![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
name the most common CLONAL hematologic disorder
|
myelodysplastic syndrome
|
|
|
if blast percentage is greater than 20%, we call that ____ _____.
|
acute leukemia
|
|
|
MDS is primarily a dz of the YOUNG/ELDERLY, with more MEN/WOMEN being affected
|
elderly; men
|
|
|
disorder/cancer that results from chromosome deletion of 5 and 7.
pathogenesis? |
MDS
a mutation in one of the HSC's will give rise to abnormal cells (clonal expansion) --> inc in production of HSC inhibitors that induce T cell mediated cell death--> inc in apoptotic cell death of marrow precursor cells (die before they get out into circulation) |
|
|
what is teh major mechanism of MDS?
|
ineffective hematopoiesis
Proliferation of progenitor and early precursor cells is normal – increased (giving a hypercellular marrow), but there is a failure to accumulate mature cells leading to the cytopenias |
|
|
what types of drugs/toxins can predispose to MDS?
|
benzene
alkylating agents topoisomerase inhibitors (chemo) |
|
|
what are the clinical manifestations of MDS (3)
|
1) anemia -weakness, fatigue
2) thrombocytopenia - bleeding, bruising 3) leukopenia - inc susceptibility to infection |
|
|
what are 3 things you expect to see in red cells in a blood smear of MDS?
|
1) basophilic stippling
2) cabot rings 3) Howell jolly: pts with splenic dysfxn |
|
|
what are 2 things you expect to see of white cells on blood smear of pt with MDS
|
1) Pseudo-pelger huet: Hyposegmentation of nucleus of neutrophil
2) Stodmeister cell: neutrophil fails to segment at all (so they have single lobe) |
|
|
T or F. micromegakaryocytes are present in MDS
|
T.
|
|
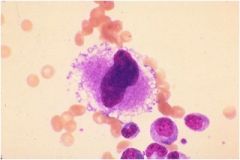
identify.
dx? |
micromegakaryocytes
may indicate MDS |
|
|
dimorphic population of rbcs, 5% blasts in marrow, risk of AML is 10% at 2 yrs
|
refractory anemia (don't tend to rapidly develop AML)
|
|
|
type of MDS characterized by ringed accumulation of iron within mitochondria (circling the nucleus)
|
refractory anemia with ringed sideroblasts (<5% blasts in marrow, rarely goes to AML)
|
|
|
type of MDS that occurs primarily in middle-aged women; characterized by macrocytic anemia and normal/increased platelet count (including megakaryocytes with hypolobulated nuclei)
|
MDS assoc with isolated deletion of chromosome 5q
|
|
|
standard tx of MDS
|
- EPO, G-CSF, GM-CSF, IL-11
- blood transfusion - deferoxamine (iron chelator) |
|
|
what do you have to be careful about with blood transfusions?
|
bewar eof excess iron, so ned to give with iron chelator)
|
|
|
what is the mechanism of action of vidaza (prodrug of decitabine)
what must you be aware of ? |
allows reactivation of silenced tumor-suppressor genes -- to decrease the proliferation of mutated cell lines
be aware of significant side effects (thrombocytopenia can be difficult to manage) |
|
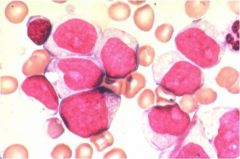
what inclusion is notable here?
dx? |
auer rod (conglomeration of granules in a blast on the way to become mature neutrophils)
acute myelogenous leukemia (AML) |
|
|
AML occurs mostly in CHILDREN/ADULTS.
|
adults
|
|
|
ALL occurs mostly in CHILDREN/ADULTS.
|
chilren
|
|
|
AML type that is assoc with t(15:17)
|
M3 acute promyelocytic leukemia (APL)
|
|
|
AML type that is assoc with inv 16
|
M4 Acute myelomonocytic leukemia
|
|
|
AML type assoc with t(8:21)
|
M2 AML with maturation
|
|
|
AML can present wiht hyperleukocytosis. why is this bad?
|
inc risk of CNS involvement...leading to leukostasis primarily affecting lungs and brains
|
|
|
what are the extramedullary dz's that can occur with AML?
|
gum infiltrates (M4/M5)
chloroma (M2) CNS chloroma: the development of multiple, malignant, localized green masses of abnormal cells, usually myeloblasts, especially beneath the periosteum of the skull, spine, and ribs. |
|
|
pt with M3 is esp at risk for what coagulopathy?
|
DIC
|
|
|
what is the most feared complication of acute leukemia
|
CNS hemorrhage in a pt with M3 (this is what kills pts early on)
|
|
|
dx of AML
|
first, bone marrow exam + biopsy
then, special stain (Wright-Giemsa, Sudan) & flow cytometry/cytogenetics |
|
|
what is the unique tx of M3 AML (acute promyelocytic leukemia)
|
ATRA (all trans retinoic acid) + chemotherapy
|
|
|
tx of AML.
name some complications of tx |
chemotherapy (complications include prolonged neutropenia/thrombocytopenia)
|
|
|
when is transplant useful for an AML pt?
|
early on after remission (don't wait for relapse)..bc youll have better outcome.
|

