![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
Which drug is an osmotic diuretic? Mechanism? |
Mannitol
- ↑ Tubular fluid osmolarity - Produces ↑ urine flow - ↓ Intracranial / intraocular pressure |
|
|
What are the clinical uses of Mannitol?
|
- Drug overdose
- ↑ Intracranial / intraocular pressure |
|
|
What potential toxicity is associated with Mannitol? Contraindications?
|
- Pulmonary edema
- Dehydration - Contraindication in anuria and CHF |
|
|
Which drug is a carbonic anhydrase inhibitor? Mechanism?
|
Acetazolamide
- Causes self-limited NaHCO3- diuresis - ↓ Total body HCO3- stores |
|
|
What are the clinical uses of Acetazolamide?
|
- Glaucoma
- Urinary alkalinization - Metabolic alkalosis - Altitude sickness - Peudotumor cerebri |
|
|
What toxicity is associated with Acetazolamide?
|
- Hyperchloremic metabolic acidosis ("ACID"azolamide causes "ACID"osis)
- Paresthesias - NH3 toxicity - Sulfa allergy |
|
|
What are the types of loop diuretics?
|
- Furosemide
- Ethacrynic Acid |
|
|
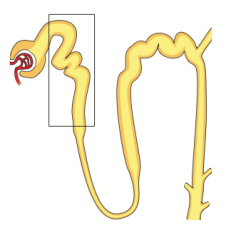
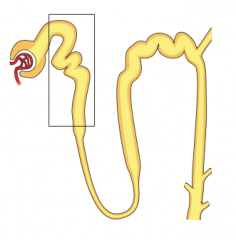
What is the mechanism of Furosemide?
|
Sulfonamide loop diuretic:
- Inhibits co-transport system (Na+/K+/2Cl-) of thick ascending limb of loop of Henle - Abolishes hypertonicity of medulla, preventing concentration of urine - Stimulates PGE release (vasodilatory effect on afferent arteriole); inhibited by NSAIDs - ↑ Ca2+ excretion (Loops Lose Calcium) |
|
|
What are the clinical uses of Furosemide?
|
- Edematous states (CHF, cirrhosis, nephrotic syndrome, pulmonary edema)
- Hypertension - Hypercalcemia (Loops Lose Calcium) |
|
|
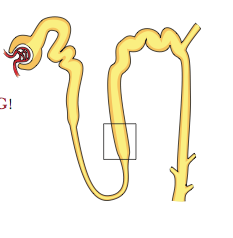
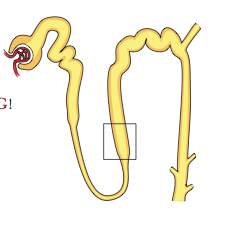
What are the potential toxic side effects of Furosemide?
|
OH DANG!
- Ototoxicity - Hypokalemia - Dehydration - Allergy (sufla) - Nephritis (interstitial) - Gout |
|
|
What is the mechanism of Ethacrynic Acid?
|
Loop Diuretic:
- Phenoxyacetic acid derivative (not a sulfonamide) - Inhibits co-transport system (Na+/K+/2Cl-) of thick ascending limb of loop of Henle - Abolishes hypertonicity of medulla, preventing concentration of urine - Stimulates PGE release (vasodilatory effect on afferent arteriole); inhibited by NSAIDs - ↑ Ca2+ excretion (Loops Lose Calcium) |
|
|
What is the clinical use of Ethacrynic Acid?
|
Diuresis in patients allergic to sulfa drugs (Furosemide):
- Edematous states (CHF, cirrhosis, nephrotic syndrome, pulmonary edema) - Hypertension - Hypercalcemia (Loops Lose Calcium) |
|
|
What are the side effects of Ethacrynic Acid?
|
- Similar to furosemide (OH DANG: Ototoxicity, Hypokalemia, Dehydration, Nephritis (interstitial), Gout)
- Can cause hyperuricemia - never used in patients with gout |
|
|
What is the mechanism of Hydrochlorothiazide?
|
Thiazide Diuretic:
- Inhibits NaCl reabsorption in early distal tubule - ↓ Diluting capacity of the nephron - ↓ Ca2+ excretion |
|
|
What are the clinical uses of Hydrochlorothiazide?
|
- Hypertension
- CHF - Idiopathic hypercalciuria (↓ Ca2+ excretion) - Nephrogenic diabetes insipidus - Osteoporosis (↓ Ca2+ excretion) |
|
|
What are the potential side effects of Hydrochlorothiazide?
|
- Hypokalemic metabolic alkalosis
- Hyponatremia - Sulfa allergy Hyper-GLUC: - HyperGlycemia - HyperLipidemia - HyperUricemia - HyperCalcemia |
|
|
What are the K+ sparing diuretics?
|
- Spironolactone and Eplerenone
- Triamterene - Amiloride |
|
|
What is the mechanism of the Spironolactone and Eplerenone?
|
K+ Sparing Diuretics:
- Competitive aldosterone antagonists in the cortical collecting tubule |
|
|
What is the mechanism of Triamterene and Amiloride
|
K+ Sparing Diuretics:
- Act on cortical collecting tubule by blocking Na+ channels |
|
|
What are the clinical uses of the K+ sparing diuretics?
|
- Hyperaldosteronism (Spironolactone and Eplerenone are aldosterone receptor antagonists)
- K+ depletion - CHF |
|
|
What are the potential toxicities of K+ Sparing Diuretics?
|
- Hyperkalemia: can lead to arrhythmia
- Endocrine effects with Spironolactone: eg, gynecomastia, anti-androgen effects |
|
|
How do diuretics affect urine NaCl? Exceptions?
|
↑ urine NaCl, serum NaCl may ↓ as a result
- Exception: Acetazolamide |
|
|
How do diuretics affect urine K+? Exceptions?
|
↑ with loop and thiazide diuretics
Serum K+ may ↓ as a result - Exception: K+ sparing diuretics |
|
|
Which diuretics cause acidemia? Mechanism?
|
- Carbonic Anhydrase Inhibitors (Acetazolamide) by ↓ HCO3- reabsorption
- K+ sparing / Aldosterone Antagonists by preventing K+ secretion and H+ secretion; hyperkalemia leads to K+ entering all cells (via H+/K+ exchanger) in exchange for H+ exiting cells) |
|
|
Which diuretics cause alkalemia? Mechanism?
|
Loop diuretics and thiazide diuretics:
- Volume contraction → ↑ AT II → ↑ Na+/H+ exchange in proximal tubule → ↑ HCO3- reabsorption ("contraction alkalosis") - K+ loss leads to K+ exiting cells (via H+/K+ exchanger) in exchange for H+ entering cells - In low K+ state, H+ (rather than K+) is exchanged for Na+ in cortical collecting tubule → alkalosis and "paradoxical aciduria" |
|
|
How do diuretics affect urine Ca2+? Mechanism?
|
- ↑ urine Ca2+ with loop diuretics: ↓ paracellular Ca2+ reabsorption → hypocalcemia
- ↓ urine Ca2+ with thiazide diuretics: enhanced paracellular Ca2+ reabsorption in distal tubule |
|
|
What are the types of ACE inhibitors?
|
- Captopril
- Enalapril - Lisinopril |
|
|
What is the mechanism of ACE inhibitors?
|
- Inhibit ACE → ↓ AT II → ↓ GFR by preventing constriction of efferent arterioles
- Levels of renin ↑ as a result of loss of feedback inhibition - Inhibition of ACE also prevents inactivation of bradykinin, a potent vasodilator |
|
|
What is the mechanism of Angiotensin II Receptor Blockers?
|
Similar effect as ACE-Inhibitors but they don't ↑ bradykinin → ↓ risk of cough and angioedema
|
|
|
What are the clinical uses of ACE-inhibitors?
|
- Hypertension
- CHF - Proteinuria - Diabetic nephropathy - Prevent unfavorable heart remodeling as a result of chronic hypertension |
|
|
What toxic events can occur because of ACE-inhibitors?
|
CATCHH:
- Cough - Angioedema (contraindicated in C1 esterase inhibitor deficiency) - Teratogen (fetal renal malformations) - ↑ Creatinine (↓ GFR) - Hyperkalemia - Hypotension |
|
|
When should you avoid use of ACE-Inhibitors? Why?
|
- Women of reproductive age (because it is a teratogen)
- Bilateral renal artery stenosis (because will further ↓ GFR → renal failure) |

