![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
What kind of cancer arises on Mucosal Surfaces?
|
SCCA
|
|
|
What kind of cancer arises on skin? (3)
|
BCCA
SCCA Melanoma |
|
|
Name three different kinds of thyroid cancer
|
Papillary
Follicular Medullary |
|
|
What kind of cancer arises on soft tissue?
|
Sarcoma (by definition)
|
|
|
1) 95% of Mucosal H&N Cancers are:
2) Other 5%? |
1) SCCA
2) salivary gland or lymphoma |
|
|
Two Major risk factors for mucosal cancer of H&N (and therefore for SCCA)?
|
Alcohol
Tobacco |
|
|
EBV is predisposing factor for what kind of cancer?
|
Nasopharynx SCCA
|
|
|
In addition to Alcohol and Tobacco, HPV is a risk factor for SCCA at what specific site?
|
Oropharynx
|
|
|
Predominant pattern of spread of Mucoas H&N cancers
|
Neck Lymph nodes prior to distant site.
|
|
|
____% of Mucosal H&N cancer patients present with advanced stage disease.
|
70%
|
|
|
Name the Five general areas where Mucosal cancers can appear
|
Oral
Pharynx Larynx Esophagus Nasal Cavity/Sinuses |
|
|
1) Name the three divisions of the pharynx
2) Two of them can be affected by viruses predisposing them to SCCA. Match the virsues. |
Oropharynx - HPV
Nasopharynx - EBV Hypopharynx |
|
|
Name seven distinct sites of cancer in the mouth.
|
Lip
Anterio 2/3 of tongue Floor of of mouth Alveolar ridge Retromolar trigone Buccal mucosa hard palate. |
|
|
What are the worst and second worst places to get cancer in the mouth?
|
worst- Buccal Mucosa
second worst- Anterior 2/3 of tongue |
|
|
Nasopharynx subsites (2)
|
1) fossa of Rosenmuller
(behind eust. tube ostium) 2) posterior pharyngeal wall |
|
|
where are the frontal, maxillary, ethmoid, and sphenoid sinueses
|
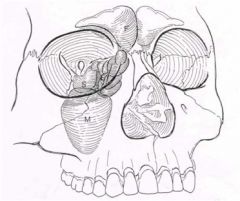
|
|
|
Mucosal tumor staging (TNM)
|
Stage I: T1 N0 M0
Stage II: T2 N0 M0 Stage III: T3 N0 M0, T1-3 N1 M0 Stage IV: T4 Nx M0, Tx N2-3 M0, Tx Nx M1 |
|
|
Any tumor which is M1:
1) stage? 2) treatment? |
1) 4
2) palliative rather than curative |
|
|
1) The most important prognostic indicator for mucosal cancers is:
2) How does this affect prognosis? |
1) cervical lymph node involvement
2) 50% decrease in survivial |
|
|
A tumor with ANY node metastasis is stage:
|
3 or 4
|
|
|
Any tumor with distant metastasis is stage:
|
4
|
|
|
General strategy for evaluation of a patient with mucosal H&N cancer.
(4 parts) |
History
physical imaging biopsy |
|
|
Who gets involved in a H&N tumor case?
|
Multidisciplinary tumor board
H&N surgeon rad-onc med-onc pathologist radiologist speech patholgist prosthodontist occasionally neurosurgeon or Thoracic Surgeon |
|
|
Rule of 80 for neck masses
|
If over 40 and have a neck mass for more than 2 weeks. 80% are neoplastic, and 80% of those are malignant.
|
|
|
Most important symptoms of H&N cancer
|
Hoarseness
Unilateral Otalgia Unilateral Middle ear fluid Neck Mass Chronic Sore throat |
|
|
Less emphasized symptoms of H&N Cancer
|
Dysphagia
Odynophagia (painful swallowing) weight loss trimus (lockjaw) nasal obstruction epistaxis cranial neuropathies aspiration airway obstruction Hemoptysis (coughing blood) |
|
|
Pertinent elements of history
|
Past cancer
meds soc fam |
|
|
Familal inheritance patterns aof H&N cancer are common/rare
|
rare
|
|
|
Physical exam IN ADDITION to a FULL PHYSICAL
|
All mucosa
skin and scalp cranial nerves ears neck/thyroid/salivary glands Bimanual (2 fingers) palpation of oral cavity, oropharynx |
|
|
Evaluation of neck "nodes"
|
size, location, numbers
fixation? pulsatile? |
|
|
1) How do we biospy neck nodes?
2) when would we not do this? |
1) fine needle aspiration
2) pulsatile |
|
|
Describe the 5 neck "levels"
|
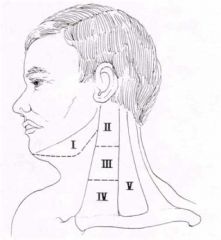
|
|
|
1) Do we do open biopsies of nodes?
2) why? |
1) NOT UNLESS UNAVOIDABLE
2) can spill cancerous cell out of node |
|
|
What two kinds of anatomical cross sectional imaging do we use?
|
CT, MRI
|
|
|
What form of functional imaging do we use?
|
PET
|
|
|
What kind of noninvasive imaging do we do?
|
US
|
|
|
What three characteristics make a cancer very high risk for metastasis?
|
1) multiple nodes
2) LOWER neck nodes 3) extracapsular spread from nodes |
|
|
1) What is our main mode of evaluation for distant metastases
2) why? |
imaging
2) CXR, and Labs (alk phos, Ca++, LFTs) are insensitive |
|
|
1) Three major distant sites of mucosal H&N cancer spread
2) single most common one? |
1) lung
bone liver 2) lung |
|
|
In what % of cases will panendoscopy show a second tumor?
|
5-15%
|
|
|
Why do we use panendoscopy?
|
biopsy and mapping of primary tumor
(diagnosis, staging, treatment planning) |
|
|
When do we use a curative approach to treatment? (by stage)
|
1-3 and some 4
|
|
|
3 reasons we would pursue a palliative approach to mucosal H&N cancer?
|
1) distant mets
2) far advanced local or regional disease 3) co-morbidities limit treatment options |
|
|
Treatment for:
Nasopharyngeal stage I and II |
Radiation alone
|
|
|
Treatment for:
Nasopharyngeal Stage 3 and 4 |
Chemo/radiation
|
|
|
What role does surgery play in the treatment of nasopharyngeal cancers?
|
Little role at primary site, may be used to excise residual nodes after primary has been cured by chemo/rads
|
|
|
Treatment of:
Non-nasopharynx cancers stage 1 and 2 |
Single modality treatment
Surgery OR Radiation |
|
|
Treatment of:
Non-nasopharynx cancers stage 3 and 4 that we are trying to CURE |
Multi-modality
a) surgery/postop rads +/- chemo b) chemo/rads wth surgery for salvage or lymph node removal |
|
|
Treatment of:
Non-nasopharynx cancers stage 3 and 4 when we are doing palliative approach |
Chemotherapy alone
|
|
|
Nasal and paranasal sinus cancer early signs
|
non-specific
|
|
|
MANY typse of cancer can arise in the nose/paranasal area
|
SCCA, minor salivary gland cancers, lymphoma, melanoma, rhabdomyosarcoma, SNUC, olfactory neuroblastoma, Ewing’s sarcoma/PNET
|
|
|
Therapy for nose/paranasal area?
|
Multimodality and dependant upon the pathology
|
|
|
Treatment consideration in nose/paranasal area cancer
|
proximity to palate, orbit, skull base, dura, brain
|
|
|
evaluation of nose/paranasal area cancer almost includes what imaging?
|
CT AND MRI
|
|
|
significant prognostic indicators for SCCA and its likelihood to metastasize
|
N0 vs. N1
size of largest node number of positive nodes location of positive nodes extracapsular spread soft tissue deposits |
|
|
Incidence and pattern of mets of HNSCCA is predictable based upon (2 simple ones)
|
disease site
T-stage |
|
|
Name three kinds of tissue transfers used to restore form and function?
|
local flaps
regional flaps (pec. major, latissimus) Distant (free) flaps- radial forearm, fibula |
|
|
Example given for facial reconstructions
|
Andy Gump Deformity
|
|
|
Post-treatment recommendations for H&N cancer.
|
1) STOP tobacco and alcohol (associated with 30-50% recurrence)
2) optimize nutritional, medical psychosocial status |
|
|
8 post-treatment considerations
|
Speech/swallowing therapy
Xerostomia Taste Alterations Physical therapy Prosthodontics Social support Thyroid function Tumor surveillance |
|
|
Tumor surveillance:
_______% of recurrences occur within ______ years. |
80% within 3 years
|
|
|
1)Considerd cured if free of recurrence after _______
2) then the focus turns to |
1) 5 years
2) watching for secondary tumors |
|
|
Prognosis:
Survival for stage I and II is: |
75%
|
|
|
Prognosis:
Survival for stage 3-4 is: |
40%
|
|
|
Except for _____ cancer, we have not imporved survival in the past 50 years
|
nasopharyngeal
|
|
|
most nasopharyngeal cancer start in the____
|
Fossa of Rosenmuller
|
|
|
People wo have never smoked have a better prognosis in what specific cancer?
|
stage 3 or 4 HPV+ oropharynx cancer
|

