![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
what is the dominant artery? what does that mean
|
85% right dominant: Right coronary artery gives rise the posterior descending artery perfusing the posterior 1/3 of the septum
the "dominant" artery perfuses the posterior 1/3 of the septum |
|
|
|
what is the direction of blood flow in the myocardium
|
from epicardium to endocardium
|
|
|
|
when does blood flow in the heart myocardium
|
mainly during diastole
|
|
|
|
when the unobstructed vessel dilates, how much can it increase its flow
|
8 times
|
|
|
|
What is myocardial ischemia
|
it is an imbalance of supply (perfusion) and demand (increased need for oxygenated blood)
|
|
|
|
what causes 90% of the cases of IHD
|
IHD is secondary to decreased blood flow through the coronary arteries because of atherosclerotic dz
(other causes are anemia, blood loss, Anemia chronic dz) |
|
|
|
what are the causes of decreased oxygen supply
|
coronary artery occlusion
anemia (ACD, blood loss, trauma) Pulmonary dz/hypoxemia tachycardia |
|
|
|
what are the causes of increase oxygen demand
|
tachycardia
left ventricular hypertrophy HTN (HTN pregnancy) anything that increases cardiac work/wall tension physical exertion, emotional excitment |
|
|
|
What are the 4 clinical syndromes of IHD
|
1. MI
2. Angina Pectoris 3. Chronic IHD with Heart failure 4. acute coronary syndromes |
|
|
|
what are acute coronary syndromes
|
- unstable angina -->MI-->sudden death
-abrupt and unpredictable conversion of stable AS plaque to unstable lesion (erosion, rupture, hemorrhage, superimposed thrombosis) -plaque disruption/acute plaque changes =one of the most common causes |
|
|
|
What are the epidemiology facts regarding IHD?
how many deaths/yr, why is incidence decreaseing |
-leading cause of death in men& women in US
-500,000 deaths per year - incidence is decreasing due to better tx, increased awareness, and prevention via risk factor modification (dec diabetes & smoking) |
|
|
|
What are the 6 items listed for the pathogenesis of IHD
|
1. fixed coronary obstruction
2. plaque morphology 3. acute plaque changes 4. inflammation 5. thrombosis 6. vasoconstriction |
|
|
|
Describe fixed coronary obstruction
|
75% or greater decresase in reduction in the cross sectional area of the coronary artery
symptoms will occur with exertion IF >90% obstruction symptoms will occur at rest |
|
|
|
Why is plaque morphology important
|
Vulnerable plaques - larger lipid laeden center with thinner fibrous caps
|
|
|
|
What are the acute plaque changes
|
rupture/fissue
erosion/ulceration hemorrhage |
|
|
|
What acute phase reactant is involved in the inflammatory pathogenesis of IHD
|
CRP - it is a marker in the serum produced by the liver.
It is secreted from cells within the AS intima -->activates local endothelial cells-->inc adhesiveness of leukocytes & induces prothrombotic state |
|
|
|
what is the common pathophysiological basis that the acute coronary syndromes(acute MI, angina, sudden death) share
|
coronary atherosclerotic plaque disruption and resulting intraluminal thrombus formation
|
|
|
|
Describe Angina
|
chest pain associated with transient myocardia ischemia (pain <15min, if >20 GO TO ER)
paroxysmal & recurrent attacks precordial discomfort/pain "squeezing, choking, constricting" stable and unstable types |
|
|
|
What is the most common form of angina? describe the cause and relief
|
Stable Angina = fixed severe stenosis but no plaque disruption
brought on by exertion, not changing in frequency, duration or inciting factors relieved by rest or vasodilators |
|
|
|
What is the pattern, cause, and relief for unstable angina
|
it is preinfarction angina (prodrome for MI) caused by intermitten platelet aggregation
GREATLY increased risk probability of thrombosis/acuteMI it changes in pattern, frequency, severity = "crescendo angina" |
|
|
|
What is prinzmetal angina?
|
it is a variant angina secondary to vasospasm, usually without fixed coronary stenosis
it responds to vasodilators |
|
|
|
What are the exam findings in prinzmetal angina
|
pt has episodic chest pain, occurs at rest.
may see elevated ST segments on ECG circulating adrenergic agonists |
|
|
|
What defines Sudden Death
|
unexpected death from cardiac causes
death with in a hour of the onset of symptoms |
|
|
|
What is the most common cause of Sudden Death
|
Ischemia is the most common cuase of sudden death
|
|
|
|
What are the non- AS cuases of sudden death
|
electrolyte derangements, valvular dz, HOCM, myocarditis, conduction disorders
|
|
|
|
In adults what are for common associations with sudden death
|
usually associated with severe CAD, often 2 or 3 vessle dz, an arrythmia, thrombus may NOT be demonstrable,
|
|
|
|
What is the definition of an acute MI
|
death of cardiac muscle resulting from ischemia
it is the leading cause of death in the US -->1.5 million suffer an MI annually |
|
|
|
What are the risk factors
|
Old age
HTN smoking diabetes hyperlipidemias (esp hyperchol) male gender |
|
|
|
What are the sequemtial effects of ischemia
|
ATP depletion (seconds)
Loss of contractility (2 min) ATP depleted (40-50 min) IRREVERSIBLE INJURY(20-40 min) microvascular injry (hours) |
|
|
|
how can you stop the injury
|
reperfuse within 20 can stop the injury
|
|
|
|
what is layer of the myocardium is most affected by an MI
|
endocardial >>>epicardial
|
|
|
|
where do most transmural infarcts involve
|
almost all involve the LV, up to 30% involve the RV
|
|
|
|
What is the frequency of each vessel in an MI?
-LAD -RCA -L Circ |
-LAD = 40-50%
-RCA = 30-40% -L Circ = 15-20% |
|
|

describe the pathology
|
TTC staining at 2-3 hours - stains normal myocardium red and infarcted myocardium pale
**since he stated no one uses this I would put a star by and assume it will be on the test Now describe the gross morphology at <12 hrs 12-14 hrs 10days+ weeks |
<12 hrs: inapparent unles ttc stain
12-14 hrs: hyperemic red blue hue 10days+: sharply defined yellow tan, soft region with hyperemic border (=highly vasc granulation tix) weeks: fibrous scar |
|
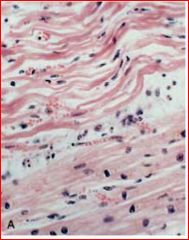
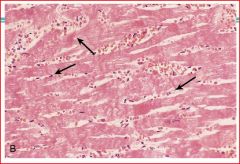
describe the pathology and time point
|
4-12 hours: wavy fibers followed by changes of coagulation necrosis
-myocytolysis: vacuolization of myocytes at infarct margins, potentially reversible esp in subendocardial zone |
|
|
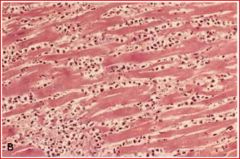
describe pathology and time point
|
3 days - acute inflammation most prominent; no nuclei present, dense neutrophils attacking tissue
|
|
|
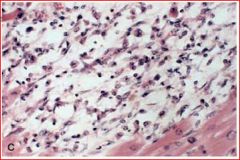
describe pathololgy and time point
|
7-10 days: macrophages removing necrotic tissue
macrophages with clear cytoplasm |
|
|
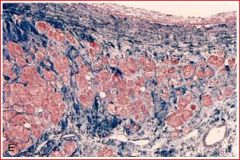
describe pathology and time point
|
weeks: red = residual myocytes, blue = dense fibrosis
2-4 weeks = granulation tissue eventually replaced by fibrosis 6-8 weeks: fully fibrotic |
|
|
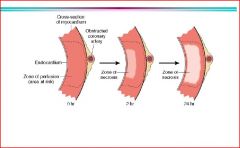
figure
|
wave of injury = from the subendocardial progressing to transmural
* note endocardial zone prefused directly from blood in atria |
|
|
|
when is highest risk off rupture
|
3-7(or10) days - present with pulseless paradoxus, distant heart sounds, and heart failure = cardiac tamponade
|
|
|
|
what is the goal of reperfusion
|
an attempt to restore perfusion quickly to salvage ischemic myocardium
|
|
|
|
what are ways to reperfuse myocardium
|
thrombolysis therapy, ballon angioplasty, PTCA
|
|
|
|
what is the time frame for reperfusion
|
with in 20 minutes, can salvage everything; decreasing proportion with increasing time
|
|
|
|
How does an infarct with reperfusion appear and why
|
it appears hemorrhagic in appearance owing to leakage from injured vasculature
-contraction band necrosis -hypercontracted sarcomeres |
|
|
|
Why does a small amount of new damage occur after reperfusion
|
free radical mediated
|
|
|
|
What may persist despite reperfusion
|
stunned myocardium = function changes may persist despite reperfusion.
- not completely dead, after recovers, heart function improves after a few days |
|
|

describe the pathology
|
reperfused myocardium
|
|
|
describe the pathology
|
contraction bands = no nuclei
|
|
|
|
what are clinical findings with an MI
|
rapid weak pulse, diaphoresis, crushing chest pain, dyspnea, nausea
**Diabetics often have silent MI |
|
|
|
What do you normally see on ECG
|
ST elevation
Q wave - transmural non-Q wave - subendocardial |
|
|
|
what molecules would you want to measure, that leak out of damaged myocardium
|
myoglobin, troponin T & I, CKMB, LDH
|
|
|
|
Prognosis of MI
|
death - 1/2 are with in 1 hr
poor prognosis = advanced age, female,diabetic, previous MI 3/4 will have a complication post MI |
|
|
|
What are the complications of a MI
|
contractile dysfuncion;/pump failure
arrythmia myocardial rupture pericarditis RV infarction infarct expansion/extension mural thrombus -->stroke ventricular aneurysm papillary muscle dysfunction/rupture progressive late heart failure (chronic ICD-->fibrotic scars) |
|
|
|
what are the consequences of myocardial rupture
|
free wall rupture = 7-10 days, hemopericardium and tamponade
septal rupture = L-->R shunt papillary muscle rupture = severe mitral regurgitation |
|
|
|
what is a consequence several weeks post MI
|
dresslers syndrome - immune function
|
|
|

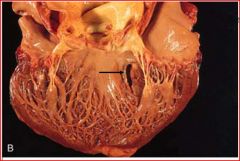
describe the pathology
|
anterior myocardial rupture
|
|
|

describe the pathology
|
papillary muscle rupture
complicate with mitral valve prolapse |
|
|
describe the pathology
|
ventricular septal rupture
|
|
|

describe the pathology
|
fibrious pericarditis
|
|
|
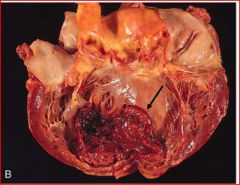
describe the pathology
|
thrombus and infarct expansion
* he said in lecture - that the bottom part was skinny and yellow = 3-7 days old |
|
|

describe the pathology
|
aneurysm
|
|
|
|
what characterizes chronic IHD
|
progressive heart failure after ischemic myocardial events
- usually secondary to MI, compensatory mech are exhausted -->up to 1/2 may req cardic transplant |
|
|
|
what condition is associated with sudden death on exertion
|
mild aortic stenosis
|
|
|
|
what is the difference between myocardial ischemia and hypoxia
|
ischemia = imbalance between the supply and demand of osyygten, combined with decreases availability of nutrient substrates and inadequate removal of toxic metabolites
hypoxia = decreased transport of oxygen by blood (cyanotic CHD, anemia, advanced lung dz) which can also be aggravated by hypertrophy, shock, tachycardia |
|
|
|
90% of myocardial ischemia is due to waht
|
atherosclerotic coronary artery disease or obstruction (CAD)
|
|
|
|
what are the acute coronary syndromes and what causes them
|
1.MI (plaque chage induces total occlusion)
2 sudden cardiac death (regional MI that induces fatal ventricular arrythmias) 3. unstable angina - (partially involved vessel and vasoconstriction causing severe transient flow reduction) 4 usually caused by sudden atherosclerotic disruption to create an unstable plaque with ooverlying thrombus |
|
|
|
what degree of obstruction do plaques become symptomatic
|
on exertion = 75%
at rest = 90% |
|
|
|
where do plaque fissures most commonly occur
|
at the junction of the fibrous cap and the normal arterial segment
|
|
|
|
what alows the fibrous cap to undergo continuous remodeling
|
production of collagen by smooth muscle cells and its degradation by macrophage metalloproteinases
destabilization occurs due to increased inflammation and cholesterol |
|
|
|
what acute phase reactant protein may predict increasked risk of CAD and where is it produced
|
C reactive protein (CRP) - syn in liver
|
|
|
|
what type of IHD is typically not associated with plaque dysruption
|
stable angina
|
|
|
|
what characterizes chronic IHD
|
progressive heart failure after ischemic myocardial events
- usually secondary to MI, compensatory mech are exhausted -->up to 1/2 may req cardic transplant |
|
|
|
what condition is associated with sudden death on exertion
|
mild aortic stenosis
|
|
|
|
what is the difference between myocardial ischemia and hypoxia
|
ischemia = imbalance between the supply and demand of osyygten, combined with decreases availability of nutrient substrates and inadequate removal of toxic metabolites
hypoxia = decreased transport of oxygen by blood (cyanotic CHD, anemia, advanced lung dz) which can also be aggravated by hypertrophy, shock, tachycardia |
|
|
|
90% of myocardial ischemia is due to waht
|
atherosclerotic coronary artery disease or obstruction (CAD)
|
|
|
|
what are the acute coronary syndromes and what causes them
|
1.MI (plaque chage induces total occlusion)
2 sudden cardiac death (regional MI that induces fatal ventricular arrythmias) 3. unstable angina - (partially involved vessel and vasoconstriction causing severe transient flow reduction) 4 usually caused by sudden atherosclerotic disruption to create an unstable plaque with ooverlying thrombus |
|
|
|
what degree of obstruction do plaques become symptomatic
|
on exertion = 75%
at rest = 90% |
|
|
|
where do plaque fissures most commonly occur
|
at the junction of the fibrous cap and the normal arterial segment
|
|
|
|
what alows the fibrous cap to undergo continuous remodeling
|
production of collagen by smooth muscle cells and its degradation by macrophage metalloproteinases
destabilization occurs due to increased inflammation and cholesterol |
|
|
|
what acute phase reactant protein may predict increasked risk of CAD and where is it produced
|
C reactive protein (CRP) - syn in liver
|
|
|
|
what type of IHD is typically not associated with plaque dysruption
|
stable angina
|
|
|
|
what is stable angina
|
transient recurrent attacks of substernal/precordial chest discomfort due to ischemia that lasts 15 sec - 15 min, but falls short of causing myocardial cell death
|
|
|
|
what are the 3 types of angina and what causes them
|
1. stable/typical - due to AS
2. prinzmetal/variant- due to coronary artery spasm 3. unstable/crescendo - due to plaque disruption |
|
|
|
how does nitroglycerin alleviate chest pain
|
it is a potent vasodilator that dec cardiac work by causing peripheral vasodilation (also causes dilation of cardiac vessels)
|
|
|
|
what are the two patterns of MI
|
transmural - ischemic necrosis of nearly full wall thickness, usually in distrobution of 1 blocked coronary artery
subendocardial - necrosis is limited to less than half of the inner wall and may overlaop vessel territories, and may be circumfrenetial when caused by hypotension/shock |
|
|
|
what layer of the heart is most vulnerable to ischemia
|
subendocardial zone
|
|
|
|
why is there a narrow rim (0.1mm) zone of preserved subendocardial tissue
|
it is sustained by diffusion of O2 and nutrients from lumen
|
|
|
|
irreversible ischemic damage (necrosis) occurs in how long
|
20-40 minutes of ischemia with <10% of normal flow
|
|
|
|
when are MIs first apparent to the pathologist
|
grossly - 12-24 hrs old
microscopically - 4-12 hrs old |
|
|
|
what is the difference between TPA, PTCA, CABG
|
TPA - thrombolysis only
PTCA - percutaneous transluminal coronary angioplasty - thrombolysis and plaque removal CABG - coronary artery bypass graft- flow redirected around affeccted vessel |
|
|
|
how does reperfused infarct appear
|
- hemorrhagic due to injured vasculature that become leaky on flow restoratin
- may have contraction bands (of closely packed sarcomeres) in irreversibly injured myocytes |
|
|
|
what patients are notorious for having atypical or siletn chest pain
|
diabetics and elderly
|
|

