![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
254 Cards in this Set
- Front
- Back
|
How controls the National Practioner Data Bank? |
The Health Resources and Services |
|
|
Role of The Agency for Health Care |
improving the quality of health care |
|
|
What are the key features of an HMO? |
Offers a standardized benefits package to |
|
|
Point of service plan |
Indemnity-type option for HMOs or PPOs * participants must designate a network-based physician as their primary health care provider |
|
|
Examples of PPOs |
Private (Indemnity) insurance payment Physician, hospital, and other providers |
|
|
Utilization Management |
A cost-containment strategy that limits health |
|
|
Disease Management |
a comprehensive effort to help clinicians plan |
|
|
What percent of Americans receive health insurance from their employer? |
70% |
|
|
Medicare part A |
Hospital inpatient services--partial payment |
|
|
Medicare part B |
Fee for service |
|
|
Medicare part C |
Medicare+Choice: a managed *Most plans require a primary care physician *some plans cover prescription drugs, dental care, vision care |
|
|
Part D |
Prescription drug benefit plan |
|
|
Act that created medicare part D |
Medicare Modernization Act of 2003 |
|
|
Approx how many people are covered by medicaid? |
>62 million people |
|
|
True or false States receive matching funds from the feds for SCHIP |
True |
|
|
True or False? SCHIP funds are often used to expand existing |
True |
|
|
True or False The ACA ends Pre-Existing Condition Exclusions for Children: |
true |
|
|
True or False The ACA:Keeps Young Adults Covered: If you are under 26,you may be eligible to be covered under your parent’s health plan. |
T
|
|
|
True or False The ACA ends Arbitrary Withdrawals of Insurance Coverage: |
T
|
|
|
True or False The ACA Guarantees Your Right to Appeal: You now have the right to ask that your plan reconsider its denial of payment. |
T
|
|
|
True or False? The ACA ends Lifetime Limits on Coverage: Lifetime limits on |
T
|
|
|
True or False? The ACA reviews Premium Increases: Insurance companies |
T
|
|
|
True or False? The ACA helps You Get the Most from Your Premium Dollars: |
T
|
|
|
True or False? The ACA Covers Preventive Care at No Cost to You: You may be eligible for recommended preventive health services. No copayment. |
T
|
|
|
True or False? The ACA protects Your Choice of Doctors: Choose the primary |
T
|
|
|
True or False? The ACA removes Insurance Company Barriers to Emergency Services: You can seek emergency care at a hospital outside of your health plan’s network. |
T
|
|
|
True or False? The ACA the health reform law will require all businesses, even the smallest ones, to provide health insurance for their employees. |
False. The law does not require employers to provide health benefits. However, it does impose penalties in some cases on larger employers (those with 50 or more workers) that do not provide insurance to their works or that provide coverage that is unaffordable. |
|
|
True or False? The health reform law will allow undocumented immigrants to receive financial help from the government to buy health insurance. |
False
|
|
|
Top three expenditures by type of service
|
Hospital, physician services, rx drugs, and other non-durable medical services
Source: Kaiser foundation. |
|
|
Diagnosis Related Group (DRG)
|
What is a statistical system of classifying any inpatient stay for the purpose billing. Divided into body systems and subgroup for medicare reimbursement.
|
|
|
Resource relative value scale
|
payments to physicians are based on the resour.ces necessary to provided them. include practice, physician, and liability insurance. Conversion factor used to account for resource difference by geographic area.
|
|
|
The Hospital Survey and ConstructionAct (The Hill-Burton Act--1946)
|
First federal attempt to enact global health planninglegislation
Aimed to improve the hospital bed ratio in rural areasand increase numbers of physicians in those areas. Required states to designate a single agency to plan andimplement hospital construction Limited outcome because end result was state based andfocused on beds rather than services |
|
|
Overarching health people goals
|
Attain high-quality, longer lives free of preventable disease, disability, injury, and premature death;
Achieve health equity, eliminate disparities, and improve the health of all groups; Create social and physical environments that promote good health for all; Promote quality of life, healthy development, and healthy behaviors across all life stages. |
|
|
Performance
|
How a plan or provider is functioning with regard to specific standards, benchmarks, or measures. The measures are often indicators of value, quality, or both.
|
|
|
Efficiency
|
Maximization of the quality of a comparable unit of health care delivered for a given unit of health resources used
|
|
|
Economy
|
The total level of expenditure for healthcare, given realistic performance on quality andefficiency, and a realistic assessment of availableresources
|
|
|
Structural measures
|
The attributes of the settings in whichcare occurs
Provide the basis for most currentregulations Often required by governmentprograms through accreditation,licensure, or certification requirements Ensure a minimal capacity for quality. |
|
|
Process
|
Denotes what is actually done in givingand receiving careƒÞ Patient activities in seeking careƒÞ Patient activities in carrying out therecommended careƒÞ Physician activities in making a diagnosisand recommending or implementingtreatment
|
|
|
Outcome measures
|
Assess the quality of the final product Used to capture the effect of anintervention on health status control of a chronic condition specific clinical findings patients’ perceptions of care.
|
|
|
staff model HMO
|
physicians are employed and all premiums are paid to the HMO, which then compensates the physicians on a salary and bonus arrangemen -
|
|
|
group model HMO
|
Contracts with certain provider groups, with whom rates for medical care are negotiated. HMO then pays the negotiated rate for care provided to the policyholders. Contracts are also made with hospitals for care provided to the policyholders.
|
|
|
network model HMO
|
Under this model, an HMO contracts with several physician groups. Physicians may share in savings, but may provide care for other than HMO members.
|
|
|
independent practice association
|
a U.S. type of physician alliance in which the physicians own the practice, Physicians are legally organized as a corporation, partnership, professional corporation, or foundation to contract as a group to provide services. Economic risk is shared, but overhead is not. May contract with a healthmaintenance organization (HMO) to service enrollees but will usually still see non-HMO clients.
|
|
|
JCAHO
|
Accrediates: Acute and long-term care Ambulatory care Behavioral health care Home care, clinical laboratory services Managed care networks
|
|
|
National Committee forQuality Assurance (NCQA)
|
nationally recognized evaluation of managed careplans purchasers, regulators, consumers
|
|
|
Health Plan Employer Data andInformation Set (HEDIS)
|
introduced by NCQA in 1991
* Annual updates to help purchasers andconsumers compare the quality ofcommercial, Medicaid, and Medicaremanaged care plans. *Standardized performance measuresfocusing on quality of care in cancer,heart disease, smoking, asthma, diabetes * Used for MCOs * Informs purchasers and consumers |
|
|
The American Medical Accreditation Program(AMAP)
|
a voluntary accreditation programthat measures and evaluates individualphysicians against national standards, criteria,and peer performance in: Credentials Personal qualifications Environment of care Clinical process Patient 149outcomes
|
|
|
National Practitioner Data Bank
|
Purpose--facilitate a comprehensive review ofprofessional credentials Established by Title IV of Public Law 99-660, the Health Care QualityImprovement Act of 1986. Administered by the Bureau of HealthProfessions, HRSA, HHS
|
|
|
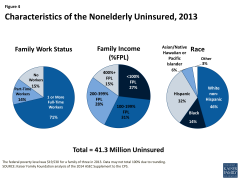
Characteristics of uninsured |
|
|
|
First health plan in the US? |
Blue cross (covered only hospitalizations) |
|
|
Title XVII |
Medicare |
|
|
Title XIX |
Medicaid |
|
|
True or false? Local public health dept are organized most frequently at the county level rather than at other local government levels. |
True |
|
|
Legislation required employers to contribute an amount equal to that contributed toward indemnity plan premiums for employes. |
Health maintenance act of 1973. |
|
|
How do PPOs earn money? |
By charging an access to the insurance company for use of their services |
|
|
Review types of health insurance plans. |
https://www.youtube.com/watch?v=25G9hFRmCM8 |
|
|
What are the two basic categories of provider reimbursement? |
variable reimbursement arrangements Fixed imbursement |
|
|
What are two major concerns with variable reimbursement models (e.g., RBRVS?) |
Upcoding, e.g., making a short office visit and extended one Unbundling, billing separately for services for which a bundled coded exists. |
|
|
What are some examples of fixed reimbursement arrangements? |
*DRG *Medical severity diagnosis related groups (MS-DRGs) * Case rate/bundled case rate-predetermined, fixed payment for all services related to a defined episode of care, e.g., heart transplant (generally used for high cost/high risk proceedures) *Global fee (a type of case rate). Flat rate negotiated for a set of multiple services, e.g., pre natal, deliver, and post-natal care. * Per diem. Pay a fixed rate for each day of stay. Hospitals less likely to shorten stay. So insurance places tough length of stay guidelines. *Capitation. Providers make $ when patients are health, e.g., providing low cost preventive services. Financial incentive is to minimize care. |
|
|
What is a risk pool?
|
Money available for reimbursement after certain targets are met, e.g. hospital days per 1,000 pt. Can also involve with holding $. |
|
|
Who finances America's hospital bill? |
1) Private insurers 2) Medicare 3) Medicaid 4) Out of pocket |
|
|
What are two evidence based practices to increase immunization rates in children? |
Call/reminder systems Physician based tracking |
|
|
How were physician practices structured in 2014 (AMA practice arrangment survey?) |
53% of physicians are self-employed 60% work in practices owned by physicians 23% work in practices partially owned by a hospital
Trends project more physicians will work for hospitals |
|
|
Title V |
MCH state block grants |
|
|
Title XXI |
SCHIP |
|
|
Title IIX |
Medicaid |
|
|
Title XVIII |
Medicare |
|
|
What drives the me median age of the population? |
Birth rate |
|
|
What is the difference between need and utilization of healthcare services? |
Unmeet need |
|
|
Adverse selection. |
Persons who are sicker are more interested in acquiring health insurance. This drives the cost up for other enrollees. Thus, insurers prefer to insure workers. |
|
|
How is medicare part B and D financed and subsidized? |
General taxes |
|
|
What laws does the federal government use to authorize public health actions? |
Interstate commerce Welfare clause |
|
|
A health plan that is similar to those offered by PPOs, except use is restricted to in network providers |
Exclusive provider plan |
|
|
Setting insurances premiums based on a groups' health care expenses in a prior period. This allows groups to pay less. |
Experience rating |
|
|
Setting reimbursement based on actual cost incurred |
Retrospective payment. |
|
|
Reimbursement to a provider to cover cost plus a factor for capital? |
Cost-plus. |
|
|
Public health care programs only for select groups of people. |
categorical programs |
|
|
What drives the me median age of the population? |
Birth rate |
|
|
A classification to differentiate nursing home residents by their level of use? |
Resource utilization groups |
|
|
An aggregate of the severity of conditions requiring medical intervention. Categories are mutually exclusive and differentiate patients according to the extent of resource use. |
case-mix |
|
|
Method of determining health insurance premiums that takes into account demographic factors such as age, gender, geography, and family composition, while ignoring other risk factors. |
adjusted community rating |
|
|
An account set up and funded by an employer that can be used by an employee or a retiree to pay for health care expenses. |
health reimbursement arrangement |
|
|
What is the difference between need and utilization of healthcare services? |
Unmeet need |
|
|
Adverse selection. |
Persons who are sicker are more interested in acquiring health insurance. This drives the cost up for other enrollees. Thus, insurers prefer to insure workers. |
|
|
How is medicare part B and D financed and subsidized? |
General taxes |
|
|
What laws does the federal government use to authorize public health actions? |
Interstate commerce Welfare clause |
|
|
A health plan that is similar to those offered by PPOs, except use is restricted to in network providers |
Exclusive provider plan |
|
|
Setting insurances premiums based on a groups' health care expenses in a prior period. This allows groups to pay less. |
Experience rating |
|
|
Setting reimbursement based on actual cost incurred |
Retrospective payment. |
|
|
Reimbursement to a provider to cover cost plus a factor for capital? |
Cost-plus. |
|
|
Public health care programs only for select groups of people. |
categorical programs |
|
|
A phenomenon in which individuals who are likely to use more health care services than others due to poor health enroll in health insurance plans in greater numbers, compared to people who are healthy. |
Adverse selection |
|
|
Separate payments to the providers for each separate service, such as examination, administering a test, and hospitalization |
Fee for service |
|
|
Separate payments to the providers for each separate service, such as examination, administering a test, and hospitalization |
Fee for service |
|
|
Determined by a spell of illness beginning with hospitalization and ending when the beneficiary has not been an inpatient in a hospital or a skilled nursing facility for 60 consecutive days |
Benefit period |
|
|
Separate payments to the providers for each separate service, such as examination, administering a test, and hospitalization |
Fee for service |
|
|
Determined by a spell of illness beginning with hospitalization and ending when the beneficiary has not been an inpatient in a hospital or a skilled nursing facility for 60 consecutive days |
Benefit period |
|
|
An organized approach to evaluating and coordinating care, particularly for patients who have complex, potentially costly problems that require a variety of services from multiple providers over an extended period |
Case-management |
|
|
An evaluation required under federal regulations, before a patient can be admitted to a Medicaid-certified nursing facility, to determine whether a nursing facility is the best alternative for individuals with serious mental illness or intellectual disability or whether their needs can be adequately met in community-based settings. |
Preadmission Screening and Resident Review (PASRR |
|
|
An evaluation required under federal regulations, before a patient can be admitted to a Medicaid-certified nursing facility, to determine whether a nursing facility is the best alternative for individuals with serious mental illness or intellectual disability or whether their needs can be adequately met in community-based settings. |
Preadmission Screening and Resident Review (PASRR |
|
|
A health plan that combines a savings option with a health insurance plan carrying a high deductible |
High deductible plan. |
|
|
A legal entity formed between a hospital and a physician group to achieve shared market objectives and other mutual interests. |
Physician hospital organization |
|
|
Stop-loss coverage that self-insured employers purchase to protect themselves against any potential risk of high losses. |
Reinsurance |
|
|
Factors that influence an individual and a population’s health |
Genetic make up 20% of premature deaths Individual Behaviors 50% of premature deaths Medical Practice 10% of premature deaths Social and Environmental 20% of premature deaths |
|
|
In 2010, the healthcare workforce composed how much of the total workforce. |
3% |
|
|
What percent of health professionals work in hospitals(2010)? |
40 % |
|
|
What percent of health care professionals work in long term care/nursing homes?
|
12% |
|
|
What percent of health care professionals work in physician offices? |
10% |
|
|
What percent of health care professionals work in physician offices? |
10% |
|
|
How many physicians are there per /100,000 people? |
28/100000 in 2009 |
|
|
What percent of physicians are primary care and specialists? |
approximately 40.8% of the 40.8 %physicians are generalists and approximately 59.2% are specialists |
|
|
Health care information organization |
An independent organization that brings together health care stakeholders within a defined geographic area and facilitates electronic information exchange among these stakeholders with the objective of improving the delivery of health care in the community |
|
|
Required premarket notification to the FDA so the agency could assess the safety of a new drug or device. |
1938 Food, Drug, and Cosmetic Act |
|
|
Required premarket notification to the FDA so the agency could assess the safety of a new drug or device. |
1938 Food, Drug, and Cosmetic Act |
|
|
1962 Kefauver-Harris Amendments |
Premarket notification was inadequate. The FDA took charge of reviewing the efficacy and safety of new drugs, which could be marketed only once approval was granted. |
|
|
Safe medical device act of 1990. (FDA) |
Health care facilities must report serious or potentially
serious device-related injuries, illness, or death of patients and/or employees. |
|
|
Safe medical device act of 1990. (FDA) |
Health care facilities must report serious or potentially
serious device-related injuries, illness, or death of patients and/or employees. |
|
|
Food and Drug Administration Safety Innovations Act (2012) |
Allows the FDA to use markers that are thought to predict or that are reasonably likely to predict clinical benefit to qualify a drug for accelerated approval if the drug is indicated for a serious condition and fills an unmet medical need. |
|
|
Medical Device Amendments, 1976 (to the FD&C Act of 1938) |
Class I – only subject to controls over fraudulent claims of effectiveness Class II – subject to labeling requirements, performance standards, and post-market surveillance Class III – require premarket approval |
|
|
COBRA |
Employment-based coverage can continue for 18 months after separation from a job 29 month coverage for individuals declared to be disabled (HIPAA 1996) Family coverage for 36 months if the former worker dies, enrolls in Medicare, or is divorced The individual must pay 102% of the group premium The ACA does not affect it |
|
|
Outpatient Prospective Payment System (OPPS) |
For services provided by hospital outpatient departments; OPPS for nonhospital ambulatory surgery centers Ambulatory Payment Classifications (APCs): 300 procedural groups New technology APCs a bundled rate to include anesthesia, drugs, supplies, recovery Physician services are reimbursed separately, based on RBRVS |
|
|
Case-Mix Methods |
Case mix: Aggregate severity of conditions Determined through a comprehensive assessment Mutually exclusive case-mix categories represent resource use Resource Utilization Groups (RUGs) are used to determine per-diem reimbursement for skilled nursing facilities Case-Mix Groups (CMGs) are used to reimburse inpatient rehabilitation facilities |
|
|
Outpatient Prospective Payment System (OPPS) |
For services provided by hospital outpatient departments; OPPS for nonhospital ambulatory surgery centers Ambulatory Payment Classifications (APCs): 300 procedural groups New technology APCs a bundled rate to include anesthesia, drugs, supplies, recovery Physician services are reimbursed separately, based on RBRVS |
|
|
What is a Critical access hospital ? |
Authorized under the Balanced Budget Act, 1997 To save small rural hospitals from closure Maximum 25 acute care or swing beds Emergency services must be available Must meet a distance test Can have a 10-bed psychiatric unit, a 10-bed rehabilitation unit, and a SNF Cost-plus reimbursement, not to exceed 101% of cost |
|
|
What is case management? |
Coordination of care for complex and potentially costly cases A variety of services from multiple providers are needed over an extended period Secondary and tertiary services are needed more often than primary care (e.g., AIDS, spinal cord injury, transplants, severe injuries, cases, etc.) Cost savings have been achieved with better delivery of care and reduced hospitalizations |
|
|
Disease management |
Population-oriented strategy for chronic problems Evidence-based treatment guidelines Focus on education, self-management training, monitoring of the disease process, and follow-up to ensure compliance–self-care with professional support Goal: prevent or delay complications Although cost savings are uncertain, better quality and disease control are achieved |
|
|
Staff model HMO |
Employ physicians on salary Contracts for only uncommon specialties and hospital services Advantages Exercise control over physicians Convenience of one-stop shopping Disadvantages Fixed salary expense can be high Expansion into new markets is difficult Limited choice of physicians |
|
|
Group model HMO |
Contract with a single multispecialty group practice Separate hospital contracts Group practice is paid a capitation fee Advantages No salary or facility expenses (as in staff model) Well known practice may lend prestige Disadvantages Difficulty with service obligations if a contract is lost |
|
|
Network HMO |
Contract with more than one group practice Variations Contracts with only PCPs who are financially responsible for specialty services, or Separate contracts with PCPs and specialists Advantage Wider choice of physicians Disadvantage Dilution of utilization control |
|
|
Advantages/ disadvantages of IPAs? |
Eliminates the need to contract with various providers Transfers financial risk to the IPA Choice of providers Disadvantages Difficulty with service obligations if a contract is lost Dilution of utilization control Generally, a surplus of specialists |
|
|
What are the features and advantages/disadvantages of a PPO? |
Discounted fees are used to pay providers (no direct risk sharing) Generally, no gatekeeping and other controls PPOs enjoy the highest enrollment (in employment-based insurance market) of all managed care plans |
|
|
What is a POS plan? |
Cross between HMO and PPO HMO features are retained (utilization controls, capitation) PPO feature: Open access option available at the point of service |
|
|
Case-Mix Methods |
Case mix: Aggregate severity of conditions Determined through a comprehensive assessment Mutually exclusive case-mix categories represent resource use Resource Utilization Groups (RUGs) are used to determine per-diem reimbursement for skilled nursing facilities Case-Mix Groups (CMGs) are used to reimburse inpatient rehabilitation facilities |
|
|
Home Health Resource Groups (HHRG) |
The PPS is fixed, predetermined for each 60-day episode of care regardless of specific services delivered Services are bundled under one payment on a per patient basis Durable medical equipment (DME) and drugs not included Outcome and Assessment Information Set (OASIS) is used to assign patients to one of 153 HHRG categories |
|
|
Health Care Service Frequency |
Primary Care 75−85% of population requires only primary Secondary Care 10−12% requires referral to short-term secondary care Tertiary care 5−10% require tertiary |
|
|
Discharges/ 1000 population |
An indicator of access and utilization Number of overnight patients a hospital serves in a given time period Include newborns and deaths |
|
|
Average length of stay definition? |
Days of care/Discharges An indicator of severity of illness and resource use Highest in federal hospitals, followed by state and local government hospitals Private nonprofit and for profit hospitals had the same ALOS in 2010 |
|
|
Occupancy rate |
Percent of capacity occupied Calculation: average daily census / number of available beds (capacity) × 100 A measure of performance |
|
|
Rehab hospital characteristics |
Therapeutic services to restore maximum function in patients Medicare rule: 75% of the inpatients must require intensive rehabilitation (at least 3 hours of therapy per day) PT, OT, Speech/language pathology Approximately 80% are hospital-based units rather than freestanding |
|
|
Acute length of stay definition |
ALOS of 25 days or less Treat acute conditions |
|
|
Approximately what percent of U.S. Hospitals are on rural areas? |
40% |
|
|
Benefits of managed care organizations ? |
*provides better value than indemnity insurance *Good access to primary care and preventive services in certain key areas On a larger scale, impact on access is not well established *quality is equivalent to indeminty plans if not better |
|
|
Types of service integration |
Management services organizations (MSOs) Physician-hospital organizations (PHOs) Provider-sponsored organizations (PSOs) |
|
|
MSO |
Supply management expertise, administrative tools, and information technology to physician group practices Mainly used by small groups that cannot employ full-time managers |
|
|
Types of highly integrated healthcare systems |
Integrated delivery systems (IDSs) Accountable care organizations (ACOs) Payer−provider integration |
|
|
Integrated delivery system |
A network of organizations Coordinated continuum of services Willing to be held clinically and fiscally accountable Managed care promoted the formation of IDSs Cost effective for MCOs to contract with a full service provider Preference by MCOs to seek cost-efficient providers who will take responsibility for quality Providers strengthened their bargaining power with MCOs and protected their autonomy |
|
|
Accountable care organization |
Integrated group of providers who take responsibility for delivering services to a defined population Take responsibility for improving health status Provide cost-efficient care Focus on satisfaction with care
*use mechanisms already used by MCOs and IDSs (disease management, care coordination, sharing cost savings with providers, etc.) to improve cost, quality, and population health |
|
|
True or false. 2/3 of all long te care is paid by Medicare |
False. Medicaid is the largest payer |
|
|
True or false: white women have the highest and Hispanic women the least utilization of mammograms? |
True |
|
|
True or false: white women have the highest and Hispanic women the least utilization of mammograms? |
True |
|
|
True or false? Heart disease and stroke account for a higher percentage of deaths among women than men at all stages of life: 42% of women with heart attacks die within the year, but only 24% of men do |
True |
|
|
True or false? Until the age groups 65 and older, women have higher physician utilization rates than men However, hospitalization rates are comparable for men and women |
True |
|
|
Accessibility |
fit between the locations of providers and patients (transportation, convenience) |
|
|
Accessibility |
fit between the locations of providers and patients (transportation, convenience) |
|
|
Accommodation |
how resources are organized to provide services and the patient’s ability to use the services (timely appointments, quick service, walk-ins, etc.) |
|
|
Accessibility |
fit between the locations of providers and patients (transportation, convenience) |
|
|
Accommodation |
how resources are organized to provide services and the patient’s ability to use the services (timely appointments, quick service, walk-ins, etc.) |
|
|
Acceptability |
compatibility (waiting time, race, culture, gender, etc.) |
|
|
In the Omnibus Budget Reconciliation Act of 1986, Congress provided rural hospitals three important provisions: |
Separated urban and rural pools of funds used to pay for outliers, or cases in which excessive expenditures above the prospective payment system allotment are incurred. Provided early payments to those with less than 100 beds. Changed criteria for rural referral centers to allow more hospitals to qualify for funds. |
|
|
In the Omnibus Budget Reconciliation Act of 1986, Congress provided rural hospitals three important provisions: |
Separated urban and rural pools of funds used to pay for outliers, or cases in which excessive expenditures above the prospective payment system allotment are incurred. Provided early payments to those with less than 100 beds. Changed criteria for rural referral centers to allow more hospitals to qualify for funds. |
|
|
Has sole jurisdiction over Medicare Part A, Social Security, unemployment compensation, public welfare, and health care reform |
House ways and means committee |
|
|
In the Omnibus Budget Reconciliation Act of 1986, Congress provided rural hospitals three important provisions: |
Separated urban and rural pools of funds used to pay for outliers, or cases in which excessive expenditures above the prospective payment system allotment are incurred. Provided early payments to those with less than 100 beds. Changed criteria for rural referral centers to allow more hospitals to qualify for funds. |
|
|
Has sole jurisdiction over Medicare Part A, Social Security, unemployment compensation, public welfare, and health care reform |
House ways and means committee |
|
|
Has jurisdiction over Medicaid, Medicare Part B, matters of public health, mental health, health personnel, HMO’s, foods and drugs, air pollution, consumer products safety, health planning, biomedical research, and heath protection |
House energy and commerce committee . |
|
|
Has jurisdiction in most health bills |
Committee on labor and human resources |
|
|
Has jurisdiction over taxes and revenues, matters related to Social Security, Medicare, Medicaid, and Maternal and Child Health |
Committee on finance |
|
|
Provided greater increase in reimbursement to rural hospitals than to urban hospitals Allowed rural hospitals located adjacent to metropolitan statistical areas to be defined as urban hospitals Authorized a rural health care transition program to provide assistance to hospitals and others wishing to adopt new service delivery strategies |
The OBRA of 1987 included provisions that |
|
|
Cont...The OBRA of 1987 included provisions that: |
Required a report in the appropriateness of separate urban and rural rates Authorized small rural hospitals to serve as residency training cites for physicians |
|
|
The leftover sum by the provider to the patient after insurance has only partially paid the charge initially billed |
balance billing |
|
|
The leftover sum by the provider to the patient after insurance has only partially paid the charge initially billed |
balance billing |
|
|
occurs when high-risk individuals, that is, people who are likely to use more health care services than others because of their poor health status, enroll in health insurance plans in greater numbers, compared to people who are healthy |
adverse selection |
|
|
adjusting premiums to reflect health status and making potential high-cost enrollees pay more |
Risk rating |
|
|
Provisions in the ACA related to primary care include |
(1) increasing Medicare and Medicaid payments to primary care providers, (2) creating new incentives such as funding for scholarships and loan repayment for primary care providers working in underserved areas, (3) expanding the health center program and bolstering the capacity of health centers, and (4) establishing additional training programs such as establishing 11 Teaching Health Centers for training primary care providers |
|
|
8. How does hospital utilization vary according to a person’s age, gender, and socioeconomic status? |
< 1 years of age has the highest utilization, females > men, low SES.hgiher SES, western states have the lowest utilization |
|
|
a model that requires a Medicaid enrollee to choose a PCP, who is responsible for coordinating the enrollee’s care and paid a monthly fee for doing so, on top of the payment for providing medical services. In general, all medical services are reimbursed on a fee-for-service basis |
primary case management |
|
|
2. What are the three main payment mechanisms managed care uses? In each mechanism, who bears the risk? |
Fee for service: MCO Capitation: provider Discounted fees: MCO Salary: Shared (physicians bonuses tied to performance. |
|
|
does case management differ from disease management? |
Case management targets high-risk patients--those who, because of diverse combinations of health, social and functional problems, are likely to need hospitalization. Disease management targets patients who have one major diagnosis and who, because of their major diagnosis, have a relatively standard set of needs. |
|
|
What three sources do health ecomonist use to guage over spending in the US healthcare sustem? |
1. International comparisons 2. Rise of premiums 2. Spending on public programs |
|
|
What are some supply side (regulatory) cost containment strategies? |
Restrictions on capital expenditures (new construction, renovations, and technology diffusion) Example: Certificate of need Restrictions on supply of physicians Example: Entry barriers for foreign medical graduates |
|
|
NQS, Priority 1: Making care safer by reducing harm caused in the delivery of care |
Reduce preventable hospital admissions and readmissions. Reduce the incidence of adverse health care-associated conditions. Reduce harm from inappropriate or unnecessary care. |
|
|
Critical pathway |
Multidisciplinary management tool based on evidence-based practice for a specific group of patients with a predictable clinical course, in which the different tasks (interventions) by the professionals involved in the patient care are defined, optimized and sequenced either by hour (ED), day (acute care) or visit (homecare). Outcomes are tied to specific interventions. |
|
|
Priority 2: Ensuring that each person and family members are engaged as partners in their care |
Improve patient, family, and caregiver experience of care related to quality, safety, and access across settings. In partnership with patients, families, and caregivers—and using a shared decision-making process—develop culturally sensitive and understandable care plans. Enable patients and their families and caregivers to navigate, coordinate, and manage their care appropriately and effectively. |
|
|
Priority 3: Promoting effective communication and coordination of care |
Improve the quality of care transitions and communications across care settings. Improve the quality of life for patients with chronic illness and disability by following a current care plan that anticipates and addresses pain and symptom management, psychosocial needs, and functional status. Establish shared accountability and integration of communities and health care systems to improve quality of care and reduce health disparities. |
|
|
Priority 4: Promoting the most effective prevention and treatment practices for the leading causes of mortality, starting with cardiovascular disease |
Promote cardiovascular health through community interventions that result in improvement of social, economic, and environmental factors. Promote cardiovascular health through interventions that result in adoption of the most healthy lifestyle behaviors across the lifespan. Promote cardiovascular health through receipt of effective clinical preventive services across the lifespan in clinical and community settings. |
|
|
Priority 5: Working with communities to promote wide use of best practices to enable healthy living |
Promote healthy living and well-being through community interventions that result in improvement of social, economic, and environmental factors. Promote healthy living and well-being through interventions that result in adoption of the most important healthy lifestyle behaviors across the lifespan. Promote healthy living and well-being through receipt of effective clinical preventive services across the lifespan in clinical and community settings. |
|
|
Priority 6: Making quality care more affordable for individuals, families, employers, and governments by developing and spreading new health care delivery models |
Ensure affordable and accessible high-quality health care for people, families, employers, and governments. Support and enable communities to ensure accessible, high-quality care while reducing waste and fraud. |
|
|
6. What are the main provisions of HIPAA with regard to the protection of personal health information? What provisions were added to HIPAA under the HITECH Act? |
To accelerate the adoption of EHRs, some major policy initiatives were launched during the George W. Bush administration. These initiatives culminated in the enactment of earmarked an estimated $19 billion in direct grants and financial incentives to promote the adoption of EHRs by hospitals and physicians (Wang et al. 2013). Beginning in 2011, Medicare and Medicaid started offering financial incentives of up to $44,000 for Medicare providers and $63,750 for Medicaid providers for “meaningful use” of health information technology (CDC 2012). To demonstrate “meaningful use,” health care providers have to meet a range of metrics in areas such as quality, safety, efficiency, reduction of health disparities, patient engagement, care coordination, and security of health information (Halamka 2010). Meaningful use criteria are being phased in over three stages between 2011 and 2015. To qualify for incentive payments, eligible providers must meet a set of objectives at each meaningful use stage (CMS 2013). Starting in 2015, hospitals that fail to meet the meaningful use criteria will be subject to financial penalties (DesRoches et al. 2013b).
also established the State Health Information Exchange Cooperative Agreement Program, which awarded more than $540 million to states to establish mechanisms that would facilitate the exchange of clinical information (Blumenthal 2011). One approach states are employing is to establish HIOs. |
|
|
According to the federal government, what are the components of meaningful use? |
Improve care coordination Reduce healthcare disparities Engage patients and their families Improve population and public health Ensure adequate privacy and security |
|
|
based on a group’s own medical claims experience. Under this method, premiums differ from group to group because different groups have |
experience rating |
|
|
spreads the risk among members of a larger population. Premiums are based on the utilization experience of the entire population covered by the same type of health insurance. Under pure community rating, the same rate applies to everyone regardless of age, gender, occupation, or any other indicator of health risk (Goodman and Musgrave 1992). For example, a person who has a life-threatening condition would pay the same premium as someone who does not. When premiums are based on community rating, the good risks, that is, healthy people, actually subsidize the insurance cost for the poor risks (Somers and Somers 1977). In other words, costs shift from people in poor health to people in good health and make health insurance less affordable for those who are healthy |
Community rating |
|
|
also known as modified community rating, overcomes the main drawbacks of experience rating and pure community rating. Under this method, price differences take into account demographic factors such as age, gender, geography, and family composition, while ignoring other risk factors. In the past, state laws have governed health insurance, including premium rate setting, with different states adopting one of the three methods discussed earlier. |
Adjusted community rating |
|
|
the employer acts as its own insurer instead of obtaining insurance through an insurance company. |
Self-insurance |
|
|
Resource ultilization groups (RUGs) |
This method is used for paying SNFs. Implemented in 1998, the PPS provides for a per diem prospective rate based on the intensity of care needed by patients in an SNF. The case mix is determined through a comprehensive assessment of each patient, using an assessment instrument called the Minimum Data Set (MDS). The MDS consists of a core set of screening elements used to assess the clinical, functional, and psychosocial needs of each patient admitted to an SNF. |
|
|
occurs when healthy people disproportionately enroll into a health plan |
Risk rating or favorable risk |
|
|
The leftover sum by the provider to the patient after insurance has only partially paid the charge initially billed |
balance billing |
|
|
occurs when high-risk individuals, that is, people who are likely to use more health care services than others because of their poor health status, enroll in health insurance plans in greater numbers, compared to people who are healthy |
adverse selection |
|
|
adjusting premiums to reflect health status and making potential high-cost enrollees pay more |
Risk rating |
|
|
Provisions in the ACA related to primary care include |
(1) increasing Medicare and Medicaid payments to primary care providers, (2) creating new incentives such as funding for scholarships and loan repayment for primary care providers working in underserved areas, (3) expanding the health center program and bolstering the capacity of health centers, and (4) establishing additional training programs such as establishing 11 Teaching Health Centers for training primary care providers |
|
|
8. How does hospital utilization vary according to a person’s age, gender, and socioeconomic status? |
< 1 years of age has the highest utilization, females > men, low SES.hgiher SES, western states have the lowest utilization |
|
|
a model that requires a Medicaid enrollee to choose a PCP, who is responsible for coordinating the enrollee’s care and paid a monthly fee for doing so, on top of the payment for providing medical services. In general, all medical services are reimbursed on a fee-for-service basis |
primary case management |
|
|
2. What are the three main payment mechanisms managed care uses? In each mechanism, who bears the risk? |
Fee for service: MCO Capitation: provider Discounted fees: MCO Salary: Shared (physicians bonuses tied to performance. |
|
|
does case management differ from disease management? |
Case management targets high-risk patients--those who, because of diverse combinations of health, social and functional problems, are likely to need hospitalization. Disease management targets patients who have one major diagnosis and who, because of their major diagnosis, have a relatively standard set of needs. |
|
|
What three sources do health ecomonist use to guage over spending in the US healthcare sustem? |
1. International comparisons 2. Rise of premiums 2. Spending on public programs |
|
|
What are some supply side (regulatory) cost containment strategies? |
Restrictions on capital expenditures (new construction, renovations, and technology diffusion) Example: Certificate of need Restrictions on supply of physicians Example: Entry barriers for foreign medical graduates |
|
|
NQS, Priority 1: Making care safer by reducing harm caused in the delivery of care |
Reduce preventable hospital admissions and readmissions. Reduce the incidence of adverse health care-associated conditions. Reduce harm from inappropriate or unnecessary care. |
|
|
Critical pathway |
Multidisciplinary management tool based on evidence-based practice for a specific group of patients with a predictable clinical course, in which the different tasks (interventions) by the professionals involved in the patient care are defined, optimized and sequenced either by hour (ED), day (acute care) or visit (homecare). Outcomes are tied to specific interventions. |
|
|
Priority 2: Ensuring that each person and family members are engaged as partners in their care |
Improve patient, family, and caregiver experience of care related to quality, safety, and access across settings. In partnership with patients, families, and caregivers—and using a shared decision-making process—develop culturally sensitive and understandable care plans. Enable patients and their families and caregivers to navigate, coordinate, and manage their care appropriately and effectively. |
|
|
Priority 3: Promoting effective communication and coordination of care |
Improve the quality of care transitions and communications across care settings. Improve the quality of life for patients with chronic illness and disability by following a current care plan that anticipates and addresses pain and symptom management, psychosocial needs, and functional status. Establish shared accountability and integration of communities and health care systems to improve quality of care and reduce health disparities. |
|
|
Priority 4: Promoting the most effective prevention and treatment practices for the leading causes of mortality, starting with cardiovascular disease |
Promote cardiovascular health through community interventions that result in improvement of social, economic, and environmental factors. Promote cardiovascular health through interventions that result in adoption of the most healthy lifestyle behaviors across the lifespan. Promote cardiovascular health through receipt of effective clinical preventive services across the lifespan in clinical and community settings. |
|
|
Priority 5: Working with communities to promote wide use of best practices to enable healthy living |
Promote healthy living and well-being through community interventions that result in improvement of social, economic, and environmental factors. Promote healthy living and well-being through interventions that result in adoption of the most important healthy lifestyle behaviors across the lifespan. Promote healthy living and well-being through receipt of effective clinical preventive services across the lifespan in clinical and community settings. |
|
|
Priority 6: Making quality care more affordable for individuals, families, employers, and governments by developing and spreading new health care delivery models |
Ensure affordable and accessible high-quality health care for people, families, employers, and governments. Support and enable communities to ensure accessible, high-quality care while reducing waste and fraud. |
|
|
What are the standards used in CDCs evaluation framework? |
Standard 1: utility, Standard 2: feasibility, Standard 3: propriety, and Standard 4: accuracy. |
|
|
What are the standards used in CDCs evalutation framework |
Standard 1: utility, Standard 2: feasibility, Standard 3: propriety, and Standard 4: accuracy. |
|
|
What are three groups of stakeholders identified by CDC for program evaluation ? |
those involved in program operations (e.g., sponsors, collaborators, coalition partners, funding officials, administrators, managers, and staff); those served or affected by the program (e.g., clients, family members, neighborhood organizations, academic institutions, elected officials, advocacy groups, professional associations, skeptics, opponents, and staff of related or competing organizations); and primary users of the evaluation. |
|
|
Engage stakeholdersThose persons involved in or affected by the program and primary users of the evaluation. Describe the programNeed, expected effects, activities, resources, stage, context, logic model. Focus the evaluation designPurpose, users, uses, questions, methods, agreements. Gather credible evidenceIndicators, sources, quality, quantity, logistics Justify conclusionsStandards, analysis/synthesis, interpretation, judgment, recommendations. Ensure use and share lessons learnedDesign, preparation, feedback, follow-up, dissemination |
Steps in CDCs evaluation framework |
|
|
Read about the CDC evaluation framework |
http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.361.8594&rep=rep1&type=pdf |
|
|
6. What are the main provisions of HIPAA with regard to the protection of personal health information? What provisions were added to HIPAA under the HITECH Act? |
To accelerate the adoption of EHRs, some major policy initiatives were launched during the George W. Bush administration. These initiatives culminated in the enactment of earmarked an estimated $19 billion in direct grants and financial incentives to promote the adoption of EHRs by hospitals and physicians (Wang et al. 2013). Beginning in 2011, Medicare and Medicaid started offering financial incentives of up to $44,000 for Medicare providers and $63,750 for Medicaid providers for “meaningful use” of health information technology (CDC 2012). To demonstrate “meaningful use,” health care providers have to meet a range of metrics in areas such as quality, safety, efficiency, reduction of health disparities, patient engagement, care coordination, and security of health information (Halamka 2010). Meaningful use criteria are being phased in over three stages between 2011 and 2015. To qualify for incentive payments, eligible providers must meet a set of objectives at each meaningful use stage (CMS 2013). Starting in 2015, hospitals that fail to meet the meaningful use criteria will be subject to financial penalties (DesRoches et al. 2013b).
also established the State Health Information Exchange Cooperative Agreement Program, which awarded more than $540 million to states to establish mechanisms that would facilitate the exchange of clinical information (Blumenthal 2011). One approach states are employing is to establish HIOs. |
|
|
What are the focus areas of the Partnership for Patients (safety) initiative? |
Adverse Drug Events Catheter-Associated Urinary Tract Infections Central Line Associated Blood Stream Infections Injuries from Falls and Immobility Obstetrical Adverse Events Pressure Ulcers Surgical Site Infections Venous Thromboembolism Ventilator-Associated Pneumonia Readmissions |
|
|
Module on patient safety |
http://patientsafetyed.duhs.duke.edu/module_e/module_overview.html |
|
|
Read about root-cause analysis. |
http://psnet.ahrq.gov/primer.aspx?primerID=10 |
|
|
Read about diagnostic error |
http://psnet.ahrq.gov/primer.aspx?primerID=12 |
|
|
Medication errors that do not cause any harm—either because they are intercepted before reaching the patient, or by luck |
Potential Adverse drug event |
|
|
the patient experienced harm from a medication that, while not completely preventable, could have been mitigated |
Ameliorated adverse drug rxn |
|
|
a certain percentage of patients will experience ADEs even when medications are prescribed and administered appropriately |
Non-preventable adverse drug event |
|
|
Two screening tools for prescribing safety in the eldery? |
Beers STOP/START |
|
|
contains 21 patient perspectives on care and patient rating items that encompass nine key topics: communication with doctors, communication with nurses, responsiveness of hospital staff, pain management, communication about medicines, discharge information, cleanliness of the hospital environment, quietness of the hospital environment, and transition of care. The survey also includes four screener questions and seven demographic items, which are used for adjusting the mix of patients across hospitals and for analytical purposes. The survey is 32 questions in length |
Hospital consumers assessment of Providers and systems |
|
|
Name Two patient satisfaction surveys |
Short form Patient Satisfaction survey (PSQ 18) Consumer Assessment Health plans (overseen by CMS) |
|
|
According to the federal government, what are the components of meaningful use? |
Improve care coordination Reduce healthcare disparities Engage patients and their families Improve population and public health Ensure adequate privacy and security |
|
|
an ordinal scale used to measure performance in activities of daily living (ADL). Each performance item is rated on this scale with a given number of points assigned to each level or ranking.[1] It uses ten variables describing ADL and mobility. A higher number is associated with a greater likelihood of being able to live at home with a degree of independence following discharge from hospital. The amount of time and physical assistance required to perform each item are used in determining the assigned value of each item. External factors within the environment affect the score of each item. If adaptations outside the standard home environment are met during assessment, the participant’s score will be lower if these conditions are not available |
Barthel ADL index |
|
|
What are consider instrumental ADLs? |
SHAFT: shopping, housekeeping, accounting, food preparation/meds, telephone/transportation. |
|
|
What three federally mandated assessments capture functional status? |
1)IRF Patient Assessment Instrument (hospital rehabs 2)The Home Health Outcome Outcome and Assessment Information Set (OASIS) 3) Minimum data set (for SNF, info gathered on admission and transfer to state database). |
|
|
What is disease management? |
a system of coordinated healthcare interventions and communications for populations with conditions in which patient self-care efforts are significant."[1][2][3]
For people who can access health care practitioners or peer support it is the process whereby persons with long-term conditions (and often family/friend/carer) share knowledge, responsibility and care plans with healthcare practitioners and/or peers. To be effective it requires whole system implementation with community social support networks, a range of satisfying occupations and activities relevant to the context, clinical professionals willing to act as partners or coaches and on-line resources which are verified and relevant to the country and context |
|
|
based on a group’s own medical claims experience. Under this method, premiums differ from group to group because different groups have |
experience rating |
|
|
spreads the risk among members of a larger population. Premiums are based on the utilization experience of the entire population covered by the same type of health insurance. Under pure community rating, the same rate applies to everyone regardless of age, gender, occupation, or any other indicator of health risk (Goodman and Musgrave 1992). For example, a person who has a life-threatening condition would pay the same premium as someone who does not. When premiums are based on community rating, the good risks, that is, healthy people, actually subsidize the insurance cost for the poor risks (Somers and Somers 1977). In other words, costs shift from people in poor health to people in good health and make health insurance less affordable for those who are healthy |
Community rating |
|
|
also known as modified community rating, overcomes the main drawbacks of experience rating and pure community rating. Under this method, price differences take into account demographic factors such as age, gender, geography, and family composition, while ignoring other risk factors. In the past, state laws have governed health insurance, including premium rate setting, with different states adopting one of the three methods discussed earlier. |
Adjusted community rating |
|
|
the employer acts as its own insurer instead of obtaining insurance through an insurance company. |
Self-insurance |
|
|
Resource ultilization groups (RUGs) |
This method is used for paying SNFs. Implemented in 1998, the PPS provides for a per diem prospective rate based on the intensity of care needed by patients in an SNF. The case mix is determined through a comprehensive assessment of each patient, using an assessment instrument called the Minimum Data Set (MDS). The MDS consists of a core set of screening elements used to assess the clinical, functional, and psychosocial needs of each patient admitted to an SNF. |
|
|
occurs when healthy people disproportionately enroll into a health plan |
Risk rating or favorable risk |
|
|
Fundamentally, how it is the feds or the state who are responsible for the public's health? |
States, under the 10th admendment |
|
|
What is the IOM's definition of quality? |
The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional standards |
|
|
How are need, unmet need, and utilization related? |
Unmet need = need - utilization |
|
|
National quality forum |
Panel of experts focused on developing metric. Works with AHRQ to develop adverse events reporting standards |
|
|
Public-private parternship focused on improving quality within organizations by identifying and sharing management best practices, principles, and strategies |
Baldridge program |
|
|
Non profit Creating will to change Creating new models Million lives campaign: implement bundles of improvements |
Institute for healthcare improvement |
|
|
Accrediates accountable care organizations and patient centered medical homes |
Nationals committee on quality assurance |
|
|
What is failure mode and effects analysis? |
Failure Modes and Effects Analysis (FMEA) is a systematic, proactive method for evaluating a process to identify where and how it might fail and to assess the relative impact of different failures, in order to identify the parts of the process that are most in need of change. FMEA includes review of the following:
Steps in the process Failure modes (What could go wrong?) Failure causes (Why would the failure happen?) Failure effects (What would be the consequences of each failure?) Teams use FMEA to evaluate processes for possible failures and to prevent them by correcting the processes proactively rather than reacting to adverse events after failures have occurred. This emphasis on prevention may reduce risk of harm to both patients and staff. FMEA is particularly useful in evaluating a new process prior to implementation and in assessing the impact of a proposed change to an existing process. |
|
|
What is valuable based purchasing? |
Medicare payment tied to quality metrics |
|
|
IOM dimensions of quality |
Quality care is: 1) safe-RCA and FMEA apply 2) timely/ efficient- lean or six sigma 3) pt centered - surveys and value based purchasing 4) evidence based 5) equitable |
|
|
What is a federally qualified health Center? |
Federal government repayment designation. * Create as a health care safety net to serve medically underserved populations regardless of ability to pay. * Created to free up ERs *Expansion: Health Center initiative (Bush); ACA * Medicare pts utilize (CMS doing demonstration projects on incorporating pt centered medical homes) *Non-for-profits controlled w/ board of directors |
|
|
The majority of local health departments are under the jurisdiction of what authority A) City Correct answerB) County C) Multi-county D) State |
Answer: B. According to the National Association of County and City Health Officers, 60% of local health departments fall under the jurisdiction of counties. 11% fall under combined city and county jurisdiction and another 11% fall under town and township jurisdiction. The remaining local health departments fall under multi-county district, regional or city jurisdiction |
|
|
51. A physician orders a thyroid stimulating hormone (TSH) test on a patient. The test result comes back indicating the TSH is elevated. No action is taken and the patient develops complications as a result of hypothyroidism. Which class of medical error does this represent Correct answerA) Diagnostic Error B) Equipment Failure C) Translation Error D) Misinterpretation of Medical Orders |
Answer: A. Diagnostic Errors occur when a wrong action is taken or when there is failure to take an indicated action. Other common forms of medical error include: Equipment Failure, which occurs when a specific device (such as a defibrillator or an IV pump) fails; Translation Error, which occurs when the provider and patient do not speak the same language and important clinical information such as how to take a prescribed medication is not communicated properly; and Misinterpretation of Medical Orders, which occurs when a physician order is acted upon incorrectly. (Reference is “To Err is Human,” www.nap.edu.readingroom |
|
|
91. The primary objective of utilization management is:
Correct answer: A) You chose: A)
Correct answerA) Cost containment B) Quality improvement C) Reduction of regional disparities in use of health care resources D) Regulation of health insurance industry |
Answer: A. Utilization management is a cost-containment strategy that limis health care expenditures by limiting reimbursement. It includes preadmission certification, concurrent (during admission) review, case management and disease management. It is linked to quality improvement, but quality improvement is not its primary objective. |
|
|
A patient requiring an emergency hospital stay does not have health insurance. In the months following the stay, the patient receives bills for hospital and physician services that total $10,000. In terms of health economics, these bills represent? |
A) Cost Correct answerB) Price C) Reimbursement D) Value
Answer: B. The price is what the consumer is asked to pay for a good or service. Cost is the actual monetary value of the the resources consumed in producing a good or service. Reimbursement is what the payor provides for the service. |
|
|
What offices are contained under HRSA? |
Vaccine injury compensation Bureaus of MCH/ primary care/HIV(Ryan white)/ health workforce Organ and transplant |

