![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
how much does the female and male heart normally weigh
|
females: 250-300 gm
male: 300-350 gm |
|
|
|
Describe the cardiac myocyte:
-ion transport -electrical connection -prefered energy substrate other random stuff |
-anastomosing electrically connected gap jxns, intercalated disks
-highly organized T tubule system, SR, terminal cisternae for ion transport - perfers Fatty Acids, long chain FFA (glucose and galactose also used) -other: 60% contractile, 25% mito, has receptors and secretory granules (ANP) |
|
|
|
normal myocyte has central nuclei, what happens during injury
|
during injury they get large and rectangle, he described them as "box car nuclie"
|
|
|
|
where do you measure the thickness of the ventricle
|
1 cm below the mitral valve
|
|
|
|
what determine CO? (what is the equation
|
SV x HR
strokevolume & heart rate |
|
|
|
preload = EDV, what factors affect preload
|
1. increase with exercize, with increase in blood volume, and sympathetics.
2. decrease with venodilators |
|
|
|
afterload = mean arteial pressure (proportional to perifpheral resistance)
|
vasodilators decrease afterload
|
|
|
|
what variables affect CO
|
SV CAP
Stroke Volume Contractility Afterload Preload |
|
|
|
what law governs wall tension
|
LaPlace's law = PxR / 2T
as wall thickness increases wall tension decreases\ if you dilate the ventricle tension goes up |
|
|
|
on a cellular level what controls contractility, ultimately determining SV
|
-ion fluxes, membrane pumps
-actin myosin coupling -blood flow, oxygenation, cellular energetics - adrenergic receptors, other circulating and local factors. |
|
|
|
on an organ level what controls contractility, ultimately determining SV
|
- how quickly, efficiently, forcefully the ventricle can contract
- Measured by** EJECTION FRACTION: SV/EDV NI= 55-85% Mod dysfxn= 30-50% ***SEVER DYSFXN = BELOW 30% |
|
|
|
what are the 5 principle mechanisms for CV dysfunction
|
-pump failure - most commome
-obstuction to flow - HTN or aortic stenosis -regurgitant flow (valvular dz) -disorders of cardiac conduction (arrythmias) = not efficient heart -interuption of circulation = coronary artery dz |
|
|
|
What is the difference between heart failure and congestive heart failure
|
Heart failure is the pathophysiologic state where the heart can not deliver enough blood to the meet the needs of the body.
In contrast congestive heart failure is a syndrome that overall reflects inadequate pump function |
|
|
|
What clinical presntations do you see in RHF
|
hepatosplenomegaly, peripheral edema, and cough
|
|
|
|
pure HTN leads to what type of cardiomegaly
|
hypertrophy not dilation
|
|
|

describe the pathology
|
L side = concentric hypertrophy -->HTN
R side = dilation and hypertrophy -->HTN + ischemia -->cannot pump against volume |
|
|
|
4 conditions in cardiomegaly
|
1 is affecting the kidneys-->dying-->renal failure is coming-->Inc afterload
2 is accelerated - HTN too much for heart = dilation 3 CAD-->infarcts-->slow myocardial scarring won't be able to pump and starts dilating 4. Massive MI - rapid increase in dz and heart failure, not pumping against system |
|
|

review figure
|
what are the 3 events that lead to heart failure and cardiac dysfxn
|
Hypertension
Valvular Dz Myocardial Infarction |
|
|
what is the definition of shock
|
systemic hypoperfusion often related to sudden loss of cardiac function
-many diverse forms/etiologies (see Sim center notes) |
|
|
|
when the heart is experiencing excessive hemodynamic burden or disturbance in myocardial contractility, how does the heart compensate?
|
Frank Starling-(inc BP) increased preload yields increased contractility-->if goes to far =heart failure
structural changes in myocardium, augmented muscle mass activation of neurohumoral systems: norepi/ept, renin-angio-aldo, ANP |
|
|
|
what is the frank starling mechanism
|
incrased preload of dilation enhnaces contractility (more sarcomere cross bridging) and better cardiac performance
|
|
|
|
which is most common systolic or diastolic dysfunction
|
systolic dysfunction
|
|
|
|
what are the 3 most common causes of systolic (left-sided) dysfunction
|
1 Ischemic Heart Dz
2 HTN 3 Aortic or mitral valve abnormalities progressive deterioration of contractile function |
|
|
|
name the causes of diastolic dysfunction
|
heart chamber can't relax and filling is compromised = restrictive heart diseases
massive L vent hypertrophy, myocardial firbrosis, amyloid deposition, constrictive pericarditis |
|
|
|
does augementation of cardiac muscle happen by hypertrophy or hyperplasia of muscles?
|
hypertrophy since myocytes are terminaly differentiated they cannot undergo hyperplasia
|
|
|
|
what are the two types of congestive heart failure
|
Forward failure = diminished cardiac output -->can't meet demand, renal failure,ect because try to preserve Brain
Backward failure = accumulation of blood in the venous system OR BOTH |
|
|
|
What are the common causes of left heart failure
|
Ischemic heart disease, HTN, Aortic;mitral valve disease, non-ischemic myocardial disease
|
|
|
|
what happens in left heart failure
|
progressive damming of blood in the pulmonary circulation and diminished peripheral blood pressure/flow
|
|
|
|
what are clinical symptoms of forward failure
|
poor organ perfusion (especially kidneys and brain)
|
|
|
|
what are the clinical symptoms of backward failure
|
dyspenea and peripheral edema
|
|
|
|
List findings in left sided heart failure
|
LV hypertrophy, +/- dilation, fibrosis, secondary enlargement of atrium (may cause atrial fibrillation with increased risk of embolism), pulmonary congestion, edema, dyspnea, orthopnea, PND, cough
|
|
|
|
what do you see in the lungs with congestion and edema
|
sideroblasts (heart failure cells),, kerley B lines on xray, dyspnea, orthopnea, paroxsymal nocrurnal dyspnea
|
|
|
|
what causes kerley b lines on xray
|
perivascular and interstitial transudate
|
|
|
|
what is paroxsymal nocturnal dyspnea
|
attacks of "suffocation" when lying down at night
|
|
|
|
decreased renal perfusion leads to what?
|
activation of the renin-angio-aldo system causing retetion of salt and water giving volume expansion-->which contributes to pulmonary edema -->counteracted by ANP by atrial dilation
|
|
|
|
Right sided heart failure is most commonly due to
|
secondary to left sided heart failure, causing increased pulmonary pressure
|
|
|
|
how does the congestion inthe RHF compare with LHF
|
it is very minimal with RHF, the "congestion" in RHF occurs as engorgemnet of systemic and portal venous systems, giving ascites and anasarca
|
|
|
|
RHF causes what findings int he liver
|
passive centrilobular congestion (and possibly necrosis if concurrent with LHF ischemia)
affected centrilobular areas can become fibrotic periportal areas usually spared |
|
|
|
what is pure RHF due to
|
cor pulmonade due to severe and chronic pulmonary HTN
|
|
|
|
what is nutmeg liver
|
the combination of mottled appearance due ot retrograde congestion and hemorrhagic plus ischemic necrosis
**NOT portal tracts |
|
|
|
which sided heart failure causes each lung finding listed below:
1. pulmonary effusion 2. pulmonary edema |
1pulmonary effusion = RHF
2pulmonary edema = LHF |
|
|
|
what is massive generalized edema called
|
anasarca
|
|
|
|
what other lung disease can cause RHF
|
COPD, diffuse lung dz, pulmonary emboli, sarcoidosis
|
|
|
|
what is the progression in RHF
|
Increase RVhypertrophy-->then dilates-->affects the valve-->atrial hypertrophy-->then dilates-->creates area prone to thrombi-->could cause PE
** once start-->gets worse -primary pulmonary HTN is not very common |
|
|
|
what is cardiac cirrhosis
|
subsequently to centrilobular necrosis you get central fibrosis
|
|
|
|
heart failure is usually a biventricular process secondary to chronic cardiac decompensation resulting in combined effects and symptoms
|
random slide at end of this lecture that i couldnt come up with a question for
|
|
|

describe the pathology
|
this is a picture of an actual nutmeg(upper left) and nutmeg liver
I have stars by this in my notes, so i would make sure to know this and the previous cards on the pathogenesis of this finding |
|
|
|
besides predisposing to CHF, what is also an independent risk factor for sudden death?
|
Left Vent Hypertrophy
|
|
|
|
how does hyperthyroidism trigger tachycardia
|
stimulation of beta-adrenergics
|
|
|
|
what causes the following heart weights:
-250-350 -350-600 -400-800 -600-1000 |
250-350 = normal
-350-600 = (2x normal) pumonary HTN, ischemic heart dz -400-800 = 3x normal, systemic HTN, aortic stenosis, mitral regurgitation, hypertrophyic cardiomyopathy -600-1000 = >3x normal aortic regurgitation, hypertrophic cardiomyopathy |
|
|
|
contrast hypertrophy due to pressure vs volume overload
|
Pressure (aortic stenosis, HTN) = concentric, parallel sarcomere deposition, cross sectional area expanded by cell length unchanged
volume (valvular dz, MI) = new sarcomeres and cell length increases giving dilation and increase wall thickness |
|
|
|
what are other abnormalities in both types of hypertrophy
|
decreased capillary to myocyte ration
increased fibrotic tissue abnormal protein deposition |
|
|
|
what are predictable and sequential lung findings in CHF
|
perivascular and interstitial transudate, edematous widening of alveolar septa, alveolar space edema
|
|
|
|
what are 5 principal mechanisms that cause cardiovascular dysfunction and give examples of each
|
1. failure of pump: inadequate muslce contraction (systolic dysfxn) or relaxation (diastolic dysfxn)
2. flow obstruction: aortic stenosis, HTN, aortic coartation 3. regurgitant flow; aortic and mitral regurgitation 4. conduction disorders: heart block arrythmias 5. ciculatory disruption: blood loss, GSW |
|
|
|
LO - compare teh hypertrophy of the trained heart athletic heart with that of the failing heart
|
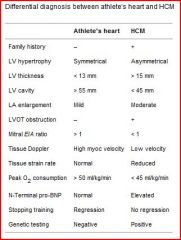
yes, i know it wasn't in the notes anywhere or Robbins that I could find quickly but found this in the International Journal of Cardiology via a google search
|
|

