![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
79 Cards in this Set
- Front
- Back
|
What are the 3 types of hormones?
|
-Peptide Hormones
-Steroids -Amino Acid Derived |
|
|
Peptide Hormone Characteristics
|
-Hydrophillic
-Made in the RER (preprohormone) and cut in ER lumen (prohormone) and packaged into vesicles by Golgi -Bind to membrane recptors and activate 2nd messengers -RAPID BUT SHORT-LIVED |
|
|
Steroid Hormone Characteristics
|
-Hydrophobic
-Made from cholesterol in Smooth ER and immediately secreted from cell -Travel bound to protein plasma and diffuse diffuse through cell membranes -Activate cytosolic proteins or alter txn of [protein] in nucleus -SLOW BUT LONG-LIVED |
|
|
Amino Acid Derived Hormones
(Tyrosine-derived) |
Mimic either peptide or steroid hormonal characteristics
-Peptide: Catecholamines (adrenaline, norepinephrine) -Steroid: Thyroid Hormones; T3, T4 |
|
|
Is the Pancreas an endocrine or exocrine gland?
|
Both!
-Exocrine: secretes digestive enzymes and biocarbante through ducts into gastrointestinal tract -Endocrine: secretes hormones into bodily fluid (insulin glucagon, and somatostatin) |
|
|
What cells in the pancreas secrete endocrine hormones?
|
Islet cells; "The islets of Langerhans"
-Alpha: secrete insulin -Beta: secrete glucagon -Delta: secrete somatostatin |
|
|
Insulin (4 main functions)
|
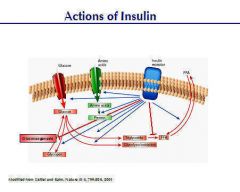
1. Increase cellular uptake of glucose
2. Decrease blood glucose levels 3. Promote glycogen production in liver 4. Increase protein & triglyceride synthesis |
|
|
Glucagon
|
Opposite effects of Insulin.
1. Increases blood glucose levels by: a) Promoting glycogenolysis and gluconeogensis in liver 2. Also promotes lipid breakdown **Does Not Decrease Cellular uptake of Glucose** |
|
|
Somatostatin
|
Regulates endocrine system by inhibiting digestive processes--takes longer for nutrients to be absorbed
-Inhibits both insulin and glucagon |
|
|
What is hyperglycemia?
|
Excessively high blood glucose levels caused by:
-diminished insulin secretion or activity |
|
|
What is hypoglycemia?
|
Excessively low blood glucose levels caused by:
-elevated insulin levels -insufficient glucagon in body |
|
|
Two adrenal glands are:
|
1. Cortex
2. Medulla |
|
|
Adrenal Cortex
|
-Produces steroid hormones:
a) mineralcorticoids i.e. aldosterone (most outer) b) glucocorticoids i.e. cortisol (inner) c) sex hormones (most inner) |
|
|
Aldosterone
|
What? Steroid mineralcorticoid increasing:
1) urinary excretion of K+ 2) Interstitial Na+ concentration 3) 2° effect: water conservation, ↓urine output How and where? -Increase Na+/K+ pump activity in the distal convoluted tubule of the kidney |
|
|
Cortisol
|
Glucocorticoid stress hormone regulated by ACTH of the anterior pituitary gland which is further regulated by the hypothalmus.
-↑ blood sugar through gluconeogenesis, cardiac contractions, water retention & anti-inflammatory -↓ immune activity |
|
|
Adrenal Medulla
|
Secretes the catecholamine peptide hormones: epinephrine & norepinephrine.
-Increases heart rate, blood pressure, increase alertness |
|
|
Thyroid
|
Secretes both tyrosine-derived (T3/T4) and peptide hormones (calcitonin).
|
|
|
Other names for T3 and T4
|
Triiodothyronine and Thyroxine
|
|
|
T3 and T4 function
|
-Generalized increase in metabolism
-Stimulate O2 demand, heat production, and growth/development Regulated by anterior pituitary (TSH) and hypothalamus --Negative Feedback Inhibition on TSH and TRH |
|
|
Hypothyroidism
|
Inaqdequate production of thyroid hormones causing:
-Decrease in metabolism→overweight, -Goiter: increase in growth for iodine absorption |
|
|
Calcitonin
|
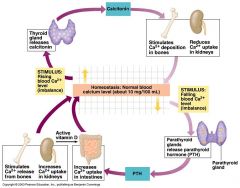
Pep. hormone produced in parafollicular cells of thyroid
-Reduces blood Ca++ levels by: -Increasing Ca++ deposition in bones -Decreasing kidney Ca++ resorption |
|
|
Parathyroid Hormone (PTH)
|
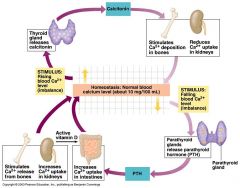
-Opposite effects of calcitonin.
-Responds to low Ca++ blood levels and increases blood Ca++ concentration by: 1) ↑ bone release of Ca++ 2) ↑ Intestinal and Kidney Ca++ uptake |
|
|
Ovaries
|
Site of oogenesis in women and responsible for progesterone and estrogen synthesis
|
|
|
Menstrual Cycle
|
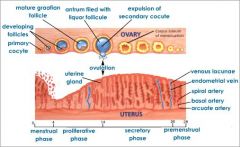
Series of hormonally induced events preparing female for pregnancy. Described by changes with respect to ovaries (ovarian cycle) or endometrial lining (uterine cycle). Bleeding marks first 1st day (flow).
|
|
|
Phases of Ovarian Cycle
|
1) Follicular- Anterior pituitary releases FSH & LH that stimulates rapid growth of follicle. Follicle secretes estrogen that stimulates LH (+ feedback) & causes luteal surge (day 14)
2) Ovulation: Mid-cycle release of the egg 2) Luteal Phase-After ovulation, corpus luteum remains secreting progesterone & estrogen day 14-28 3) Flow-shedding of uterine lining; corresponds w/ beginning of follicular phase |
|
|
Phases of the Uterine Cycle
|
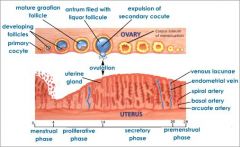
(1) Menses- shedding of uterine lining; same time as early follicular phase
(2) Proliferative Phase- Until day 14. Estrogen secretion from follicle induces proliferation of endometrium (3) Secretory Phase- Progesterone (& estrogen) from corpus luteum promotes rapid thickening & vascularization of endometrium--final 14 days |
|
|
What happens if mature ovum is not fertilized?
|
~13 days after ovulation (day 27)
-corpus luteum degenerates into corpus albicans -progesterone/estrogen not available so endometrium severs (~5 days)---> new proliferative phase |
|
|
What happens if mature ovum is fertilized?
|
~day 14, developing placenta secretes hCG upon implantation that keeps corpus luteum from degenerating until end of 1st trimester when placenta takes over
|
|
|
Where is the mature ovum usually fertilized by sperm?
|
Oviduct (fallopian tube)
-more specifically, the AMPULLA of the uterine tube |
|
|
Luteal Surge
|
Sudden ↑ of LH associated with release of ovum (haploid cell produced by 1st meiotic division of 1° oocyte)
|
|
|
Corpus Luteum
|
Remnant of ruptured follicle. Secretes progesterone and estrogen that promotes endometrium growth.
|
|
|
hCG
|
Human chorionic gonadotropin.
-secreted from placenta upon implantation of fertilized ovum that keeps corpus luteum from degenerating until end of 1st trimester when placenta takes over progesterone/estrogen secretion |
|
|
Primary Follicle
|
-FSH stimulates growth of granulosa cells around 1° ooctye.
-g cells secrete viscous zona pellucida around egg |
|
|
Secondary Follicle
|

LH--->follicle to complete first meiotic division in which theca cells arise from interstitial tissue around 1° follicle to form 2° follicle.
|
|
|
Theca cells
|
Stimulated by LH and release androgen that is converted to estradiol by granulosa cells (+FSH) that is secreted into blood
|
|
|
Gonadotropin releasing hormone (GnRH)
|
Secreted from hypothalamus. Responsible for secretion of FSH & LH from anterior pituitary gland.
|
|
|
Where does spermatogenesis (gametogenesis) take place?
|
Seminiferous tublules of the testes
|
|
|
Gonads
|
Ovaries or Testes
|
|
|
Name of male germ cells as it grows?
|
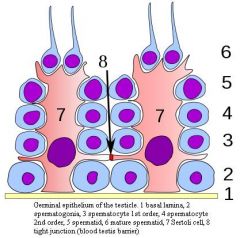
(1) Spermatogonia or spermatogonium
(2) 1° Spermatocyte (3) Spermatids (4) Spermatozoa or spermatozoon |
|
|
Leydig cells
|
-Interstitum tissue of seminiferous tubules
-secretes testosterone when stimulated by LH |
|
|
ICSH
|
interstitial cell stimulating hormone
-another name for LH in males -becomes plentiful upon puberty |
|
|
Testosterone
|
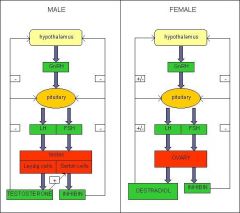
Primary male androgen
-Promote spermatogenesis -Promotes secondary sex characteristics (i.e. deep voice, facial/pubic hair, penis enlargement) |
|
|
Spermatogenesis
|
Division of spermatogonia within the seminferous tubules to produce haploid spermatozoa
|
|
|
Sertoli Cells
|
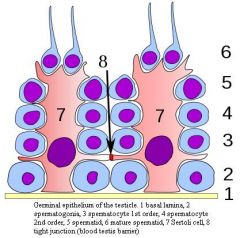
-Nurture and surround spermatocytes and spermatid
-Stimulated by FSH -Secrete inhibin which blocks FSH (@ant. pit./hypothal) |
|
|
Inhibin
|
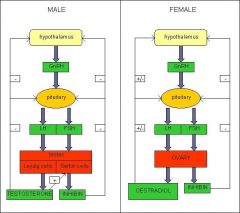
-Peptide hormone that secreted from sertoli cells -inhibits release of FSH from anterior pituitary gland
|
|
|
When do male germ cells form the "head, midpiece, and tail" configuration?
|
From spermatid (regular cell characteristics) to a spermatozoon.
|
|
|
Acrosome
|
Contains lysosome-like enzymes for penetration of egg during fertilization
|
|
|
Anatomy of Spermatozoon
|
Head-contains nucleus and acrosome
Midpiece- contains mitochondria to provide movement of tail Tail- standard 9+2 microtubule arrangement |
|
|
Epididymis
|
Coiled tube attached to each testis
-site where spermatozoon mature |
|
|
Where is semen produced?
|
1. Seminal valves-fructose and prostaglandins
2. Prostate- milky alkaline fluid 3. Cowper's glands (bulbourethral glands) |
|
|
Path of Ejaculation
|
Spermatozoon--->vas deferens---->urethra--->out of penis
|
|
|
At what stage do 1° oocytes become arrested?
|
Prophase I of meiosis
|
|
|
What two cells are formed at the end of meiosis I?
|

Secondary oocyte and polar body (both haploid)
|
|
|
Polar body
|
Formed after meiosis I from oocyte
-contains less cytoplasm (nutrients) -may continue with meiosis II but ultimately disintegrates |
|
|
What stimulates the release of GnRH?
|
Low levels of estrogen/progesterone in the blood monitored by the hypothalamus?
|
|
|
What causes termination of reproductive cycle in females?
|
Negative feedback from high levels of estrogen/progesterone inhibits FSH/LH secretion through inhibiting GnRH at hypothalamus
|
|
|
Endocrine functions of Hypothalamus
|
-Releases hormones that control secretions from the pituitary gland
-Regulating control center for endocrine and ANS |
|
|
Tropic Hormone
|
Hormones that target other endocrine glands
|
|
|
Name the 6 (or 7) peptide hormones from the anterior pituitary gland
|
"FLAT PEG"
1. FSH 2. LH 3. ACTH (adrenocorticotropic hormone) 4. TSH 5. PTH 6. Endorphins 7. Growth Hormone (hGH) |
|
|
All hormones secreted from the anterior pituitary are tropic and peptide hormones (T/F)
|
False.
All are peptide hormones, however, GH and Prolactin are non-tropic hormones |
|
|
TSH or thyrotropic hormone
|
Thyroid Stimulating Hormone
-stimulates thyroid to release of T3, T4 via cAMP -responsible for increase in thyroid size/number, and secretion rate of T3, T4 |
|
|
ACTH
|
Adrenocorticotropin Hormone
-stimulates adrenal cortex to release glucocorticoids, mainly CORTISOL, via cAMP |
|
|
LH
|
Luteinizing Hormone
-Stimulates gonads (ovaries or testes) to promote sex hormone secretion (estrogen/progesterone, testosterone) -stimulates gamete production (Leydig cells) |
|
|
FSH
|
Follicle stimulating hormone
-stimulates follicle maturation -stimulates sperm production (sertoli cells) |
|
|
Non-tropic hormones
|
Hormones that directly stimulate target cells to induce effects (Prolactin, GH, Oxytocin)
|
|
|
GH
|
Growth Hormone
-Influences growth in most cells of the body -Development of skeletal muscle, bones, and organs -W/O GH----> abnormal development |
|
|
STH
|
Somatotropin Hormone aka Growth Hormone
|
|
|
Prolactin
|
-Directly targets female breasts
-Stimulates breast development and milk production |
|
|
ADH and Oxytocin are produced at the posterior pituitary gland (T/F)
|
False.
Produced in the neural soma of the hypothalamus and transported via vesicles down axons---> stored and released from posterior pituitary |
|
|
What are the two peptide hormones released from the posterior pituitary gland?
|
1. ADH
2. Oxytocin |
|
|
ADH
|
Antidiuretic hormone or Vasopressin
-stimulates water absorption at the collecting ducts of kidneys -2° effects: ↑blood pressure, salty urine |
|
|
What inhibits ADH?
|
Caffeine, beer
|
|
|
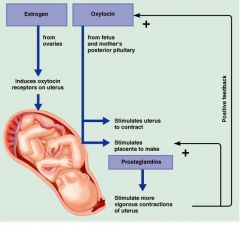
Oxytocin
|
-Smooth muscle contractions of breast lactating
Released at childbirth (parturition): -Causes uterus to contract and push the fetus through birth canal -Stimulates placenta to secrete prostaglandins--> more vigorous contractions of uterus |
|
|
Adrenal Cortex is responsible for the production of mineral/glucocorticoids...as well as sex hormones (T/F)
|
True.
-Secretes low levels of sex steroids (mostly androgens) |
|
|
CRH
|
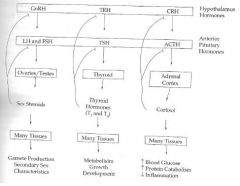
Cortico Releasing Hormone
-secreted from hypothalamus and stimulates release of ATCH from posterior pituitary |
|
|
TRH
|
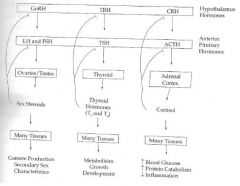
Thyrotropin-releasing hormone
-produced in hypothalamus -stimulates release of TSH from pituitary gland |
|
|
Two major divisions of feedback regulation
|
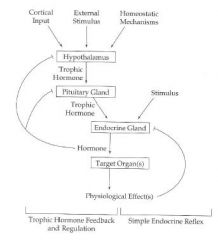
(1) Simple Endocrine Reflex: physiological endpoint shutting off signal at endocrine gland
(2) Tropic Hormone feedback regulation: regulating release from higher organs (hypothalamus, pituitary) |
|
|
Progesterone
|
Builds vascularization of endometrium for blastocyst implantation. Secreted by follicle, corpus luteum, and placenta. (also stored in the adrenal cortex,mostly males)
|
|
|
What hormonal signal causes menstruation to begin?
|
High levels of estrogen and progesterone
Estrogen+Progesterone---|GnRH--->FSH+LH--->Corpus L. |

