![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
What is the most common thrombocytopenia in adults and children ? |
ITP |
|
|
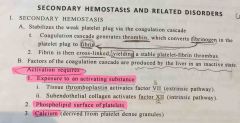
2ry Hemostasis ? |
|
|
|
What is the most common thrombocytopenia in adults and children ? |
ITP |
|
|
What is ITP ? What is the cause of ITP ? |
Autoimmune production of IgG against platelet GPIIb/IIIa by plasma cells in the spleen |
|
|
What are the Platelets disorders? |

Back (Definition) |
|
|
What is the rule of spleen in ITP ? |
1/Production of igG antibodies against GPIIb/IIIa by plasma cells in the spleen.
2/antibody pound platelets are consumed by splenic macrophages resulting in thrombocytopenia |
|
|
Types of ITP ? |
1/ acute --> children --> weeks after viral infection or immunization. Self limited and usually resolve within weeks. Response well to steroids. 2/chronic --> adults ( women of child bearing age ) --> 1ry or 2ry ( SLE ) 1st manifestation of it. May cause short lived thromcytopenia in offering since igG cross placenta. Response to steroids early but often relapse. |
|
|
What is MAHA ? |
Pathological formation of platelet microthrombi in small vessels --> platelets are consumed in the formation of microthrombi --> RBCs are sheared as they cross microthrombi --> hemolytic anemia with schistocytes |
|
|
What are the MAHA diseases ? |
HUS
TTP |
|
|
Most common inherited coagulation disorder ? |
vWF disease |
|
|
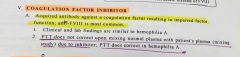
Coagulation factor inhibitors? Most common affected factor ? Diagnosis ? |
Back (Definition) |
|
|
What is vWF disease ? Presentation ? Lab ? Diagnosis ? Treatment ? |

|
|
|
Vit K affect which factors |
disco 1972 Protein C and S Factors 10, 9, 7, 2 |
|
|
Vit k function on coagulation ? |
Vit K is activated by epoxied reductase in the liver, activated vit k. Gamma carboxylates factor 10,9,7,2 and proteins C and S. Gamma carboxylation is necessary for factor function. |
|
|
How does liver failure affects coagulation ? |
1/ decrease production of coagulation factors 2/ decrease activation of vit k by epoxide reductase It is followed by PT |
|
|
How does liver failure affects coagulation ? |
1/ decrease production of coagulation factors 2/ decrease activation of vit k by epoxide reductase It is followed by PT |
|
|
How does large volume transfusion affect 2ry Hemostasis? |
Dilutes coagulation factors results in relative deficiency |
|
|
Heparin induce Thrombocytopenia? |
Development of IgG antibodies against heparin bound platelet factor 4 (PF4) __> antibody heparin PF4 complex activates platelets causing thrombosis and thrombocytopenia. |
|
|
What is Virchow triad ? |
1/ disruption of blood flow 2/endothelial cell damage 3/ HyperCoagulation |
|
|
What causes disruption of blood flow ? |
1/ immobilization 2/ cardiac wall dysfunction ( arrythmias, MI ) 3/aneurysms |
|
|
What is Hypercoagulable state ? Causes ? |
Excessive procoagulant protein and decrease anticoagulant. It could be inherited or acquired. 1/protein c or s def. 2/ factor V Leiden 3/prothrombin 20210A 4/anti-thrombin def. III 5/OCPs |
|
|
Mechanism of fibrinolysis ? |
Fibrinolysis removes thrombus after damaged vessel heals. 1/ tissue plasminogen activator (tPA) converts plasminogen to plasmin--> plasmin cleaves fibrin and serum fibrinogen , destroy coagulation factors and blocks platelet aggregation. 2/ A2-antiplasmin inactivate plasmin |
|
|
What are disorders of fibrinolysis? |
They are due to plasmin over activity :- 1) radical prostatectomy--> release of urokinase activate plasmin 2) liver cirrhosis--> reduce production of a2-anti plasmin |
|
|
What are the labs in fibrinolysis disorders ? |
Increase PT, PTT, bleeding time, normal platelet counts. Increase fibrinogen split product |
|
|
What are disorders of fibrinolysis? |
They are due to plasmin over activity :- 1) radical prostatectomy--> release of urokinase activate plasmin 2) liver cirrhosis--> reduce production of a2-anti plasmin |
|
|
What are the labs in fibrinolysis disorders ? |
Increase PT, PTT, bleeding time, normal platelet counts. Increase fibrinogen split product |
|
|
Treatment of fibrinolysis disorders ? |
Aminocaproic acid which blocks activation of plasminogen |
|
|
What are the procoagulant factors ? |
1/ TXA2 from platelets 2/decrease blood flow 3/ increase platelet aggregations |
|
|
Anti aggregation factors ? |
PGI2 NO Increase blood flow Decrease platelet aggregation Protein c Protein s Anti thrombin III |
|
|
Most common cause of Hypercoagulability in whites ? What is the cause and explain it ? |
Factor V Leiden. Mutation at the site of cleavage by protein c and s --> resistant to degradation |
|
|
Anti-thrombin III job ? Deficiency causes ? |
It is activated by heparin like molecules produced by the endothelium. Then ATIII inactivate thrombin and coagulation factor. Deficiency causes HyperCoagulation. |
|
|
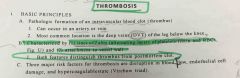
Thrombosis vs post mortem clot ?? |
Back (Definition) |
|
|
What is Virchow triad ? |
1/ disruption of blood flow 2/endothelial cell damage 3/ HyperCoagulation |
|
|
What causes disruption of blood flow ? |
1/ immobilization 2/ cardiac wall dysfunction ( arrythmias, MI ) 3/aneurysms |
|
|
How does endothelium prevent thrombosis ?? |
1/ block the subendothelial collagen and underlying tissue factor 2/ produce and secret: 1. Prostacyclin ( prostaglandin I2) 2. NO Both vasodilate and inhibitor platelet aggregation 3. Heparin like molecule --> augment ATIII which inactivates thrombin and coagulation factors 4. tPA ( converts plasminogen to plasmin) 5.thrombomodulin --> redirect thrombin to activated protein C which inactivates factor V & VIII |
|
|
Causes of endothelial damage ? |
Atherosclerosis Vasculitis High levels of homocysteine ( vit B12, folate def. or cyststhionine beta synthase def. ) |
|
|
What is cyststhionine beta synthase deficiency ? And what are the consequences of it ? |
It converts homocysteine to cyststhionine. If it is deficient then lead to build up of homocysteine and homocysteinuria--> 1/ vessel thrombosis 2/mental retardation 3/lens dislocation 4/ long slender fingers |
|
|
HUS vs TTP ? |

Back (Definition) |
|
|
Cyststhionine beta synthase def ?? |

Back (Definition) |
|
|
Which hormone increase the production of coagulation factors ? |
Estrogen |
|
|
Causes of fat embolism ? And what is the characteristics of it ? What is composed of ? |
1/ bone fracture (specially long) while fracture is still present or shortly after repair.
2/ soft tissue trauma.
Characterized by dyspnea and petechia r on the skin overlying the chest
The emboli have fat and bone marrow elements. |
|
|
What are the cases of gas embolism ? |
1) decompression sickness [ joint and muscle pain " bends" and respiratory symptoms "chokes"]
2)laparoscopic surgeries |
|
|
What is the composition of emboli ? |
Cholesterol cleft in it |
|
|
What is the composition of amniotic fluid embolus and what is the symptoms of it ? |
Composed of squamous cells, keratin debris from fetal skin.
Present with Sob, DIC and neurological symptoms |
|
|
Why is most of PE's are Asymptomatic ? |
1/ dual blood supply of the lung 2/ the emboli usually small --> self resolves. |
|
|
When does Pulmonary infarction happen in PE ? |
If a large or medium sized artery is obstructed in pts with pre-existing cardiopulmonary compromise; only 10% of PEs cause infarction |
|
|
What causes sudden death from PE ? |
Large saddle embolus that blocks both left and right pulmonary arteries OR significant occlusion of a large pulmonary artery. Death usually due to electromechanical dissociation. |
|
|
What may arise from chronic emboli ? |
When they reorganized over time they may cause pulmonary HTN. |
|
|
Systemic embolism where due they arise from ? |
Left heart |

