![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
What fluid/non-fluid compartments can the total body weight be divided into (what percentages)? |
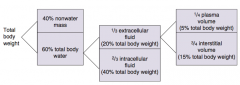
- 40% non-water mass
- 60% total body water |
|
|
What fluid compartments can the total body water be divided into? What percent of total body weight?
|
- 1/3 extracellular fluid (20% total body weight)
- 2/3 intracellular fluid (40% total body weight) |
|
|
What fluid compartments can the extracellular fluid be divided into? What percent of total body weight?
|
- 1/4 plasma volume (5% total body weight)
- 3/4 interstitial volume (15% total body weight) |
|
|
What is the "rule" to remember the % of body weight of the different fluid compartments?
|
60:40:20 rule:
- 60% total body water - 40% ICF - 20% ECF |
|
|
How do you measure the plasma volume?
|
Radio-labeled albumin
|
|
|
How do you measure the extracellular volume?
|
Inulin
|
|
|
What is the normal serum osmolarity?
|
290 mOsm/L
|
|
|
What is the glomerular filtration barrier composed of? What does each layer restrict?
|
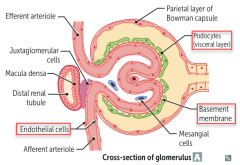
- Fenestrated capillary endothelium (size barrier)
- Fused basement membrane with heparan sulfate (negative charge barrier) - Epithelial layer consisting of podocyte foot processes |
|
|
What happens to the glomerular filtration barrier in nephrotic syndrome? Consequences?
|
Charge barrier (fused basement membrane with heparan sulfate) is lost in nephrotic syndrome, results in:
- Albuminuria - Hypoproteinemia - Generalized edema - Hyperlipidemia |
|
|
How do you calculate renal clearance?
|
Volume of plasma from which the substance is completely cleared per unit time
Cx = (Ux * V) / Px Cx = Clearance of X (mL/min) Ux = Urine concentration of X (mg/mL) Px = Plasma concentration of X (mg/mL) V = urine flow rate (mL/min) |
|
|
What does it tell you if the clearance of a substance is less than the GFR?
|
Net tubular reabsorption of X
|
|
|
What does it tell you if the clearance of a substance is greater than the GFR?
|
Net tubular secretion of X
|
|
|
What does it tell you if the clearance of a substance is equal to the GFR?
|
No net secretion or reabsorption
|
|
|
What can be used to calculate the GFR? Why?
|
Inulin clearance because it is freely filtered and is neither reabsorbed nor secreted (C-inulin = GFR)
GFR = (U-inulin * V) / P-inulin U-inulin = Urine concentration of inulin (mg/mL) P-inulin = Plasma concentration of inulin (mg/mL) V = urine flow rate (mL/min) |
|
|
How can you calculate GFR based on the pressures in the glomerulus and Bowman's capsule?
|
GFR = Kf [ (P-gc - P-bs) - (π-gc - π-bs) ]
P = hydrostatic pressure π = oncotic pressure gc = glomerular capillary bs = bowman's space π-bs usually equals zero (protein shouldn't be in bowman's space) |
|
|
What is a normal GFR?
|
~100 ml/min
|
|
|
Clearance of what can estimate GFR?
|
Creatinine clearance is an approximate measure of GFR; slightly overestimates GFR because creatinine is moderately secreted by the renal tubules
|
|
|
What is the staging of chronic kidney diseases based on?
|
Incremental reductions in GFR
|
|
|
How do you estimate the Effective Renal Plasma Flow (ERPF)?
|
Estimated using para-aminohippuric acid (PAH) clearance because it is both filtered and actively secreted in the proximal tubule; nearly all PAH entering the kidney is excreted
ERPF = (U-pah * V) / P-pah Underestimates the true renal plasma flow (RPF) by ~10% |
|
|
How do you determine the renal blood flow?
|
RBF = RPF / (1 - Hct)
RPF is estimated by ERPF = (U-pah * V) / P-pah |
|
|
What are the characteristics of para-aminohippuric acid (PAH) in the kidney?
|
- Both filtered and actively secreted in proximal tubule
- Nearly all PAH entering the kidney is excreted |
|
|
How do you calculate the filtration fraction? What is normal?
|
FF = GFR / RPF = normally 20% |
|
|
How do you calculate the filtered load?
|
Filtered load (mg/min) = GFR (ml/min) * plasma concentration (mg/ml)
|
|
|
How do NSAIDs affect the filtration at the glomerulus?
|
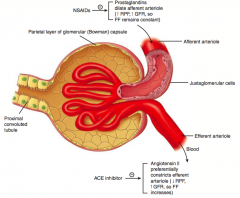
NSAIDs inhibit prostaglandins, preventing dilation of the afferent arteriole
- ↓ RPF, ↓ GFR, so Filtration Fraction remains constant (remember FF = GFR/RPF) |
|
|
How do prostaglandins affect the filtration at the glomerulus?
|
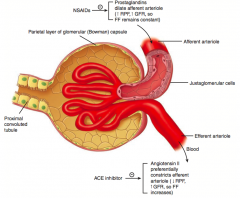
Prostaglandins dilate the afferent arteriole |
|
|
How do ACE-inhibitors affect the filtration at the glomerulus?
|
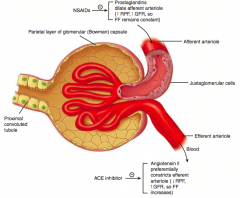
ACE-I inhibit AngII, preventing constriction of the efferent arteriole
- ↑ RPF, ↓ GFR, so FF decreases (remember FF = GFR/RPF) |
|
|
How does Angiotensin II affect the filtration at the glomerulus?
|
AngII preferentially constricts the efferent arteriole
- ↓ RPF, ↑ GFR, so FF increases (remember FF = GFR/RPF) |
|
|
How does afferent arteriole constriction affect RPF, GFR, and FF (GFR/RPF)?
|
- ↓ RPF |
|
|
How does efferent arteriole constriction affect RPF, GFR, and FF (GFR/RPF)?
|
- ↓ RPF
- ↑ GFR - ↑ FF |
|
|
How does ↑ plasma protein concentration affect RPF, GFR, and FF (GFR/RPF)?
|
- = RPF
- ↓ GFR - ↓ FF |
|
|
How does ↓ plasma protein concentration affect RPF, GFR, and FF (GFR/RPF)?
|
- = RPF
- ↑ GFR - ↑ FF |
|
|
How does constriction of the ureter affect RPF, GFR, and FF (GFR/RPF)?
|
- = RPF
- ↓ GFR - ↓ FF |
|
|
How do you calculate the filtered load?
|
Filtered load = GFR * Px
Px = plasma concentration of X (mg/ml) |
|
|
How do you calculate the excretion rate?
|
Excretion rate = V * Ux
V = urine flow rate (ml/min) Ux = urine concentration of X (mg/ml) |
|
|
How do you calculate the reabsorption rate?
|
Reabsorption = Filtered load - Excretion rate
Filtered load = GFR * Px Excretion rate = V * Ux |
|
|
How do you calculate the secretion rate?
|
Secretion = Excretion rate - Filtered load
Filtered load = GFR * Px Excretion rate = V * Ux |
|
|
What are the characteristics of glucose clearance in the kidney?
|
- Glucose at a normal plasma level is completely reabsorbed in the proximal tubule by Na+/glucose co-transport
- At plasma glucose of ~200 mg/dL, glucosuria begins (threshold) - At plasma glucose of ~375 mg/dL, all transporters are fully saturated (Tm) |
|
|
At what plasma glucose concentrations does all glucose get reabsorbed in the proximal tubule?
|
Up to ~200 mg/dL
- Above 200 mg/dL, glucosuria begins (threshold) |
|
|
At what plasma glucose concentrations are all Na+/glucose co-transporters fully saturated (Tm)?
|
At ~375 mg/dL
|
|
|
What happens to glucose and amino acid reabsorption during pregnancy?
|
Normal pregnancy ↓ reabsorption of glucose and amino acids in proximal tubule → glucosuria and aminoaciduria
|
|
|
How are amino acids normally treated in the kidney?
|
Normally all amino acids are reabsorbed by Na+ dependent transporters in the proximal tubule
|
|
|
What disorder causes a deficiency of neutral amino acid (eg, tryptophan) transporters in the proximal renal tubular cells and on enterocytes? Implications?
|
Hartnup Disease:
- Leads to neutral aminoaciduria and ↓ absorption from gut - Results in pellagra-like symptoms; treat with high-protein diet and nicotinic acid |
|
|
What should you think of if you have a patient with a neutral aminoaciduria and decreased absorption from the gut with pellagra-like symptoms (dermatitis, diarrhea, and mental disturbance)? Cause?
|
Hartnup Disease
- Autosomal recessive deficiency of neutral amino acid (eg, tryptophan) transporters in the proximal renal tubular cells and on enterocytes |
|
|
What are the characteristics of Hartnup Disease? Cause / Symptoms / Treatment?
|
- Autosomal recessive disorder, caused by deficiency of neutral amino acid (eg, tryptophan) transporters in the proximal renal tubular cells and on enterocytes
- Leads to neutral aminoaciduria and ↓ absorption from gut - Results in pellagra-like symptoms (dermatitis, diarrhea, and mental disturbance) - Treat with high-protein diet and nicotinic acid |
|
|
What is reabsorbed and secreted in the proximal convoluted tubule?
|
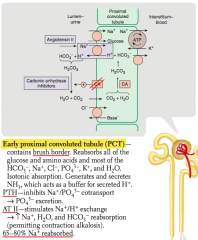
Reabsorbed:
- All glucose and amino acids - Most HCO3-, Na+, Cl-, PO4(3-), K+, H2O Secreted: - NH3 (buffers secreted H+) |
|
|
Which hormones act on the early proximal convoluted tubule?
|
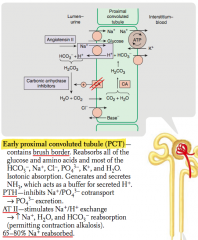
- PTH
- AngII |
|
|
What is the action of PTH on the early proximal convoluted tubule?
|

Inhibits Na+ / PO4(3-) co-transport → PO4(3-) excretion
|
|
|
What is the action of Angiotensin II on the early proximal convoluted tubule?
|
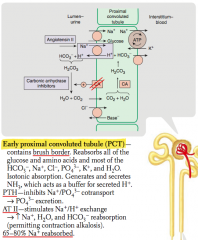
- Stimulates Na+/H+ exchange → ↑ Na+, H2O, and HCO3- reabsorption
- Permits contraction alkalosis |
|
|
What percent of Na+ is reabsorbed in the early proximal convoluted tubule?
|
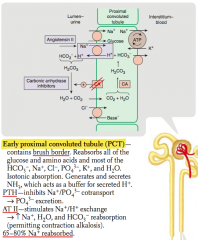
65-80% Na+ reabsorbed
|
|
|
What is reabsorbed and secreted in the thin descending loop of Henle?
|
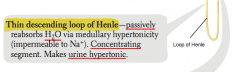
- Passive reabsorption of H2O via medullary hypertonicity
- Impermeable to Na+ |
|
|
What happens to urine in the thin descending loop of Henle?
|
- Concentrates urine
- Makes urine hypertonic |
|
|
What percent of Na+ is reabsorbed in the thin descending loop of Henle?
|
None - impermeable to Na+
|
|
|
What is reabsorbed and secreted in the thick ascending loop of Henle?
|

Reabsorbs:
- Active reabsorption of Na+, K+, and Cl- - Indirectly induces paracellular reabsorption of Mg2+ and Ca2+ (through + lumen potential generated by K+ backleak) Impermeable to H2O |
|
|
What happens to urine in the thick ascending loop of Henle?
|

- Impermeable to H2O but reabsorbing Na+
- This makes urine less concentrated as it ascends |
|
|
What percent of Na+ is reabsorbed in the thick ascending loop of Henle?
|

10-20% Na+ reabsorbed
|
|
|
What is reabsorbed and secreted in the early distal convoluted tubule?
|
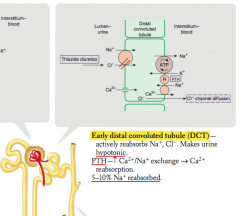
- Actively reabsorbs Na+ and Cl-
- PTH stimulates Ca2+/Na+ exchange → Ca2+ reabsorption |
|
|
Which hormones act on the distal convoluted tubule? Action?
|
PTH - stimulates Ca2+/Na+ exchange → Ca2+ reabsorption
|
|
|
What percent of Na+ is reabsorbed in the distal convoluted tubule?
|
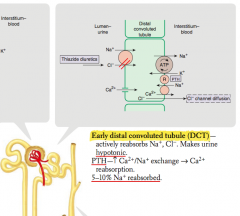
5-10% Na+ reabsorbed
|
|
|
What is reabsorbed and secreted in the collecting tubule?
|

Reabsorbs Na+ in exchange for secreting K+ and H+
|
|
|
Which hormones act on the collecting tubule? Action?
|

- Aldosterone: acts on mineralocorticoid receptor → insertion of Na+ channel on luminal side
- ADH: acts at V2 receptor → insertion of aquaporin H2O channels on luminal side |
|
|
What percent of Na+ is reabsorbed in the collecting tubule
|

3-5% Na+ reabsorbed
|
|
|
In which segments of the nephron is sodium reabsorbed? What percentages?
|
- Proximal convoluted tubule: 65-80%
- Thin descending loop of Henle: none - Thick ascending loop of Henle: 10-20% - Distal convoluted tubule: 5-10% - Collecting tubule: 3-5% |
|
|
What are the types of renal tubular defects?
|
"The kidneys put out FABulous Glittering Liquid"
- Fanconi syndrome = 1st defect (PCT) - Bartter syndrome = 2nd defect (thick ascending loop of Henle) - Gitelman syndrome = 3rd defect (DCT) - Liddle syndrome = 4th defect (collecting tubule) |
|
|
Which renal tubular defect affects the Proximal Convoluted Tubule? What does it cause?
|
Fanconi Syndrome
- ↑ excretion of nearly all AAs, glucose, HCO3-, and PO4(3-) - May cause metabolic acidosis (proximal renal tubular acidosis) |
|
|
What causes Fanconi Syndrome? Where is the defect?
|
- Causes: hereditary defects (eg, Wilson disease), ischemia, and nephrotoxins/drugs
- Reabsorptive defect in the proximal convoluted tubule |
|
|
Which renal tubular defect affects the Thick Ascending Loop of Henle? What does it cause?
|
Bartter Syndrome
- Affects Na+/K+/2Cl- co-transporter - Causes hypokalemia, metabolic alkalosis and hypercalciuria |
|
|
What causes Bartter Syndrome? Where is the defect?
|
- Causes: autosomal recessive defect of Na+/K+/2Cl- co-transporter
- Reabsorptive defect in thick ascending loop of Henle |
|
|
Which renal tubular defect affects the Distal Convoluted Tubule? What does it cause?
|
Gitelman Syndrome
- Hypokalemia - Metabolic alkalosis - NO hypercalciuria |
|
|
What causes Gitelman Syndrome? Where is the defect?
|
- Cause: autosomal recessive defect of NaCl reabsorption |
|
|
Which renal tubular defect affects the Distal and Collecting Tubules? What does it cause?
|
Liddle Syndrome
- Hypertension - Hypokalemia - Metabolic alkalosis - ↓ Aldosterone |
|
|
What causes Liddle Syndrome? Where is the defect?
|
- Cause: Autosomal Dominant defect leading to increased activity of epithelial Na+ channel
- Distal and collecting tubules |
|
|
How do you treat Liddle Syndrome?
|
Amiloride
|
|
|
What syndrome causes ↑ excretion of nearly all AAs, glucose, HCO3-, and PO4(3-), which may lead to a metabolic acidosis? What causes this?
|
Fanconi Syndrome
- Reabsorptive defect in proximal convoluted tubule - Causes: hereditary defects (eg, Wilson disease), ischemia, and nephrotoxins/drugs |
|
|
What syndrome causes hypokalemia and metabolic alkalosis with hypercalciuria? What causes this?
|
Bartter Syndrome |
|
|
What syndrome causes hypokalemia and metabolic alkalosis without hypercalciuria? What causes this?
|
Gitelman Syndrome
- Reabsorptive defect of NaCl in distal convoluted tubule - Autosomal recessive, less severe than Bartter syndrome |
|
|
What syndrome causes hypertension, hypokalemia, metabolic alkalosis, and ↓ aldosterone? What causes this?
|
Liddle Syndrome |
|
|
What is the meaning of the ratio of TF/P?
|
[Tubular Fluid] / [Plasma]
|
|
|
What does it mean if the [Tubular Fluid] / [Plasma] ratio is >1?
|
Solute is reabsorbed less quickly than water
|
|
|
What does it mean if the [Tubular Fluid] / [Plasma] ratio is =1?
|
Solute and water are reabsorbed at the same rate
|
|
|
What does it mean if the [Tubular Fluid] / [Plasma] ratio is <1?
|
Solute is reabsorbed more quickly than water
|
|
|
What happens to the tubular inulin concentration as it progresses along the nephron? How?
|
Inulin concentration increases in the tubule (but not in amount) along the proximal tubule as a result of water reabsorption |

