![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is gout
|
Commonest Crystal arthropathies with systemic manifestations |
|
|
|
Key facts of gout and pseudogout |
Crystal arthropathies Commonly monoarticular Gout- small joints Pseudogout -large joints Assymatrical Always associated with hyperuricemia |
|
|
|
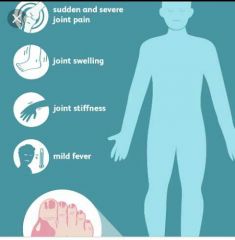
Gout clinical features |
PODAGRA other joint involvement Systemic- Fever Soft tissue tophi- ear,eyes Eyes- crystal nodules, band keratopathy, blurred vision, anterior uveitis, scleritis Urate/uric acid nephropathy
|
|
|
|
PODAGRA |
Acute Big toe inflammation Severe pain Red |
|
|
|
Gout vs pseudogout |
CF , Acute management are same But gout has more genetic aetiology Pseudogout has more sporadic aetiology Gout has a male Predominance Pseudogout is equal in both male and females
|
|
|
|
What gives rise to acute flares |
A change in serum uric acid levels (rise/decline ) |
|
|
|
What is the course of the disease |
Acute flares Progressive joint damage Development of other complications |
|
|
|
Treatment principles |
Manage acute flares - pain and inflammation Prevent recurrent flares Control uremia load |
|
|
|
What is an acute flare |
PODAGRA |

|
|
|
Management of acute flares |
NSAIDS- indomethacin Corticosteroids -prednisone Colchicine ACTH Combinations -C+N -C+C With intra-articular steroids C/C/N
|
|
|
|
Prevent recurrent flares |
Non pharmacological -prevent factors that increase uremic load Pharmacological - Colchicine Nsaids |
Risk Factors for Gout RISK FACTOR NOTES RELATIVE RISK (95% CONFIDENCE INTERVAL) Diuretic use* — 3.37 (2.75 to 4.12) Alcohol intake ≥ 50 g per day vs. none 2.53 (1.73 to 3.70) Beer ≥ 2 drinks per day vs. none 2.51 (1.77 to 3.55) Spirits ≥ 2 drinks per day vs. none 1.60 (1.19 to 2.16) Wine ≥ 2 drinks per day vs. none 1.05 (0.64 to 1.72) Hypertension — 2.31 (1.96 to 2.72) Body mass index ≥ 30 kg per m2at 21 years of age 2.14 (1.37 to 3.32) Sweetened beverage consumption ≥ 2 drinks per day vs. none 1.85 (1.08 to 3.16) Fructose intake Highest vs. lowest quintile 1.81 (1.31, 2.50) Seafood consumption Highest vs. lowest quintile 1.51 (1.17, 1.95) Meat consumption Highest vs. lowest quintile 1.41 (1.07, 1.86) Dairy product consumption Highest vs. lowest quintile 0.56 (0.42, 0.74) Vitamin C intake ≥ 1,500 mg vs. < 250 mg per day 0.55 (0.38, 0.80) Coffee consumption ≥ 6 cups per day vs. none 0.41 (0.19, 0.88) *—Adjusted for age. Adapted with permission from Roddy E, Doherty M. Epidemiology of gout. Arthritis Res Ther. 2010;12(6):223, with additional information from reference 12. Gout results from the precipitation of monosodium urate crystals in a joint space. Crystal deposition then triggers immune activation with the release of several inflammatory cytokines and neutrophil recruitment.13 Over time, the joint space can be irreversibly damaged, leading to chronic pain and disability with grossly deformed joints. Tophi (i.e., subcutaneous nodules comprised of monosodium urate crystals in a matrix of lipids, protein, and mucopolysaccharides) may also form at the joint space14(Figure 1). The first metatarsophalangeal joint is most commonly affected. Other common sites include the midtarsal joints, ankles, knees, fingers (Figure 2), wrists, and elbows. Urate crystals may also be deposited throughout the body (e.g., vertebrae, skin, soft tissues), mimicking other disease states.15 |
|
|
What is used to control uremic load |
Allopurinol - Probenecid -uricosuric agent
|
|
|
|
What are the drugs that increase serum urate load |
Aspirin Diuretics (HCT & Loop) |
|
|
|
Long term management goals |
To reduce serum urate load which has the undesirable effect of precipitating an acute flare.
|
|
|
|
How to prevent acute flares while on long term treatment |
Add NSAIDs/ Colchicine (prednisone if patients can't take the other two) |
|
|
|
What is the place of uricemic control in acute flares |
Therapy to control the underlying hyperuricemia generally is contraindicated until the acute attack is controlled (unless kidneys are at risk because of an unusually heavy uric acid load). |
|
|
|
Q1 |
WOF drugs can be successfully used to treat goutPrednisoloneAllopurinolDiclofenac sodiumFrusemideColchicine |
|
|
|
Q |
. WOF are beneficial in Rx in acute goutColchicineAllopurinolCorticosteroidsNSAIDs Febuxostat
|
|
|
|
Gout management |
Q |
|

