![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
73 Cards in this Set
- Front
- Back
|
What is a simplified definition of heart failure (think Nichols) and explain the pathway.
|
Heart failure = pump failure --> inadequate perfusion --> not enough blood where it needs to be--> inadequately pumped blood backs up (not enough where it needs to be/too much where it is not needed)
|
|
|
What are the symptoms of heart failure?
|
Symptoms associated with inadequate perfusion or those associated with blood backup under pressure with fluid transudation
Increased pulmonary venous pressure |
|
|
What does increased pulmonary venous pressure cause even before transudation of fluid into the lungs?
|
Dyspnea
|
|
|
What cause central venous pressure to increase and what causes it to decrease?
|
Increase = volume overload
Decrease = volume depletion |
|
|
True or false. There is a wide range of normal volumes and pressures.
|
True
|
|
|
What is the normal range of central venous pressure?
Thus, what is the average of normal central venous pressure (CVP)? |
2-8 mm Hg
6 mm Hg |
|
|
How do you determine CVP?
|
Physical examination
Tip of central venous catheter in superior vena cava |
|
|
A CHF patient has a CVP of 5. How do you determine if this was an increase or a decrease from normal?
|
Given bolus of fluid, if number goes up and stays up, volume depletion is not the problem. If number goes up then drops again, patient may have heart failure and volume depletion.
|
|
|
What could volume depletion be due to?
|
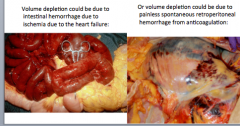
Intestinal hemorrhage due to ischemia due to heart failure.
Also painless spontaneous retroperitoneal hemorrhage from anticoagulation. |
|
|
What are the equations relating stroke volume and end volumes?
|
SV = LVEDV-LVESV
LVESV = LVEDV-SV |
|
|
What is the normal value range for LVEDP?
|
4mm Hg --> 12 mm Hg
Use 10 mm Hg as average or "normal" |
|
|
What are the normal LVEDV ranges?
|
65 ml --> 240 mL
Use 120 mL as normal (we use 150 mL in calculations) |
|
|
What is the normal stroke volume range?
|
55 mL --> 100 mL
Use 70 mL for normal (but we use 100 mL in teaching calculations) |
|
|
What are the normal EF ranges?
|
50% --> 75%
60% is an average of normal, but use 67% (2/3) for teaching. |
|
|
What are normal LVESV ranges?
|
15 mL --> 145 mL
Use 50 mL as normal LVESV |
|
|
What would be the change in these components from a normal heart to a failing heart (increase or decrease)
LVEDP LVEDV SV EF LVESV |
LVEDP = increase
LVEDV = increase SV = decrease EF = decrease LVESV = increase Think of a DILATED CM in heart failure. |
|
|
What is the initial symptom of heart failure? When is it observed?
|
Dyspnea
With exertion |
|
|
True or false.
Most heat failure patients only exhibit failure on one side? |
False!
Most have both left and right heart failure |
|
|
What is the threshold for heart failure when patients begin to exhibit symptoms (think stroke volume)?
|
25% reduction in forward stroke volume
|
|
|
What does sever acute uncompensated aortic regurgitation require?
|
Emergency surgery!
|
|
|
True or false. Mitral valve regurgitation can either be a cause of heart failure or an effect of it.
|
True
|
|
|
What type of murmur does mitral regurgitation cause?
What type of murmur does mitral stenosis cause? |
Systolic murmur (ventricular pumping)
Diastole |
|
|
Aortic regurgitation causes a murmur during what?
When does aortic stenosis cause a murmur? |
Diastole
Systole |
|
|
What are four symptoms of left heart failure?
|
1. Dyspnea on exertion --> dyspnea at rest
2. Orthopnea (shortness of breath when lying flat) 3. PND (paroxysmal nocturnal dyspnea) 4. Fatigue *JUST THINK TIRED AND CAN'T BREATHE! |
|
|
What are two symptoms of right heart failure?
|
1. Edema of feet, ankles, legs
2. Abdominal distention |
|
|
What are signs of left heart failure? (4)
|
1. Bibasilar pulmonary crackles
2. Tachycardia 3. S3 4. Pedal, ankle, or leg edema (by different mechanism than right sided) |
|
|
What are the signs of right heart failure?
|
1. Pedal, ankle, or leg edema
2. Jugular venous distention 3. Hepatomegaly 4. Ascites (fluid accumulation in abdominal cavity) *JUST THINK EVERYTHING BELOW THE HEART GETS FULL OF WATER (the backed up pressure) |
|
|
What is the pathophysiologic mechanism of edema?
LEFT SIDED HEART FAILURE |
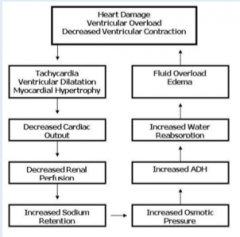
Draw this out!
|
|
|
Left heart failure causes pulmonary edema by causing a buildup of ___________ in the _________, _________, __________ and eventually the __________.
|
Pressure
Left ventricle --> left atrium --> pulmonary veins --> pulmonary capillaries |
|
|
At what pulmonary capillary pressure does fluid start to transudate out of them into the interstitium causing interstitial pulmonary edema?
|
20 mm Hg (about double that of normal)
|
|
|
At what pulmonary capillary pressure does fluid start to transudate out into the alveoli causing alveolar pulmonary edema?
What is this associated with? What can also cause alveolar edema? |
25 mm Hg
Wet moist crackles Acute lung injury |
|
|
What two things can cause acute pulmonary injury? How can you ell them apart?
|
Septic shock = normal pulmonary capillary pressure
Hemorrhagic shock = low pulmonary capillary pressure |
|
|
How do you measure pulmonary capillary pressure?
What is this technique called? |
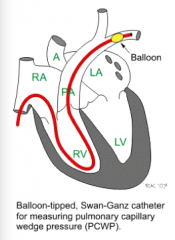
Pass a catheter with pressure monitor through SVC, right atrium, right ventricle, and pulmonary artery until it is wedged into the smallest artery it will fit into --> inflate balloon and measure pressure
Swan-Ganz catheterization |
|
|
What is the pulmonary capillary wedge pressure approximately the same as?
What else can t measure? |
Left atrial pressure and left ventricular end diastolic pressure
Mixed venous O2 sat and cardiac output |
|
|
Most common signs and symptoms of heart failure?
|
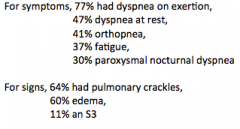
Appreciate the order.
|
|

Label each.
|
Top = systolic heart failure
Middle = normal Bottom = diastolic heart failure |
|
|
What is associated with systolic heart failure?
|
Many elderly patients develop heart failure with dyspnea, orthopnea, PND and bibasilar pulmonary crackles, but HAVE A NORMAL OR NEAR NORMAL EJECTION FRACTION!
� |
|
|
What is associated with normal heart failure?
|
Long-standing hypertension, often with obesity, and concentric left ventricular hypertrophy.
� |
|
|
What is associated with diastolic heart failure?
Another name? |
Noncompliant stiff left ventricles with impaired diastolic function and filling
Heart failure with preserved ejection fraction. |
|
|
Why do heart failure patients have tachycardia?
|
1. SNS
2. E and NE from adrenal |
|
|
Why do HF patients have elevated B-type natriuretic peptide? What does it do?
|
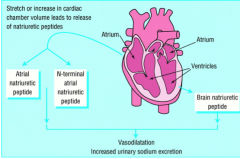
Vasodilation
Increased urinary sodium excretion |
|
|
True or false.
B-type natriuretic peptide (BNP) is counterregulatory. |
TRUE!
|
|
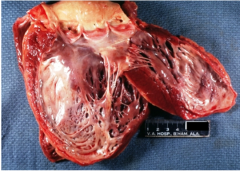
If the patient died and came to autopsy, his heart would likely have this gross pathology. Can you describe and diagnose it?
� |
erwerw
|
|

The condition shown in the previous image can be complicated by the condition shown here; what is it?
Risk of what further complication? |
Mural thrombus formation
Embolization |
|
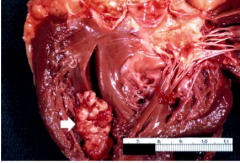
What is this?
Why did it form? Will it embolize? Why or why not? |
Mural thrombus
Myocardial infarction (compare upper and lower wall) Not likely because it is organizing |
|
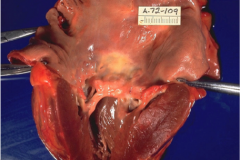
She has this condition; can you describe and diagnose it?
|
The mitral valve is severely thickened and fibrotic, with shortened and fused chordae tendineae, and the left atrium is severely dilated.
Rheumatic mitral stenosis! |
|

What is this?
|
Cardiac apex = best place to hear mitral valve murmurs
|
|
|
Do most patients with cor pulmonale have heart failure?
Why do many more patients with right heart failure? |
No, they are compensated
Because of left heart failure, NOT cor pulmonale Only a small group of patients with right heart failure due to cor pulmonale |
|
|
ksdjlfksd
|
Atherosclerosis
|
|
|
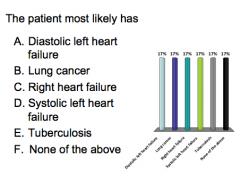
An 80-year-old white male has a history of smoking, hypertension, obesity, diabetes and dyslipidemia.
He presents with increasing dyspnea on exertion, paroxysmal nocturnal dyspnea and 2-pillow orthopnea. Diagnosis? |
Heart failure
|
|
|
An 80-year-old white male has a history of smoking, hypertension, obesity, diabetes and dyslipidemia. He presents with increasing dyspnea on exertion, paroxysmal nocturnal dyspnea and 2-pillow orthopnea.
His temperature is 37, heart rate 110, blood pressure 110/70, respirations 20 and saturation 95%. He has a third heart sound, but no murmurs. He has pulmonary crackles at both lung bases. His abdomen is soft and non-tender. He has leg edema up to the knees. Diagnosis? |
Heart failure
|
|
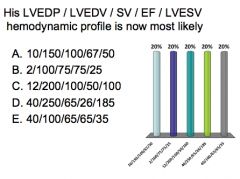
Let’s assume that when his heart was healthy, years ago, his left ventricular end diastolic pressure (LVEDP) was 10 mm Hg and end diastolic volume (LVEDV) was 150 ml, of which his left ventricle ejected two-thirds with each heartbeat, making his stroke volume (SV) 100 ml and ejection fraction (EF) 67%, leaving 50 ml behind, his left ventricular end systolic volume (LVESV).
� |
Answer option D has a markedly elevated LVEDP
of 40 mm Hg, markedly elevated LVEDV of 250 ml, of which only 65 ml (SV) is ejected for an ejection fraction (EF) of 26%, leaving behind a very large amount of blood at the end of systole (LVESV 185 ml), which be associated with left ventricular dilatation, but do not jump the gun before you consider the last option. |
|
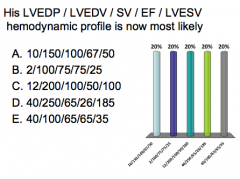
What is B associated with?
|
Answer option B has an LVEDP of 2 mm Hg and
LVEDV of 100 ml, both lower than his previous baseline, of which 3/4 is ejected (EF 75%), leaving only 25 ml behind (LVESV). This would fit much better with the clinical scenario of someone with a normal heart and severe acute blood volume loss without time to pull in fluid to compensate. |
|
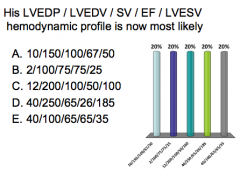
What is C associated with?
|
Answer option C has a slightly higher LVEDP of
12 mm Hg and doubled LVEDV of 200 ml, of which half is ejected (EF 50%), but that amount (SV 100 ml) is the same as his previous normal baseline; this would be compensated heart failure. |
|
|
What is E associated with?
|
Answer option E has the same high LVEDP of
40 mm Hg, but low LVEDV of 100 ml, of which 65% is ejected, leaving 35 ml behind (LVESV). This would fit much better with the clinical scenario of someone with a stiff noncompliant heart and impaired diastolic filling |
|
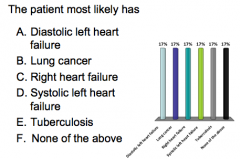
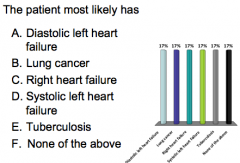
50-year-old black male with a history of smoking, gradually progressive dyspnea, dry cough over the
past 4 years, and leg edema for the past 2 months. No orthopnea or paroxysmal nocturnal dyspnea. Temperature is 37, HR 90, BP 90/70, respirations 30 and saturation 89%. Hands and feet are cool to the touch. He has jugular venous distension, diffuse dry pulmonary crackles, abdominal distension with hepatomegaly and ascites, and leg edema up to the knees. |
None of the above! Left heart failure (most common cause of right heart failure)
|
|
|
Jugular venous distention, hepatomegaly, ascites, and leg edema are classic findings of what?
|
Right heart failure
|
|
|
Patients with cor pulmonale often have dyspnea. What is the dyspnea from?
|
Lung disease that caused heart failure, not the other way around.
|
|
|
Pulmonary crackles could be from what?
|
Idiopathic interstitial lung disease --> pulmonary hypertension --> cor pulmonale
|
|
|
One thing that distinguishes right heart failure due to cor pulmonale from right heart failure due to left heart failure is that patients with cor pulmonale do not get orthopnea or paroxysmal nocturnal dyspnea; why not?
� |
Orthopnea and paroxysmal nocturnal dyspnea from exacerbation of left heart failure from the increase in venous return from being recumbent.
If pulmonary hypertension is causing the right heart to fail, it does not pump that extra venous return to the left heart. |
|
A 30-year-old south Asian female with increasingly disabling dyspnea on exertion, fatigue, palpitations and recent episodes of mild hemoptysis.
Her temperature is 37, heart rate 90, blood pressure 110/70, respirations 20 and saturation 97%. Her pulse is irregular. On cardiac auscultation, she has an opening snap and a grade III/VI diastolic rumbling murmur. She has no pulmonary crackles. Her abdomen is not distended and not tender. She has no peripheral edema. |
Mitral stenosis
=diastolic murmur, opening snap sometimes No left heart failure findings (wet pulmonary crackles) No right heart failure findings (jugular venous distention, hepatomegaly, ascites and lower edema) |
|
A 30-year-old black female food service
worker presents with increasingly disabling dyspnea on exertion, palpitations, orthopnea and paroxysmal nocturnal dyspnea, 3 months after she had her third child. Her temperature is 37, heart rate 110, blood pressure 110/70, respirations 30 and saturation 92%. Her skin is warm. On auscultation, she has an S3 third heart sound and bibasilar wet pulmonary crackles. Her abdomen is mildly distended, but not tender. She has no peripheral edema. |
Systolic left heart failure.
|
|
|
What are classic symptoms of systolic left heart failure?
What caused her to have low sodium? What percent of heart failure patients have this? |
Dyspnea on exertion, orthopnea, and paroxysmal noctural dyspnea
Actually retaining more water than sodium --> dilution Syndrome of SIADH (antidiuretic hormone) 25% |
|
|
Why do people get heart failure following pregnancy?
Peripartum cardiomyopathy |
Unknown
Cardiac angiogenic imbalances from complex pregnancy-related immune system and hormonal changes play a role |
|
|
Does heart failure lead to pro-inflammatory cytokine profile?
|
Yes!
TNF, IL-1, and IL-6 |
|
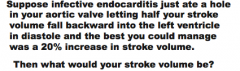
What would it be?
What would your forward stroke volume be? Would you have heart failure? |
120 mL (assuming 100 mL baseline)
60 mL Yep! |
|
|
What is the average normal EDV?
What amount is left over from last systole? What amount left from atrium? Now, with your acute aortic regurgitation, it is 170 ml (50 ml end-systolic, 60 ml back from the aorta and only 60 ml from left atrium instead of 100 ml). Where is the missing 40 ml? |
150 mL
50 mL 100 mL Not being returned from the body. |
|
|
True or false.
Severe acute uncompensated aortic regurgitation is a surgical emergency. |
TRUE!
|
|
|
You are a heart valve with a chronic mitral valve regurgitation of 95 mL. How do you cope?
|
1. Increased stroke volume
2. Increased end-diastolic volume 3. Left ventricular dilatation |
|
|
Suppose the best you could do is double normal stroke volume and 90 mL extra end diastolic volume. What would these be?
Will that be enough to avoid heart failure? |
EDV = 240 mL
Stroke volume = 200 mL Yes = forward stroke can fall 30 mL before getting heart failure. |
|
|
You are a heart with a mitral valve prolapse. Rupture of chordae have just caused acute regurgitation of 70 mL. How can you cope?
|
1. Increased stroke volume
2. Increased end-diastolic volume |
|
|
Suppose the best you can do is 40% more stroke volume and 13% more end-diastolic volume. What will these be?
Will that be enough to avoid heart failure? |
EDV = 170 mL
SV = 140 mL Probably no, if your baseline had been 100 mL, because only 70 mL is going forward. |
|
|
What is the threshold for reduction in forward stroke volume that will cause heart failure (when patients begin to have symptoms)?
|
25% reduction in forward stroke volume
|

