![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
What is jaundice and when is it visible?
|
Jaundice is the yellowish color to the skin due to deposition of bilirubin in the skin
Visible only after bilirubin is >5mg/dl in serum |
|
|
What is bilirubin?
|
breakdown product of RBC that is a yellow pigment
It can be neurotoxic substance to newborns if too much accumulates |
|
|
What are the risk factors for neonatal jaundice?
|
1.Males
2.vacuum/forceps delivery 3.maternal: fever/GBS status, DM, Blood type I, Rh neg 4.previous siblings with jaundice 5.excessive bruising 6.asian race 7.prematurity 8.breast feeding 9.excessive weight loss |
|
|
Is neonatal jaundice normal? Is it ever worrisome?
|
It usually occurs in 50-60% of all neonates during the 2-5th day of life
It is worriness if it occurs during the first 24 hrs |
|
|
What can indirect (unconjugated) bilirubin cause?
|
It is neurotoxic:
cerebral palsy seizures speech disorders partial deafness even death |
|
|
What is kernicterus?
|
excessive accumulation of bilirubin in the brain
(basal ganglia, hippocampal cortex, subthalamic nuclei and cerebellum) |
|
|
What causes physiologic jaundice?
|
failure of liver to dipose of normal amts of bilirubin from the breakdown of newborns RBC
This does not cause jaundice in the first day of life |
|
|
What are some criteria to exclused physiologic jaundice?
|
1.UCB>12.9mg/dl-term infant
2.UCB>15mg/dl-preterm infant 3.bilirubin levels increasing>5mg/dl/24hrs 4.jaundice in 1st 24hrs 5.CB>2mg/dl 6.clinical jaundice lasting>1wk in term infants and >2wks in preterm infants |
|
|
How does ABO incompatibility contribute to neonatal jaundice?
|
most common cause of hemolytic disease in newborns
leakage of fetal blood cells into maternal circulation which cause maternal IgA to breakdown babies RBCs |
|
|
In what percentage of pregnancies does ABO incompatibility occur and in what blood types?
|
Mother has to be type O
Fetus has to be type A or B (more common with A) This occurs in 12% of all pregnancies |
|
|
Is there a test that can check for ABO incompatibility in pts?
|
Yes, + Coombs test, but only sensitization in 3% of pregnancies
|
|
|
How does Rh incompatibility contribute to neonatal jaundice?
|
leakage of fetal blood cells into maternal circulation and mother produces Abs against D Ag on fetal blood cells
Cross the placenta barrier and cause hemolysis, which leads to anemia and jaundice |
|
|
Which is more severe, Rh or ABO incompatibility?
|
Rh is more severe, but less common because of Rhogam
|
|
|
When might Rh incompatibility occur?
|
Mother has Rh negative
Fetus has Rh positive Worsens with each pregnancy where the baby is Rh+ |
|
|
What are some non-physiological causes of jaundice?
|
breast feeding
RBC enzyme defects RBC membrane defects Inherited disorders of bilirubin metabolism |
|
|
How does breast feeding cause non physiologic jaundice?
How can you resolve the jaundice? |
two ways:
not enough breast milk (worsens with glucose water or water) Mother's enzymes deactivate babies enzymes Frequent feedings help resolve and prevent jaundice |
|
|
What are some RBC enzyme defects that cause non-physiologic jaundice?
|
G6PD (glucose 6 phosphate deficiency--may present with severe neonatal jaundice
Pyruvate Kinase deficiency-- leads to decreased lifespan of RBC and hemolysis with resulting neonatal jaundice |
|
|
What are some examples of RBC membrane defects that cause non-physiologic jaundice?
How do they cause jaundice? |
Hereditary spherocytosis
Hereditary elliptocytosis Both are related to fragile membranes of cell--leads to hemolysis and then neonatal jaundice |
|
|
What are some disease that deal with a defect in the enzyme UGT?
|
Crigler-Najar Type I(doesn't respond to phenobarbital) and II (responds to phenobarbital)
Lucy-Driscoll Syndrome Gilbert syndrome |
|
|
What does phenobarbital do?
|
induces UGT activity
|
|
|
What is lucy-Driscoll Syndrome?
How do you treat it? |
unspecified maternal gestational hormone in infants serum that interferes with conjugation of bilirubin that should be considered if siblings experience transient intense hyperbilirubinemia of unknown cause
Resolves spontaneously |
|
|
What is Gilbert's Syndrome?
How many people have this? |
A mild form of Crigler-Najar Type II.
Pt will turn yellow with stress, fatigue and illness 10-15% of the population might have this |
|
|
How do you visually detect for jaundice?
|
1.blanching skin with digital pressure to reveal underlying color of skin and subcutaneous tissue
2.progresses from head to toe 3.very dependent on experience of caregivers and pigmentation of skin 4. Visual estimations of bilirubin levels: LEAD TO ERRORS 5. usually don't see until serum bilirubin levels are 5-6mg/dl |
|
|
What is a bilimeter (TcB) and how reliable is it?
|
measures the level of bilirubin up to 12mg/dl--anything above 12mg/dl should be confirmed with a serum test
|
|
|
How does a serum bilirubin(TSB) test work?
|
requires a blood sample (can be obtained from cord blood if risk factors presents)
can be capillary or venous sample |
|
|
What is the jaundice protocol for the nursery?
|
1. asses infants at least every 8-12 hrs
2.Measure TcB/TSB for infant jaundice in 1st 24hrs 3.Measure TcB/TSB for infants with excessive jaundice for their age 4.Measure TcB/TSB if any question about jaundice levels 5.interpret all TSB and TcB according to their infant's age in HOURS |
|
|
When is bilirubin level considered abnormal?
|
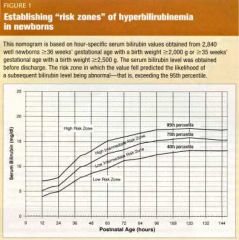
AAP published nomogram in 2004
Based on level of bilirubin and HOURS of age |
|
|
What do risk zone help with?
|
who will and won't develop hyperbilirubinemia
|
|
|
How does phototherapy work in treating jaundice?
|
Give irradiance of baby with blue-green spectrum light (430-490nm)
Deliver to as much skin as possible |
|
|
What are the risks of treating jaundice with phototherapy?
|
retinal degeneration
increased insensible fluid loss Bronze Baby syndrome (with conjugated bilirubin--causes destruction of copper porphyrins--urine and skin become bronze) Congenital erythropoietic porphyria(RARE): severe bullous lesion on exposed skin...can lead to death |
|
|
What is exchange transfusion?
When is it used? |
Removal of some of babies blood and replaced with blood without bilirubin
It is done only in the NICU or PICU and in infants that are not responding to phototherapy |
|
|
When do you discontinue treatment of phototherapy?
Is it the same with all babies? |
when bilirubin is below high risk zone and stable
That level may vary depending on baby |
|
|
Who should receive phototherapy?
|
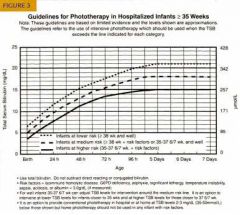
look at chart for babies >35 wks
|

