency room she seems clear, but has a seizure. She is noted to have petechiae on her legs. She is post-ictal. Her CBC shows a hematocrit of 25. The white blood cells are normal. Platelet count is 25,000. The PT and PTT are normal. The BUN and creatinine are 35/2.0 and LDH is significantly elevated. Her temperature is 100.8F.
Dx? |
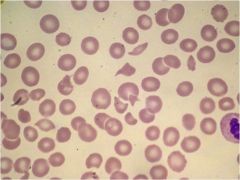
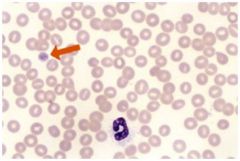
on blood smear, see hemolytic anemia-- more specifically, MAHA. shistocytes and lack of platelets.
anemia + elevated LDH + schistocytes + everything else = TTP note that pt also has neurologic findings (which is unique to TTP) |
|
|
name the 3 most important clinocal elements for diagnosing TTP!!
|
fragmentation hemolysis
thrombocytopenia elevated LDH |
|
|
what's the pathophysiology of TTP?
|
ADAMTS13 gets mutated or dysfunctional and you don’t get cleavage of vWF --> unusually large vWF --> lots of microthrombi (leading to excessive aggregation of platelets)
If large vWF multimers persist there is tendency for increased coagulation. [4] Red blood cells passing the microscopic clots are subjected to shear stress which damages their membranes, leading to intravascular hemolysis and schistocyte formation. Reduced blood flow due to thrombosis and cellular injury results in end organ damage. |
|
|
inherited thrombocytopenia that is characterized by dohle-like inclusions, macrothrombocytes
|
may-hegglin
|
|
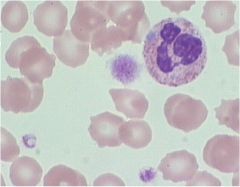
what dx?
|
abnormally large platelet with dohle body ==> may hegglin
|
|
23 year-old female c/o rash on ankles/shins and easy bruising for 10 d on her arms and sides unrelated to trauma.
On further questioning she reports nosebleeds, gum bleeding with flossing and an unusually heavy menses one week ago. She had an upper respiratory infection 3 weeks ago now resolved. Normal PE but her stool is guaiac positive. What is the most likely dx? A. Acute leukemia or lymphoma B. TTP C. Autoimmune thrombocytopenic purpura (ITP) D. Lupus E. Pseudothrombocytopenia |
C.
|
|
|
How would you treat?
A. Observation B. Platelet transfusion C. Oral steroids D. Oral steroids and IVIg E. Splenectomy |
D.
|

