![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back

what disorder is characterized by vertical interactions? what disorder is characterized by horizontal interactions?
|
vertical: hereditary spherocytosis (lose surface area)
horizontal: hereditary elliptocytosis (lose strength/elastic properties) |
|
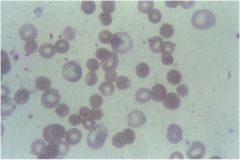
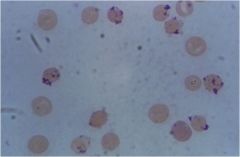
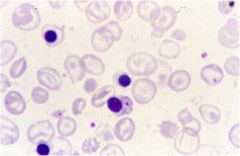
what does this pt have? what is the defect in?
|
hereditary spherocytosis; defect in ankyrin (loss of vertical connection with spectrin)
|
|
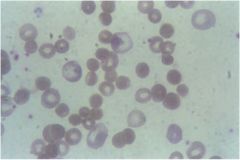
if you see a blood smear like this, could be AIHA or HS. how do you rule out AIHA?
|
by using coomb's test (it will be negative DAT) if it is HS
|
|
|
what is meant by "increased osmotic fragility" in HS?
|
where spherocytes are more likely to swell up and lyse in hypotonic solution because of its present membrane condition (can't hold any more solution in the cell)
|
|
|
tx of HS
|
folate supplementation
splenectomy |
|
|
HE is due to _____ interaction problem. more severe patients are _______ heterozygotes tha present with sever hemolytic anemia and _________. micronesian form is associated with __________.
|
horizontal; doubly; microspherocytes, splenomegaly
|
|
|
HE is MORE/LESS sever, results mainly from ____ problems.
HS is MORE/LESS severe, results mainly from _____ problems |
less; spectrin
more; ankyrin |
|
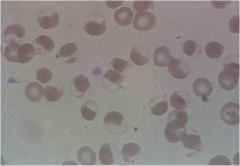
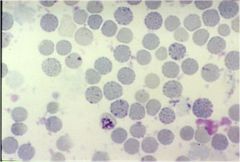
what is shown here? what is the pathophysiology?
|
"Blister" cells with chunks of degraded Hb (known as Heinz bodies)
results from deficiency of G6PD, which leads to impairment of GSH and increased oxidant stress |
|
what is shown?
|
Heinz bodies (oxidized/denatured Hb) from G6PD deficiency
|
|
what is shown?
|
Heinz bodies (oxidized/denatured Hb) from G6PD deficiency
|
|
|
why can't you take G6PD levels during a hemolytic crisis? how do you dx G6PD deficiency instead?
|
reticulocytes will give what looks like a normal G6PD level. so you have to wait 4 months to do it (life span of rbc)
dx by heinz body stain and blood smear!! |
|
|
pt gets bactrim for UTI and their Hb starts dropping like crazy, what should i be thinking?
|
oxidant hemolysis in G6PD
(bactrim and other sulfa drugs are oxidants!) |
|
|
name some other compounds that may cause oxidant hemolysis in G6PD
|
fava beans (contains divicine)
antimalarials (primaquine) bactrim nitrofurantoins methylene blue how should i memorize that?? |
|
|
which variant of G6PD is present in 12% of Afr Amer men?
|
A
|
|
|
in alpha-thalassemia:
1 gene deletion = 2 gene deletions = 3 gene deletions = 4 gene deletions = |
1 = mild microcytosis
2 = alpha thalassemia minor 3 = Hb H disease (severe microcytic, hypochromic anemia with splenomegaly; HbH can be detected in rbcs) 4 = hydrops fetalis |
|
|
alpha thalassemias result from _____ ______, while beta thalassemias result from _____ _____ that affect mRNA production.
|
gene deletions ; point mutations
|
|
|
afr american male presents with microcytic anemia.
what do you do next? he has nL Hb on electrophoresis. Dx? |
test for iron levels
if iron levels aren't low, he has a thalassemia. if Hb is nL on electrophoresis, then its alpha thalassemia minor |
|
|
pt comes in with microcytic anemia, normal iron and high HbA2 on gel electrophoresis. Dx?
|
beta thalassemia minor
|
|
|
alpha thalassemias result from _____ ______, while beta thalassemias result from _____ _____ that affect mRNA production.
|
gene deletions ; mRNA splicing defect
|
|
|
afr american male presents with microcytic anemia.
what do you do next? he has nL Hb on electrophoresis. Dx? |
test for iron levels
if iron levels aren't low, he has a thalassemia. if Hb is nL on electrophoresis, then its alpha thalassemia minor |
|
|
pt comes in with microcytic anemia, normal iron and high HbA2 on gel electrophoresis. Dx?
|
beta thalassemia minor
|
|
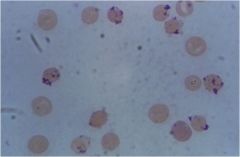
what is this showing specifically? what dz?
|
"golf balls" appearance; HbH disease (where there are 3 gene deletions in alpha thalassemia)
The crystal violet is picking up very tiny Heinz bodies which are comprised of tetramers of beta chains. |
|
|
what causes hydrops fetalis?
|
the fact that there are 4 gene deletions in alpha chain of Hb means that all the fetal Hb's will be gamma tetramer (which is extremely high in affinity for oxygen). thus, this starves the baby for oxygen and he/she is born stillborn.
|
|
|
when do beta thalassemias show up and why?
|
many weeks after delivery b/c of the gamma/beta switch post-birth... for a while, gamma's still mask the deficiency in beta chains.
|
|
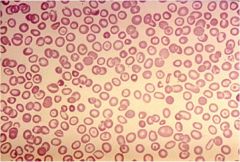
what dz is this showing?
|
beta thalassemia minor (you have one normal beta gene on a chromosome 11 and a thalassemic beta mutation on the other)
microcytic hypochromic rbc's with targeting and BASOPHILIC STIPPLING. |
|
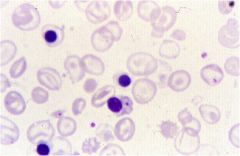
what dz?
|
beta thalassemia major (both mutations)
|
|
what dz?
|
beta thalassemia major (both mutations)
|
|

what dz is this showing?
|
beta thalassemia major (this shows marrow expansion with extramedullary hematopoiesis)
|
|
|
what one process happens to a pt with beta thal major?
|
extramedullary hematopoiesis (marrow expansion, splenomegaly
|
|
|
tx for beta thal major
|
transfusion, iron chelation, splenectomy
|

