![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
17 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Nutrition Iron Sarcopenia Neuro Nephro RS CVS GI GU ENT |
Q |
|
|
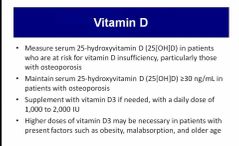
Vitamin D supplementation |
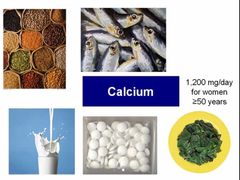
Calcium supplementation |
|
|
Q |
Q |
|
|
|
HOW TO . . . Assess for frailty The British Geriatrics Society (BGS) defines frailty as a distinctive health state related to the ageing process in which multiple body systems gradually lose their in-built reserves. Around 10% of people aged over 65 years have frailty, rising to between a quarter and a half of those aged over 85 years. It appears to be a valid construct correlating well with mortality, hospitalization, and institutionalization. Frailty is an old term that has new emphasis. It is increasingly being used within medical parlance with varying degrees of accuracy. Geriatricians have always, and should continue to embrace the concept of a holistic term that describes physical and social functioning. Scientific measurement of frailty is complex and fraught with pitfalls. Repeated studies have shown that assessment by an experienced clinician is as accurate as formalized scoring systems. Scoring systems vary from simple questionnaires (PRISMA 7), functional assessments (timed get up and go), to those approximating to the CGAs (Edmonton frailty score). These scoring systems have use within research and for triage selection of patients who would/could benefit from a multidisciplinary management approach. In an attempt to standardize this approach, the BGS is promoting FrailSafe and ‘Fit for Frailty’ campaigns. There is a push to improve identification of those at risk of frailty, with the hope of promoting healthy ageing. There is yet little evidence that this proactive approach works. Older people may object to being labelled ‘frail’, whereas relatives will often identify with the concept. Use the term judiciously. Frailty is sometimes used to justify withholding/withdrawing treatment. Once diagnosed, it should still prompt a comprehensive management plan, rather than inaction. |
Q |
|
|
|
Recurrent UTI Nitrofurantoin Trimethoprim |
Recurrent UTI 2/ MORE IN PAST 6 MONTHS OR 3 / MORE IN AN YEAR |
|
|
Sarcopenia afq034 |
|
|
|
|
|
|
|
|
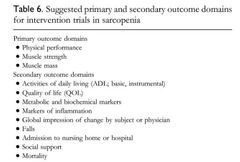
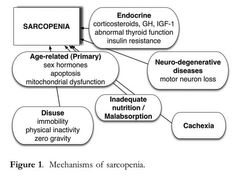
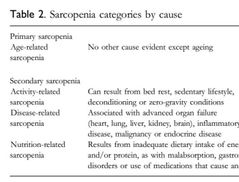
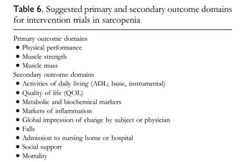
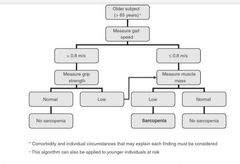
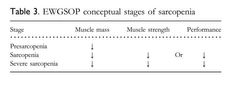
Sarcopenia Sarcopenia is a syndrome characterised by progressive and generalised loss of skeletal muscle mass and strength with a risk of adverse outcomes such as physical disability, poor quality of life and death [17, 18]. The EWGSOP recommends using the presence of both low muscle mass and low muscle function (strength or performance) for the diagnosis of sarcopenia. Thus, diagnosis requires documentation of criterion 1 plus documentation of either criterion 2 or criterion 3 ( |
|
|
|
Fraility |
Recognising frailty in a routine situationA range of tests for identifying frailty are available, but the accuracy of these is uncertain. A review was undertaken to investigate the diagnostic accuracy of some simple tests for identifying frailty. The full detail of the review is available but in summary, it searched for all studies that compared simple tests for identifying frailty (e.g. walking speed, grip strength, simple questionnaires) against a phenotype model, cumulative deficit model or comprehensive geriatric assessment.Fit for FrailtyConsensus Best Practice Guidance for the care of older people living with frailty in community and outpatient settings - published by the British Geriatrics Society and the Royal College of Nursing in association with the Royal College of General Practitioners and Age UKPart 1: Recognition and management of frailty in individuals in community and outpatient settingsNavigate toRecognising frailty in a routine situationRecognising frailty in an emergency situationRecognising frailty syndromesFrailty in the outpatient surgical settingThe review found three studies that investigated seven simple methods for identifying frailty; these were: PRISMA 7 Questionnaire. A seven item questionnaire to identify disability that has been used in earlier frailty studies and is also suitable for postal completion. A score of > 3 is considered to identify frailty.Walking speed (gait speed). Gait speed is usually measured in m/s and has been recorded over distances ranging from 2.4m to 6m in research studies. In this study, gait speed was recorded over a 4m distance.Timed up and go test (TUGT). The TUGT measures, in seconds, the time taken to stand up from a standard chair, walk a distance of 3 metres, turn, walk back to the chair and sit down.Self-Reported Health. Assessed, in the study examined, with the question 'How would you rate your health on a scale of 0-10'. A cut-off of < 6 was used to identify frailty.GP assessment. A GP assessed participants as frail or not frail on the basis of a clinical assessment.Multiple medications (polypharmacy) - where frailty is deemed present if the person takes five or more medications.The Groningen Frailty Indicator questionnaire. A 15 item frailty questionnaire that is suitable for postal completion. A score of > 4 indicates the possible presence of moderate-severe frailty.Slow walking speed (less than 0.8m/s or taking more than 5 secs to walk 4m); the PRISMA 7 questionnaire and the timed-up-and-go test (with a cut off score of 10 secs) had very good sensitivity but only moderate specificity for identifying frailty. This means that there are many fitter older people who will have a positive test result (false positives). For example, only one in three older people (over 75 years) with slow walking speed has frailty.However, the accuracy of a test is related to the prevalence of a condition in a population. For example, older people who attend outpatient clinics, receive social services assessments or require ambulance crew attendance are more likely to have frailty. This means that the tests are likely to be more accurate in these situations, which supports a case finding approach to identifying frailty. The BGS therefore recommends, as the most suitable tests, the use of gait speed (taking more than 5 seconds to walk 4 m using usual walking aids if appropriate) or the timed up and go test (with a cut off score of 10s to get up from a chair, walk 3m, turn round and sit down). The PRISMA 7 questionnaire (with a cut-off score of >3) could be considered as an alternative for self-completion, including as a postal questionnaire.Use of a two-step approach to diagnosis (for example the Prisma questionnaire followed by a gait speed test) would potentially improve accuracy but requires further investigation. Where possible, the BGS also advocates a brief clinical assessment to confirm the presence of frailty. This would help exclude some false positives (e.g. otherwise fit older people with isolated knee arthritis causing slow gait speed).It is inappropriate to use the (Rockwood) Clinical Frailty Scale (CFS) as a method of identifying frailty without a formal clinical assessment. The CFS was designed to be used to measure severity of frailty after a comprehensive geriatric assessment. It is not validated for measuring improvement in individuals after an acute illness for example. Health and social care staff will therefore need to be familiar with the tests which might be used for recognising frailty and should be trained to use them.If an older person is ill and there is reason to believe that their illness will affect their gait speed or ability to get up from a chair, the PRISMA 7 questionnaire based on their usual health status will identify those who are likely to have frailty (scoring yes to three or more questions). It can also be used for self-completion, including as a postal questionnaire.There is some evidence that grip strength (using a hand held dynamometer) may be useful in situations where it is not feasible for the patient to get up and walk. However this measurement has not yet been tested for diagnostic accuracy of frailty.In outpatient surgical settings, there is a lack of consensus on which tool should be used to identify frailty. Gait speed may help predict adverse outcomes, however, evidence is emerging for the use of the Edmonton Frail Scale 13. The strengths of this tool include brevity, clinical feasibility and identification of aspects of frailty amenable to preoperative optimisation (e.g. cognition, nutrition).Recognising frailty in an emergency situationThe presentation of an older person with frailty in an urgent situation is not always straightforward. Frailty syndromes can mask serious underlying illness and the response to a crisis call from an older person with frailty should reflect the potential underlying illness and not the symptom itself. It is not acceptable for ‘just a fall’ to be regarded as a non urgent situation without reviewing the patient in person.A health and social care professional being asked to attend an older person with frailty in an emergency situation will therefore need to act according to the clinical condition of the patient. However, prior knowledge that the person has frailty- because of access to their previously agreed care and support plans - will help make appropriate decisions. Although ideally such plans will be shared electronically, it is important always to check with the person being assessed (and their carers if appropriate) to determine if there are any care plans and advance directives in the house.Assess clinical condition: measure vital signs and consider if any red flags are present which suggest the patient needs acute hospital care - such as hypoxia, significant tachycardia or hypotension (if possible compare readings with what is usual for the patient – these should be recorded in the care and support plan). Assess current function: can they get out of bed, can they walk, have they been able to use the toilet? Is there any evidence of a frailty syndrome – falls, immobility, new onset incontinence?Are they confused: is this usual (may need help from carers to assess this) or worse than usual? The patient may have delirium even if they have a prior dementia. This would also signal frailty.If the patient is stable and at their usual level of function but has a temperature or evidence of delirium, they will need timely medical review but will not necessarily need immediate conveyance to hospital.If a patient is not severely unwell but is unable to maintain their usual status quo in the community due to a temporary change in their care needs, it is good practice and better for an older person with frailty to transfer care to a responsive community service rather than admission to hospital. This could be either a rapid response type ‘hospital at home’, or a community based intermediate care service such as a ‘step up bed’. There will be some variation in local schemes.A doctor assessing an older person with frailty as an emergency needs to strike a balance between being alert for serious underlying illness masquerading as a frailty syndrome and over medicalisation of common problems such as falls and dementia. For example, over diagnosis of urinary tract infection as a single cause for falls, immobility and delirium in older people with frailty is common and a judicious clinical assessment is required. If in doubt (i.e. the patient is not febrile and appears to be otherwise well) then a set of bloods to look for raised inflammatory markers should be done without necessarily conveying the patient to hospital.There are many national guidelines on managing these problems; for example SIGN guidance for diagnosing UTI 18 and there should be local protocols which direct people to the local alternative for hospital admission. Recognising frailty syndromesSometimes frailty means that individuals can present with what appears to be a straightforward symptom masking a more serious or complex underlying medical problem. This gives rise to the concept of ‘frailty syndromes’ (previously known as the geriatric giants).Broadly there are five frailty syndromes and encountering one of these should raise suspicion that the individual concerned has frailty:Falls (e.g. collapse, legs gave way, ‘found lying on floor’).Immobility (e.g. sudden change in mobility, ‘gone off legs’ ‘stuck in toilet’).Delirium (e.g. acute confusion, ’muddledness’, sudden worsening of confusion in someone with previous dementia or known memory loss).Incontinence (e.g. change in continence – new onset or worsening of urine or faecal incontinence).Susceptibility to side effects of medication (e.g. confusion with codeine, hypotension with antidepressants).However, it is possible to have any of these problems without frailty and sometimes there can be a very straightforward explanation for the problem. Nonetheless, frailty can mean, for example, that myocardial infarction, stroke, pneumonia or even spinal cord compression due to infection could all manifest themselves in a patient with frailty as a sudden change in mobility. Likewise a fall could indicate serious underlying illness and it will not be possible to make this decision without reviewing the patient (see above: Recognising frailty in an emergency situation.Frailty in the outpatient surgical settingIncreasing numbers of older people are undergoing elective surgery. Studies examining older patients undergoing elective procedures have reported frailty prevalence of 40-50 per cent.Frailty is an independent risk factor for post-operative major morbidity, mortality, protracted length of stay and institutional discharge.It is important to identify frailty preoperatively in order to manage risk, inform shared decision making and highlight areas for potential modification.Whilst there is a lack of consensus on which tool should be used to identify frailty in surgical settings, as noted above, evidence is emerging for the use of the Edmonton Frail Scale. The strengths of this tool include brevity, clinical feasibility and identification of aspects of frailty amenable to preoperative optimisation (e.g. cognition, nutrition). Furthermore, the association of preoperative gait velocity with postoperative morbidity and mortality makes this a potentially useful frailty measure in the elective pre-operative setting.There are no proven strategies for pre-operative management of frailty in surgical patients, however there is increasing evidence for exercise, nutritional and multi-component interventions to improve outcomes in this group 19. The translation of such approaches into routine clinical care requires close collaboration between surgeons, anaesthetists and geriatricians working as part of a multidisciplinary team. Examples of such working include proactive care of older people undergoing surgery and systematic care of older people undergoing elective surgery. This will need to be factored into the commissioning of surgical pathways and has significant policy implications but has been endorsed by the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) and the British Geriatrics Society (BGS). |
|
|
|
Q |
Q |
|
|
|
Q |
Q |
|
|
|
What is ICOPE |
Q |
|
|
|
Social services functions |
Q |
|
|
|
Previlages to elderly |
Q |
|
|
|
Q |
Q |
|
|
|
Assistive devices Mobility |
Q |
|
|
|
Falls FallsThis page give the background and potential complications of patients who present with a fall. Ideal revision for medical student OSCEs and PACESBackground to fallsFalls are one of the “Geriatric Giants”.Falls are a frequently encountered presentation or referral both to the emergency department and also to GP/rapid access clinics, but are commonly – and at times mistakenly – diagnosed as a “mechanical fall”.As with all aspects of geriatric care, falls should ideally receive a comprehensive assessment to ensure that any modifiable underlying risk factor has been identified and, if possible, corrected. Epidemiology of fallsThe rate and incidence of falls both increase with age, as multiple background co-morbidities combine to increase risk.30% of the over-65 year-old population will have at least one fall per year, rising to 50% in over-80s.Estimated cost to the NHS of more than £2.3 billion per year in 2015Greater emphasis should perhaps be placed on falls prevention, but as it is often only following a fall that a patient comes to the attention of health services, it justifies the comprehensive assessment into any patient who presents with a fall, as this may go some way to help prevent future incidents. |
Complications following a fallFall complications are not only physical (bumps, bruises, broken bones) but also psychological.PhysicalImmediateFractured neck of femur (#NOF)One of the most serious (but common) injuries experienced by patients who suffer a fall is a fractured neck of femurA fractured NOF leads to a relative increase in mortality at 3 months post-injury of 5.75 in older women, and 7.95 in older men.Other fractures (e.g. radius/humerus)Soft tissue injury (and skin breaks)DelayedImmobilityVTE and PEPressure ulcerationIncontinenceA reduction in mobility following a fall (as a result of either physical or psychological disability) can also lead to issues with incontinenceThis in turn can cause both physical and psychological complications.PsychologicalThe incidence of a fear of falling doubles in patients who have suffered a previous fall.That fear of falling itself also correlates with both an increased risk in future fall, but also a lower quality of life and higher mortality.As such, the importance of not being dismissive of any patient who has fallen cannot be emphasised enough. |
|

