![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
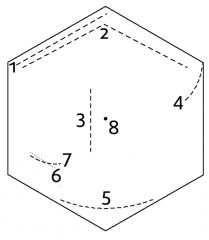
scars |
1. Kocher: right subcostal - Open cholecystectomy, liver resection, biliary surgery; Left subcostal (reverse Kocher's) - open splenectomy 4. Nephrectomy (renal surgery) 5. Pfannenstiel (Caesarean) 6. Gridiron (appendicectomy) 7. Lanz (appendicectomy) 8. Laparoscopic around umbilicus |
|
|
causes of iron deficiency anaemia |
Reduced iron absorption - Coeliac disease, duodenal bypass, poor diet |
|
|
Clinicalsigns of chronic iron deficiency |
Pallor Koilonychias |
|
|
causes of UGI haemorrhage |
Peptic ulcer - duodenal / gastric |
|
|
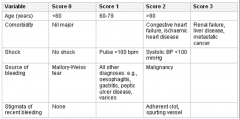
variables influencing mortality from UGI haemorrhage (Rockall score) |
Age stigmata of recent bleeding |
|
|
The Rockall score |
|
|
|
Components of the Blatchford score (indication for intervention in upper GI bleeding) |
BP Heart rate Haemoglobin Urea Melena Syncope Hepatic disease Heart failure |
|
|
management of oesophageal varices |
Fluids, blood products (if Hb<7), antibiotics, terlipressin PPI post endoscopy |
|
|
causes of dysphagia |
Carcinoma of oesophagus and stomach Achalasia neurological problems |
|
|
achalasia, assessment & management |
loss of peristalsis in the distal oesophagus and a failure of lower oesophageal sphincter relaxation with swallowing. Causes dysphagia of solids ± liquids . Assess with manometry. Surgical management - myotomy |
|
|
what causes benign strictures of the oesophagus? |
gastroesophageal reflux |
|
|
causes of dyspepsia |
Non-ulcer dyspepsia |
|
|
presentation of conjugated hyperbilirubinaemia |
Dark urine, pale stools |
|
|
management of cholecystitis (gallstone in cystic duct) |
Give fluids, analgesia, antibiotics (antibiotics are typically given until cholecystectomy despite sterile inflammation) |
|
|
risks of Cholecystectomy |
bleeding, bile leak, abscess, bowel injury, biliary injury, infection |
|
|
Presentation of bile duct injury |
Abdominal pain, persistent nausea and vomiting, and low grade fever |
|
|
management of bile leak |
ABC: oxygen, IV fluids, analgesia & antibiotics
urgent USS + drain bile MRCP CT angiogram to assess blood supply to bile duct Surgical repair with hepaticojejunostomy |
|
|
Charcot’s triad for ascending cholangitis |
right upper quadrant pain |
|
|
Blood test abnormalities in cholangitis |
Raised WCC, raised ALP, raised GGT, and raised bilirubin |
|
|
approach to cholangitis |
Fluids, analgesia, antibiotics |
|
|
complications of ERCP |
Pancreatitis Bleeding Perforation |
|
|
causes of acute colitis |
ulcerative colitis |
|
|
presentation of acute colitis |
diarrhoea and often lower abdominal pain, and blood and mucus per rectum. |
|
|
antibiotic management of c. diff |
Vancomycin PO for 14 days + metronidazole if severe |
|
|
diagnosis of coeliac disease |
1. positive immunoglobulin A tissue transglutaminase serology (TTGA IgA) 2. duodenal biopsy and histology (Villous atrophy, crypt hyperplasia,lymphocyte infiltration of lamina propria) NB. patient should keep eating gluten until biopsy |
|
|
causes of acute pancreatitis |
Gallstones (30-50%) |
|
|
Glasgow Imrie Criteria for acute pancreatitis prognosis |
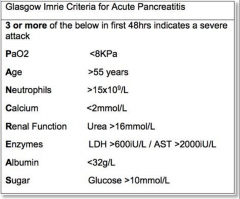
|
|
|
management of acute pancreatitis |
1. acute treatment: analgesia, IV fluids, correct electrolytes, control glucose, PPI 2. assess severity 3. nutrition: oral feeds asap; if not possible, start enteral feeding (NG/NJ) / parenteral 4. Consider cause - stop alcohol, assess for gallstones (USS/MRCP), ERCP + biliary sphincterotomy 5. if not improving, CT scan for complications |
|
|
complications of acute pancreatitis & their management |
Shock → IV fluids Extrapancreaticinfection→ antibiotics Pancreatic pseudocyst / abscess → percutaneous drainage Pancreatic necrosis → operative resection DIC → blood products |
|
|
investigations for chronic pancreatitis |
Normal amylase |
|
|
complications of diverticulitis |
abscess |
|
|
management of uncomplicated diverticulitis |
IV antibiotics - co-amoxiclav + metronidazole analgesia allow eating and drinking |
|
|
causes of small bowel obstruction |
adhesions, hernia |
|
|
causes of large bowel obstruction |
tumours |
|
|
complications of colostomy formation |
retraction |
|
|
complications of oesophagectomy |
postoperative pulmonary complications anastomotic leak |
|
|
risks of gastrectomy |
Obstruction |
|
|
causes of acute hepatitis |
1. Drugs 2. Viral (A, B, E, EBV) 3. Alcohol (ALT < 250) 4. Autoimmune Others: leptospirosis, ischaemic, pregnancy, SLE, Wilson's disease, Toxins |
|
|
diagnosis of hepatitis B via antibody/antigen tests |
Acute infection: HBsAg & anti-HBc IgM viral replication & raised infectivity: HBeAg & HBV DNA |
|
|
evidence for hepatitis B vaccination |
anti-HBs antibody alone |
|
|
diagnosis of hepatitis C infection |
Anti-HCV antibody (accurate after 3 months) |
|
|
treatment of hepatitis C |
sofosbuvir / ledipasvir |
|
|
autoantibodies in autoimmune hepatitis |
ANA & anti-smooth muscle |
|
|
diseases associated with autoimmune hepatitis |
Pernicious anaemia |
|
|
treatment of autoimmune hepatitis |
Steroids ± azathioprine. 80% respond 20% develop chronic liver disease |
|
|
causes of chronic liver disease |
Alcoholic liver disease |
|
|
causes of decompensation in chronic liver disease |
Drugs Sepsis, especially SBP GI bleed Hepatoma |
|
|
pathophysiology in primary biliary cholangitis |
Granulomatous inflammation in the small interlobular bile ducts (cause unknown) → progressive fibrosis → cirrhosis |
|
|
presentation of primary biliary cholangitis |
AMA+ Chronic, progressive, intrahepatic cholestasis - Pruritus, Lethargy, Fatigue, Steatorrhoea, Vitamin deficiency (A, D and K) |
|
|
management of primary biliary cholangitis |
1. Treat complications of the disease 3. liver transplantation |
|
|
presentation of primary sclerosing cholangitis |
Abnormal LFTs - ↑ALP |
|
|
presentation of haemochromatosis |
"Bronzed diabetes" - pigmentation diabetes mellitus Arthropathy impotence in males Cardiac enlargement ± heart failure or conduction defects |
|
|
complications of alcoholic cirrhosis |
ascites development |
|
|
assessment of ascitic fluid |
WBC count ≥ 500 cells/mm3 suggests SBP Neutrophil count ≥ 250 cells/mm3 suggests SBP Serum-ascites albumin gradient |
|
|
treatment of SBP |
IV antibiotics (ceftriaxone 2g OD) + IV albumin |
|
|
management of hepatic encephalopathy |
1. high calorie diet and no protein restriction 2. correct precipitating factors 3. lactulose 4. rifaximin |
|
|
complications of endoscopy |
bleeding - especially after biopsy perforation of gut damage to teeth reaction to sedation - vomiting, breathing difficulties aspiration pneumonia sore throat |
|
|
physical signs of abdominal peritonitis |
guarding board-like rigidity rebound tenderness decreased bowel sounds hypotension, tachycardia |
|
|
protocol for antibiotic prophylaxis at GI and biliary surgery |
give IV antibiotics at induction, ideally within 60 mins prior to skin incision -co-amoxiclav + metronidazole give single dose unless significant bleed/fluid loss give further intra-operative co-amoxiclav if surgery >3hrs |
|
|
causes of a raised amylase |
pancreatitis perforated peptic ulcer ischaemic bowel renal failure salivary gland inflammation |
|
|
presentation of appendicitis |
migratory RIF pain |
|
|
differential of appendicitis |
viral gastroenteritis Meckel's diverticulitis Crohn's disease peptic ulcer disease ureteric stone cholecystitis UTI pelvic inflammatory disease ectopic pregnancy ovarian torsin ruptured Graafian follicle |
|
|
Rovsing's sign |
RIF>LIF pain when LIF palpated |
|
|
complications of appendectomy |
wound infection intra-abdominal abscess - pelvic, RIF, subphrenic adhesions portal pyaemia abdominal actinomycosis |
|
|
causes of acute lower GI haemorrhage |
diverticular change colonic angiodysplasia ischaemic colitis distal colon / rectal carcinoma IBD |
|
|
causes of chronic LGI bleeding |
cancer angiodysplasia polyp colitis haemorrhoids |
|
|
causes of bright red rectal bleeding
|
haemorrhoids - painless (unless prolapsed & thrombosed) fissure - painful diverticular disease - painless |
|
|
causes of blood mixed with stool |
colon and rectal cancer - usually painless ulcerative colitis - blood & mucus mixed with loose stool, painless |
|
|
two common organisms responsible for intra-abdominal infections |
Bacteroides fragilis and E. coli |
|
|
adverse effects of PPIs |
Diarrhoea Headache Abdominal pain Interstitial nephritis (rare) Osteoporosis if prolonged use |
|
|
presentation of pancreatic cancer |
Jaundice, abdominal pain and weight loss palpable gallbladder back pain, anorexia, steatorrhea new onset diabetes |
|
|
Indications for urgent direct access upper gastrointestinal endoscopy (to be performed within 2 weeks) to assess for oesophageal cancer |
1. dysphagia or 2. aged >55 + weight loss and any of the following: A. upper abdominal pain B. reflux C. dyspepsia |
|
|
Indications for non‑urgent direct access upper gastrointestinal endoscopy to assess for oesophageal cancer in people aged 55 or over |
1. treatment‑resistant dyspepsia 2. upper abdominal pain with low haemoglobin levels 3. raised platelet count with any of the following: nausea, vomiting, weight loss, reflux, dyspepsia, upper abdominal pain 4. nausea or vomiting with any of the following: weight loss, reflux, dyspepsia, upper abdominal pain. |
|
|
Local complications of UC |
Fulminant colitis toxic dilation & perforation haemorrhage stricture malignant change perianal disease |
|
|
Classification of UC |
S0: clinical remission (asymptomatic) S1 (mild UC): ≤4 stools per day (+/-blood), no systemic illness, normal ESR S2 (moderate UC): >4 stools per day but minimal signs of systemic toxicity S3 (severe UC): ≥6 bloody stools daily, HR ≥ 90 bpm, T ≥ 37.5°C, Hb <10.5 g/dL, ESR ≥ 30 |
|
|
Treatment for mild to moderate and subacute UC |
topical or oral aminosalicylate/steroids Azathioprine infliximab/adalimumab |
|
|
Induction of remission for acute severe UC (≥6 bloody stools daily, HR ≥ 90 bpm, T ≥ 37.5°C, Hb <10.5 g/dL, ESR ≥ 30) |
1. IV steroids + IV ciclosporin or infliximab if not improving by day 3 2. Surgery, if not improving by day 5-7 - segmental colectomy or total colectomy with ileostomy or ileal pouch-anal anastomosis |
|
|
Indications for surgery in UC |
Acute severe UC not improving Colonic dilatation chronic symptoms complications of medical therapy delayed growth (adolescents) |
|
|
Complications of Crohn's disease |
fistulae Strictures malabsorption - steatorrhoea, vitamin deficiency |
|
|
Induction of remission in Crohn's disease |
1. Steroids ± azathioprine/methotrexate (if severe) 2. If steroids not tolerated, consider budesonide or 5-ASA treatment (mesalazine) 3. If poor response / intolerance, consider infliximab / adalimumab |
|
|
Maintenance of remission in Crohn's disease |
1. no treatment, advise re relapse symptoms 2. Azathioprine / methotrexate |
|
|
Surgical options in Crohn's disease |
Surgery can be alternative to early medical management if disease is limited to distal ileum Surgery can manage strictures, severe or recurrent obstructive symptoms, & treat fistulae into bladder/skin |
|
|
Presentation of colorectal carcinoma |
Rectal bleeding Change in bowel habit Abdominal mass iron deficiency anaemia Obstruction |
|
|
Features of abdominal pain in IBS |
recurrent - at least once weekly Related to defecation Associated with a change in stool frequency Associated with a change in stool form (appearance) |
|
|
Triple therapy for gastric ulcer with H. pylori infection |
PPI (omeprazole) + amoxicillin/metronidazole PO + Clarithromycin PO for 7 days |

