![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
What does it mean for someone to be Jaundiced?
What are sources of bilirubin in the body? |

Yellow discoloration of tissue (from bilirubin deposition >3.0 mg/dl). Sclera and underneath tongue = most import places.
Sources= normal RBC death (majority), destroyed RBCs, hemoproteins (myoglobin, cytochromes) |
|
|
What are the two major components of hemoglobin? What happens to each of them?
Describe the metabolism of Heme into unconjugated bilirubin? |
Heme + globin. Globin = recycled into AA. Heme = broken down into bilirubin.
Heme --> Biliverdin (via Heme oxygenase) --> Unconjugated bilirubin (via Biliverdin Reductase) |
|
|
How is bilirubin transported into the liver (be specific)?
What happens before it gets secreted into the bile canaliculi? |
Unconj bilirubin--Albumin (carrier) go into sinusoids --> pass through fenestrae --> OATP (organic anion transport protein) on hepatocyte takes it up
Bili is bound to protein in the cytoplasm (GST) - to prevent efflux back into sinusoid. Then gets conjugated (glucaronyl transferase) --> excreted into bile cannaliculus |
|
|
What is meant by "conjugation" of bilirubi n? What happens to most babies (note- they have low UGT1A1 at birth)?
What transport protein allows it to be secreted into the cannalicular system? |
Conjugated = attached to sugar moitey (GT) to help solubilize it. Facilitates excretion into bile.
UGT1A1 = gene that codes for conjugation protein. Babies have physiologic jaundice at birth. Bile binds MRP (multi-drug-resistant) transporter beofre leeaving bile cannaliculus. |
|
|
What are the two fates of CONJUGATED bilirubin?
|
Conjugated bili --> drains into duodenum.
1) can be hydrolyzed by bacteria in colon to urobilinogen --> urobilin --> stercobilin (brown) --> excreted in feces 2) can be reabsorbed in the terminal ileum (enterohepatic circulation) to be reexcreted by liver. Some amount also filters across renal glomerulus --> urobilin --> yello pee |
|
|
What is the difference between Direct and Indirect bilirubin?
If you do a dipstick test on a person who has jaundice and find that there is NO urobilinogen in the urine, what do you suspect? |
Named based on method used to measure them in serum (one is direct measurement, the other is a subtraction)
Direct = conjugated bilirubin Indirect = unconjugated (insoluble) bilirubin No urobilinogen in urine but patient is hyperbilirubinemic --> suspect Obstruction of biliary system (unable to drain bilirubin into gut) |
|
|
What are the initial 2 steps when evaluating a person with Jaundice?
|
1. Conjugated (direct) vs. Unconjugated (indirect)
2. Are other biochemical liver tests abnormal (wonder if it is a hepatocellular or choolestasis) |
|
|
If someone with Jaundice has blood tests that come back positive for Isolate Indirect (unconjugated) bilirubinemia, what is your differential?
What about if they came back with isolated direct (conjugated) bilirubinemia? |
1. Hemolytic disorder
Reduced Hepatic Clearance--> 2. Inherited (Gilber's or Crigler-Najjar) 3. Drugs (rifampin, probenacid) 4. Neonatal Jaundice (↓ UGT1A1 activity) Direct= Inherited disorders (Dubin Johnson syndrome, Rotor's syndrome) |
|
|
What are some causes of Hemolysis? What about ineffective erythropoiesis? What bilirubin lab values would you see?
|
1. Hemolysis = G6PD, shperocytosis, HUS, PNH, etc.
2. Ineffective erythropoiesis = Fe deficiency, Folate, B12, lead poisoning, porphyria. Expect ↑ INDIRECT bilirubin (overwhelming unconjugated amt) |
|
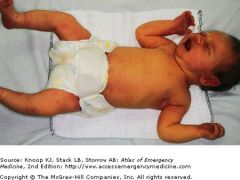
What is the cause of the syndrome shown above?
How do you treat it? |
Kernicterus --> bilirubin load is so high that it enters brain causing seizure, hearing loss, brain injury.
Why high bili? immature liver uptake, ↓ UGT1A1 activity, lack of gut flora to degrade bili. Rx= phototherapy (changes 3D structure of bili so it does not enter brain as readily) |
|
|
What drugs can cause isolated indirect bilirubin elevation? How?
|
Drugs reduce hepatic uptake of bilirubin (so it builds up in blood- unconjugated).
Ex: Rifampin, Probenacid, etc. They compete for and bind to LIGANDIN (aka GST) which usually binds to bilirubin to prevent efflux into liver sinusoids. |
|
|
Compare Crigler Najjar type I, Crigler Najjar type 2, and Gilbert's sydnrome.
Which is the most common? |
Inherited syndromes that reduce hepatic clearance of bilirubin (lead to ↑ unconjugated bili).
CN Type I = rare, AR. SEVERE. Causes jaundice and kernicterus. Undetectable UGT activity (conjugates bilirubin). CNType II= rare, AR. Rare kernicterus and asymptomatic jaundice mostly. ↓ UGT activity. Gilbert's syndrome = most common, 3-7% of population has it. Elicited by fasting or stress --> some mild sxs. Slightly ↓ UGT activity. Benign. |
|
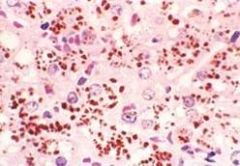
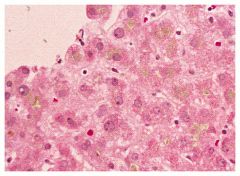
What syndrome is defined by this biopsy?
What would you find on bilirubin studies of this patient? What other syndrome can present with similar lab values? |
Dubin-Johnson Syndrome (AR mutation in MRP2 transporter- in apical membrane of cell). Causes excessive release of conjugated bilirubin into bile canaliculus. Liver looks BLACK with ↑ dark pigment.
Other syndrome = Rotor's syndrome (also AR, can cause symptomatic jaundice). Unknown molecular defect. *both have benign prognosis |
|
|
If someone with Jaundice comes back with elevated DIRECT bilirubin and other LFT abnormalities, what 2 conditions do you want to focus on?
How do you distinguish them based on the lab tests? |
Hepatocellular process (destruction of hepatocytes) vs. Cholestasis (impaired bile flow)
Hepatocellular: AL/ AST >> Alklaline Phosphatase Cholestasis : Alk Phos >> ALT/AST |
|
|
Where are AST and ALT produced? What about alkaline phosphatase?
Do elevated levels necessarily indicate liver damage? How do you confirm the liver origin of Alk Phos? |
ALT and AST both found in cytosol & AST also in mitochondria. Alk phos in microvili of bile canaliculi.
No. ALT and AST elevation may be seen in heart, muscle, or RBC injury (also found in these tissues). Alk phos is elevated in pregnant women (↑ placental production) and Children (↑bone production). Alk phos- confirm it's from liver by doing GGT, transaminases (aminotransferase) |
|
What are some hepatocellular conditions that cause elevated conjugated bilirubin and LFT abnormalities (one is shown above)?
|
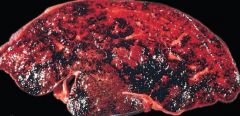
- Vascular: budd-chiari, ischemic hepatitis
- Infectious: viral hepatitis, toxins (vinyl chloride) - Autoimmune hepatitis - Metabolic: Wilson's disease (Cu2+ overload) - Iatrogenic: Drug toxicity (Tylenonl shown here, INH), Alcohol *above = budd chiari (thrombosis of hepatic vein --> blood retention in liver). |
|
|
If you saw someone with jaundice who had elevated Conjugated Bilirubin and ALT/AST > Alk Phos, what condition would you suspect?
What are two things you will need to distinguish between and what is the best way to do so? |
Cholestasis (interruption of bile secretion). Cholesterol can't be excreted either (so pts often hypercholesterolemic)
Extrahepatic cholestasis (biliary obstruction) vs. Intrahepatic cholestasis (transport protein defect) U/S, CT, MRI is useful in distinguishing this (you can see signs of extrahepatic obstruction) |
|
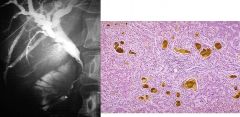
What type of LFT profile would the above condition give you ?
What are other examples of processes that cause similar LFT profiles? |
Mechanical (extrahepatic) biliary obstruction -- note stricture at common bile duct. Also bile lakes (full of bile acids) seen on histology --> these are toxic to liver cells and can --> cirrhosis.
Malignancies (cholangiocarcinoma, pancreatic/ampulla cancers, etc.). Benign conditions (PSC, liver transplants, etc.) |
|
|
What are some membrane transport defects that can lead to Cholestasis?
|
BSEP = bile salt export protein (exports bile salts into cannaliculus)
MDR3 = phospholipid excretion pump MDR1 = organic cation transporter *MRP2 = transports conjugated bile into cannaliculus (Dubin Johnson syndrome causes defective excretion). Doesn't cause excretion of cholesterol, etc. so doesn't cause cholestasis) |
|
|
What is Progressive Familial Intrahepatic Cholestasis? Compare PFIC1, PFIC2, and PFIC3?
|
Hereditary defect in bile salt transport proteins.
PFIC1 = pruritis, F1C1 transport defect (involved in phospholipid and bile salts). PFIC2 (encodes BSEP). PFIC3 = encodes MDR3, the only one that has HIGH levels of GGT. *all present with pruritis |
|
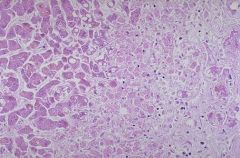
What are some drugs that case this picture?
What drugs can lead to a more severe cholestasis with hepatitis or Chronic cholestasis? |
Bland drug-induced cholestasis. No inflammatory cells, just bile retention in canaliculi. Estrogen, anabolic steroids, tamoxifen, azathioprine.
Chlorpromazine, erythromycin, NSAIDs, can all cause cholestasis with hepatisis. Chlorpromazine can also lead to chronic cholestasis. |
|
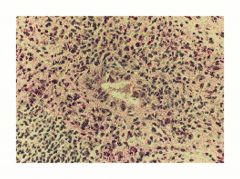
What is shown in the image above?
|
Autoimmune destruction of bile ducts (this duct is being attacked by lymphocytes). --> can interrupt bile flow.
Causes primary biliary cirrhosis. |
|
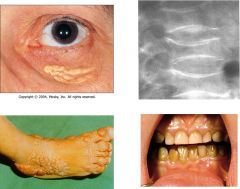
What are some complications of cholestasis (shown above)?
What vitamin deficiency syndromes can result? |
Xanthomas (from excess lipids not excreted), Pruritis (itching).
Less bile in bowel causes fat malabsorption (steatorrhea) and Vit ADEK deficiencies- Vit A= night blindness Vit D= compression fracture of spine Vit E= neuropathy Vit K= easy bruising |

