![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
Define dysmenorrhoea |
Difficultmenstruation
Painfulmenstrual cramps of uterine origin |
|
|
What is the incidence of dysmenorrhoea? |
Women9 – 24 peak onset
Lastsfor years after menarche Prevalenceis 75% Declineswith childbirth and oral contraceptive use Severeand disabling in 10-20% Inadolescents it is more primary dysmenorrhoea - Nounderlying pathology |
|
|
How do we classify dysmenorrhoea? |
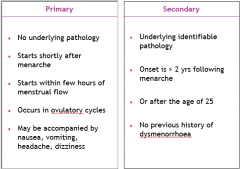
|
|
|
What is the pathophysiology of primary dysmenorrhoea? |
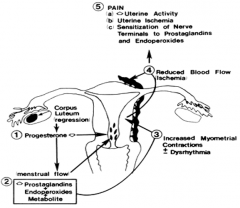
|
|
|
What are risk factors for primary dysmenorrhoea? |
Heavymenstrual flow
Age<20yrs Nulliparous Earlymenarche Smoking Obesity Strongfamily history Highlevels of stress/anxiety/ depression |
|
|
What are the clinical features of primary dysmenorrhoea? |
Shortlyafter menarche(within 6-12 months)
Ovulatorycycles Startswithin few hours of menstrual flow Cramping,spasmodic, labour like pain in lower abdomen Intensein 1st and2nd dayand lasts 2-3 days Assocwith N,V Maybe severe to interfere with daily activities |
|
|
How do we diagnose dysmenorrhoea? |
Historyalone
Bloodshave no value U/Sdone if pathology suspected |
|
|
What is the pharmacological management of dysmenorrhoea? |
Inhibit prostaglandin production and release
Effective 80-90% NSAIDs: CaboxylicAcids - Ibuprofen 400 mg 6hrly - Naproxen 500mg 6hrly - Mefenamic Acid500mg 6hrly - Indomethacin 25mg 8hrly EnoloicAcids (oxicams e.g piroxicam) Cox-2inhibitors (celebrex) - InhibitCOX I and II - Cardiovasculareffects led to their withdrawal Hormonal contraception - COC's - 2nd line treatment - Inhibitsovulation, thins the endometrium, therefore less menstrual flow, less prostaglandins - Otherhormonal treatment: subdermalimplants, DepoProvera, Mirena -Thinningof endometrium -Decreasesdysmenorrhoea -Causesamenorrhoeawithin 12 months |
|
|
What are some side effects of pharmacological treatment? |
GITulcers/GIT bleeds
Hepatotoxic Nephrotoxic Bronchospasm Haematological effects Cardiovascularadverse events (MI,stroke) –Cox-2 inhibitors |
|
|
What are some other pharmacological options? |
VitaminB6 – more effective than placebo
Vit E –2500 IU for 5days effective in 3 small trials Thiamine– 100mg daily Fishboil/Omega3 – decreased pain in swedishstudy Mgsupplements- effective than placebo Glyceryl trinitrite Transdermalnitroglycerine |
|
|
What are some non-pharmacological treatments? |
TENS– TranscutaneousElectricalNerve Stimulation
- Effective more than placebo Acupuncture – cochrane, 1small study showing effectiveness HeatTherapy – heat patch - As effective as Ibuprofen Lifestylemodification Exercise Psychologicaltherapy |
|
|
What is the surgical treatment of dysmenorrhoea? |
LUNA
- LaparoscopicUterosacralNerve Ablation - Completetransection of Uterosacralligament - Forsevere pain not responding to medical Rx LPSN - LaparoscopicPresacral Neurectomy - Disruptssensory pathway from Uterus in hypogastricnerve plexus |
|
|
What is the clinical presentation of secondary dysmenorrhoea? |
Constantdiffuse pain
Usuallyprecedes menses by several days Laststhroughout menstruation Heavymenses + pain = adenomyosis, polyps, myoma Dysmenorrhoea+ dyspareunia + infertility = endometriosis Pain+CET + fixed uterus = PID / endometriosis |
|
|
What are the extrauterine causes of secondary dysmenorrhoea? |
Endometriosis
Tumours – ovarian cysts PID Pelviccongestion syndrome –Dueto engorgement of pelvic vasculature - Hx: burning, throbbing pain at night and after standing - Dx: laparoscopic visualization ofengorged/varicosities of the broad ligament and pelvicsidewallveins Adhesions Psychogenicfactors Mulleriantract anomalies |
|
|
What are the intramural causes of secondary dysmenorrhoea? |
Adenomyosis
Leiomyoma |
|
|
What are the intrauterine causes of secondary dysmenorrhoea? |
Submucousfibroid
Polyps IUCD Cervicalstenosislinfections |
|
|
What are the non-gynaecological causes of secondary dysmenorrhoea? |
GUT
- Interstitialcystitis - Renalstones - Ureteralobstruction - Urethraldiverticulitis GIT - Irritablebowel syndrome - Diverticulitis - Bowelobstruction - Appendicitis Orthopaedic - Spondylosis - Coccydynia - Fibromyalgia |
|
|
What investigations should be done in secondary dysmenorrhoea? |
Pelvicu/s
Salinesonohysterography Urine MC&S Vaginalswab MC&S Hysteroscopy Laparoscopy |
|
|
How is secondary dysmenorrhoea treated? |
Treat the cause? |

