![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
16 Cards in this Set
- Front
- Back
|
Define UGIB |
Upper GI bleed is bleeding arising from the oesophagus, stomach or duodenum proximal to the ligament of Trietz. |
|
|
What is massive Upper GI bleed |
Massive Upper GI bleed is when the loss of blood (arising from the oesophagus, stomach or duodenum proximal to the ligament of Trietz,) is great enough to produce 1. signs of hypotension (such as *loss of consciousness or *shock with Systolic BP <100mmHg, HR >100/min) or 2. necessitate the transfusion of ≥ 3 units of blood. |
|
|
UGIB Vs LGIB which is more common? By how much? |
Upper GI bleed is 4 x More common than LGIB |
|
|
Causes of UGIB can be? |
1. Esophageal causes 2. Gastric causes 3. Duodenal causes 4. Other causes |
|
|
Causes of UGIB can be? List these causes |
1. Oesophageal Causes - Oesophageal Varices - Oesophagitis - Barret’s Ulcer/Oesophagus - Oesophageal Erosions - Oesophageal Cancer - Mallory-Weiss Syndrome (Oesophageal tear) - 2. Gastric Causes - Gastric Ulcer/PUD – The commonest cause of Upper GI bleed (27% - 40%) - Gastric Erosions eg NSAIDs Induced; Aspirin; Steroids; - Gastric Cancer - Gastric Varices (Oesophago-gastric Varices) - Gastric Antral Vascular Ectasia (GAVE) - Dieulafoy’s lesions (Gastric Vascular Malformations) - Gastritis - GIST (Gastrointestinal Stromal Tumours) 3. Duodenal Causes: - Duodenal Ulcer - Aorto-duodenal (Aorto-enteric) fistula - Haemobilia 4. Other Causes: - Pancreatic Pseudoaneurysm - Bleeding Diathesis eg Von-Willebrand disease, DIC. - Haemosuccus Pancreaticus (Bleeding from the Pancreatic Duct) |
|
|
The commonest cause of Upper GI bleed |
Gastric Ulcer/PUD 27% - 40% |
|
|
Symptoms and signs of UGIB |
*Asymptomatic – Incidental diagnosis (Few/non-acute cases) eg Unexplained Anaemia. *Acute cases seen in ER or Wards: 1. Haematemesis: 40 – 50% of UGIB (Higher Mortality); 2. Melaena: 70 -80%. NOTE: Iron & Bismuth (Colloidal Bismuth) may mimic Melaena!!! 3. Haematochezia: 15 – 20%; 4. Syncope: 14.4%; 5. Dyspepsia *Other symptoms depend on the cause 6. Epigastric pain/heartburn – assd with PUD; 7. Weight loss, dysphagia & LNs – Upper GI Malignancy; 8. Jaundice, Gynaecomastia, Ascitis, Flapping Tremors; Spider Naevi etc – Portal Hypertensive 9. Gastropathy & Varices : With History of Alcohol Abuse 10. Preceding hx of Vomiting & retching – Mallory Weiss tear or Boarhaave (with subcutaneous emphysema). 11. Investigations fBleeding from other orifices (Nose, Haematuria etc) – DIC or Bleeding Diathesis |
|
|
Investigations for LGIB. The Primary diagnostic tool of choice in UGIB is? Discuss its place in UGIB
|
1. OGD – -undertaken after Resuscitation (Unstable patients); - within 24hrs of presentatn (all others); - may offer therapeutic opportunity ( *Stenting *Adrenaline Inj, *Clips application, *Thermal coagulation, *banding, *Inj msclerotherapy, *Balloon Tamponade using either Minnesota Tube or Sengstaken-Blakemore Tube, or Linton-Nachlas Tube; *Laser Ablation of bleeding tumours, etc). |
|
|
Investigation for UGIB |
1. OGD 2. CT Angiography – *failed endoscopic diagnosis; Tumours; *Aoto-enteric fistulae, *Pancreatic pseudoaneurysms, liver ds 3. NM (Nuclear Medicine) Scans – identifies areas of active bleeding using radioactive labelled RBCs; 4. Percutaneous Selective Angiography & Transcatheter Embolization – *Provides diagnosis of site of bleed if OGD fails; *Also Rxtic eg in Haemobilia 5. CXR (PA view) – *Boarhaave’s Syndrome; *Perf viscus, *Aspiratn, *Pleural effusion, *pneumonia. 6. Clotting Profile (INR, APTT, Fibrinogen level + Platelet count) in Bleeding diathesis. 7. LFT – In Portal Hypertension from liver cirhhosis (with varices)
B. To assess extent of the disease: 1. FBC – For PCV
C. To Manage the Patient 1. Group & X-match 2. FBS 3. RVS 4. S/E/U/Cr 5. Urinalysis |
|
|
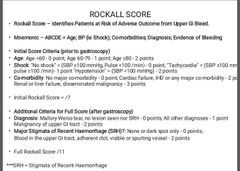
What scoring system is used in UGIB |
Rockall Score. Identifies Patients at Risk of Adverse Outcome from Upper GI Bleed. |
|
|
What is the mnemonic for Rockall score |
ABCDE 1. Age; 2. BP (ie Shock); 3. Co-morbidities; 4. Diagnosis; 5. Evidence of Bleeding |
|
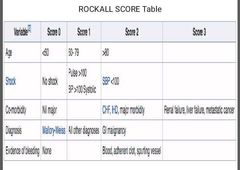
Discuss the Rockall score |
|
|
|
Discuss the interpretation of the Rockall score |
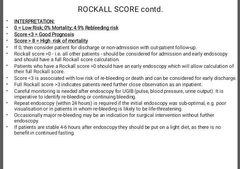
|
|
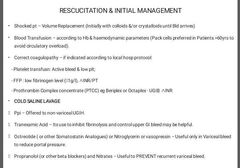
Treatment of UGIB |
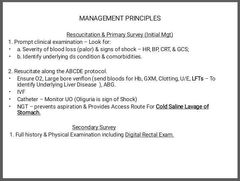
A. Rescucitation & Primary Survey (Initial Mgt) 1. Prompt clinical examination – Look for: a. Severity of blood loss (palor) & signs of shock – HR, BP, CRT, & GCS; b. Identify underlying ds condition & comorbidities. 2. Resucitate along the ABCDE protocol. *Ensure O2, Large bore venflon (send bloods for Hb, GXM, Clotting, U/E, LFTs – To identify Underlying Liver Disease ), ABG. *IVFCatheter – Monitor UO (Oliguria is sign of Shock) *NGT – prevents aspiration & Provides Access Route For Cold Saline Lavage of Stomach.
Secondary Survey 1. Full history & Physical Examination including Digital Rectal Exam. *Shocked pt – Volume Replacement (Initially with colloids &/or crystalloids until Bld arrives) *Blood Transfusion – according to Hb & haemodynamic parameters (Pack cells preferred in Patients >60yrs to avoid circulatory overload). *Correct coagulopathy – if indicated according to local hosp protocol: - Platelet transfusn: Active bleed & low plt; - FFP : low fibrinogen level (<1g/l), ∧INR/PT - Prothrombin Complex concentrate (PTCC) eg Beriplex or Octaplex - UGIB + ∧INRCOLD SALINE LAVAGEPpi – Offered to non-variceal UGIH. Tranexamic Acid – Its use to inhibit fibrinolysis and control upper GI bleed may be helpful. *Octreotide ( or other Somatostatin Analogues) or Nitroglycerin or vasopressin – Useful only in Variceal bleed to reduce portal pressure. Propranolol (or other beta blockers) and Nitrates – Useful to PREVENT recurrent variceal bleed. |
|
|
INDICATIONS FOR SURGICAL TREATMENTOf UGIB |
1. Severe life-threatening (Massive) UGIB not responsive ie UGIH Refractory to Rx 2. Failed medical & minimally invasive therapies; 3. Presence of coexisting reasons for surg (eg bowel perf, obstructn or malignancy); 4. 2nd hospitalization for Peptic Ulcer Hge; 5. Prolonged UGIB with loss of ≥50% patient’s bld vol.
NOTE: Transjugular Intrahepatic Portosystemic Shunt (TIPSS) is a Minimally Invasive Procedure reserved for Variceal bleed after controlling the acute episode with Sengstaken-Blakemore tube or Minnesota tube. |
|
|
Complications of UGIB |
1. From UGIB – Self evident 2. From Medical Treatment Given including Use of blood products: 3. From Endoscopy – Iatrogenic Perf; Further bleeding, Aspn. 4. From Interventional Radiology – Bowel Ischaemia, Bowel Perf, limb gangrene/loss, Blood vessel Injury/disection/rupture/thrombosis 5. From Surgery – Ileus, Wound sepsis, DVT, PE, Chest Complications, etc |

