![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back
|
What is the clinical scenario for heart failure with "preserved ejection fraction?"
|

Elderly patient
Long-standing hypertension (with obesity) and concentric left ventricular hypertrophy now with impaired compliance Bulking up for years and years against excess afterload until compliance finally gives way. |
|
|
What is the pathway to systolic dysfunction heart failure with decreased ejection?
|
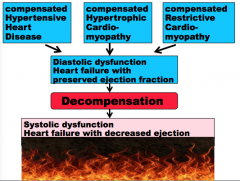
Draw it!
|
|
|
What is the spectrum of patients with heart failure?
|
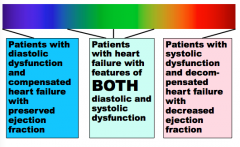
Draw it.
|
|
|
True or false. Patients with large myocardial infarctions go straight to heart failure with systolic dysfunction and decreases ejection fraction.
|
True! (they do not go through a phase of diastolic dysfunction, heart failure with preserved ejection fraction)
|
|
|
What are the four classifications for acute heart failure hemodynamics?
What percentage of each die? |
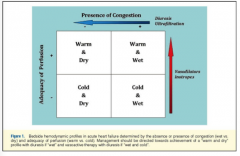
Warm and dry (10%)
Warm and wet Cold and dry Cold and wet (40%) Warm = perfusion, cold = low perfusion Dry = no pulmonary edema, wet = pulmonary edema |
|
|
What are the three general principles of heart failure?
|
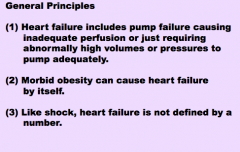
From the slide.
|
|
|
What can septic, cardiogenic, and hypovolemic shock be classified as?
Common effects of each? |
Distributive shock
Vasodilation (capacitance too big for amount of blood available) |
|
|
What is a cause of cardiogenic shock?
What is a cause of obstructive shock? |
1. Large pulmonary thromboembolus blocking pulmonary circulation
2. Hemopericardium causing cardiac tamponade |
|
Label each.
|
Distributive shock --> Hypovolemic shock --> Cardiogenic shock --> Obstructive shock
|
|
|
What is the most common type of shock? Least common?
|
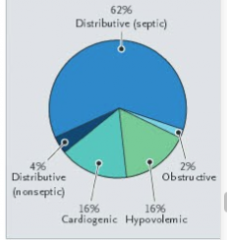
Common = distributive
Least = Obstructive |
|
|
What three things is the diagnosis of shock based on?
|
Clinical, hemodynamic, and biochemical signs.
|
|
|
What is the biochemical sign of shock?
|
Elevated serum lactate from anaerobic metabolism required because the body is inadequately perfused
|
|
|
What are the hemodynamic signs of shock?
|
Hypotension (different for each patient)
|
|
|
The clinical signs of shock are observed through which three windows of the body?
|
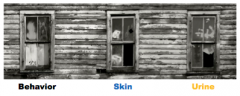
Behavior, skin, urine
|
|
|
What are behaviors that can be observed (clinical windown #1) in shock?
|
Disorientation, confusion, obtundation (decreased level of alertness)
|
|
|
What are the skin changes that can be observed in shock (clinical window #2)
|
Mottled, cold, clammy, pale, or cyanotic
|
|
|
What are unine changes that can be observed in shock (clinical window #3)?
|
Decreased output
|
|
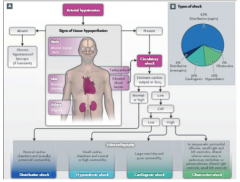
We should probably know this slide.
|
Draw it!
|
|
Aortic regurgitation due to severe dilatation of aortic root.
Name and describe the microscopic pathology indicated by arrow. Can you name the disease that would cause this? |
|
|

Why does she have mitral regurgitation? What is the reason?
|

Ruptured papillary muscle
|
|
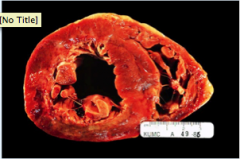
Why does she have a ruptured papillary muscle? Here is the reason. Can you find it, describe and diagnose it?
|
1. Posterior left ventricle
2. Area of mottled tan, red, light, and dark brown myocardium 3. Acute MI |
|
|
A 90-year-old white male has a history of an old myocardial infarction. He presents with increasingly disabling dyspnea on exertion, waking up short of breath and needing three pillows to prop him up for sleep.
His temperature is 37, heart rate 110, blood pressure 110/70, respirations 20 and saturation 95%. He has a third heart sound, but no murmurs. He has pulmonary crackles one-third of the way up his back bilaterally. His abdomen is distended, but not tender. He has leg edema up to the knees. Why does he have leg edema? |
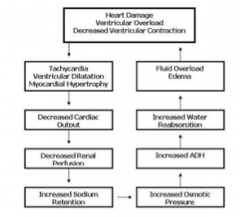
This is why?
� |
|
|
Why does he have tachycardia?
|
Sympathetic nervous stimulation
Epinephrine & norepinephrine from adrenals |
|
|
Why does he have pulmonary crackles?
|
Pulmonary alveolar edema
|
|
|
Why does he have pulmonary alveolar edema?
|
Hydrostatic pressure buildup from the excess blood the left heart is failing to pump, being transmitted back to the pulmonary capillaries, which are leaking fluid transudate into alveoli.
� |
|
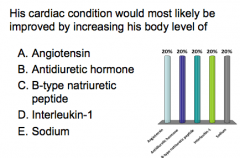
What is the answer?
|
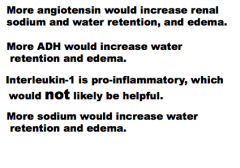
B-type natriuretic peptide
|
|
|
Which hormone opposed what the other hormones are doing in heart failure?
What is an excellent blood test for heart failure? |
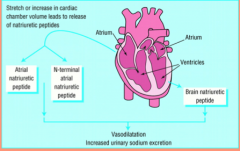
ANP
B-type natriuretic peptide (BNP) levels |
|
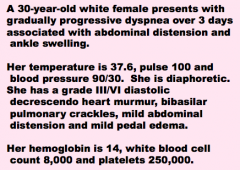
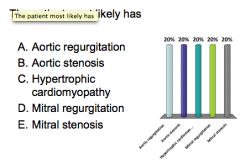
What do you think the patient has?
|
Ankle swelling + pulmonary crackles = heart failure
Diastolic murmur = valve disease (NO INNOCENT DIASTOLIC MURMURS) AORTIC REGURGITATION! |
|
Let’s assume that her baseline left ventricular
end-diastolic pressure (LVEDP) was 10 mm Hg. Assume her baseline left ventricular end-diastolic volume (LVEDV) was 150 ml. Assume her stroke volume (SV) was 100 ml. That would make her ejection fraction (EF) 67% It would make her left ventricular end-systolic volume (LVESV) 50 ml. Make sure the numbers reflect heart failure also! |
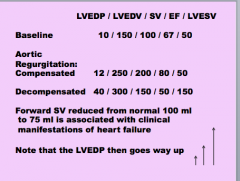
Only been three days, so regurge is not compensated.
E |
|
|
Marfan Syndrome:
What is defective? |
Defective synthesis of fibrillin --> abnormal sequestration of TGF-B in aortic wall --> dilation due to dysregulated signaling and progressive loss of elastic tissues
|
|
|
What does Marfan's syndrome lead to?
|
Inadequate extracellular matrix synthesis and accumulation of increasing amounts of amorphous proteoglycans --> cystic medial degeneration
Can also occur in scurvy. |
|
A 60-year-old obese white female smoker with diabetes (for 30 years), hypertension and hypercholesterolemia presents with rapidly progressive dyspnea over 3 hours associated with abdominal distension and ankle swelling.
Her temperature is 37.6, pulse 100 and blood pressure 90/30. She is diaphoretic. She has a grade III/VI blowing holosytolic heart murmur, bibasilar pulmonary crackles, mild abdominal distension and mild pedal edema. |
Mitral regurgication
Not aortic stenosis (female and wrong type of murmur quality) |
|
|
She had an MI that led to papillary rupture and mitral regurgitation. Why didn't she have chest pain?
|
Silent myocardial infarctions
More common in diabetics, usually involves about 10% of LV |
|
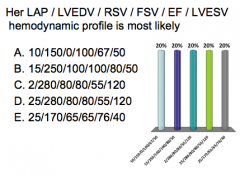
Let’s assume that her baseline left atrial pressure (LAP) was 10 mm Hg. Assume her baseline left ventricular end-diastolic volume (LVEDV) was 150 ml. Assume her stroke volume (SV) was 100 ml. That would make her ejection fraction (EF) 67% It would make her left ventricular end-systolic volume (LVESV) 50 ml. Now, with her mitral regurgitation and heart
failure, her stroke volume is partly going in reverse back into the left atrium (RSV) and partly going forward (FSV). Since there are 2 papillary muscles and she has lost one, let’s assume half of her SV is RSV…� |
E
Acute myocardial regurgitation = Elevated atrial pressure, decreased LVESV with part of stroke volume going backward Chronic = less elevated left atrial pressure, more increased LVEDV to compensate for stroke volume reverse --> higher than normal LVESV at the end of systole |
|
|
What happens when chronic mitral regurgitation passes limit of compensation and becomes decompensated?
|
Hemodynamics take on bad features of acute and chronic mitral regurgitation:
LAP increases LVEDV really high LVESV increase way up (because decompensated heart can't pump out so much) --> FORWARD STROKE VOLUME FALLS |

