![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
What are the two types of "antiestrogen" drug classes?
|
Aromatase inhibitors and estrogen receptor antagonists.
|
|
|
TAMOXIFEN:
|
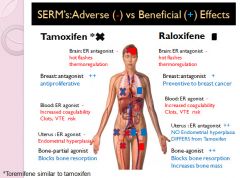
- A SERM "selective estrogen receptor modulator"
- A first line drug for ER+ breast cancers. - Metabolized by CYP450 in the liver to more active forms that act at ERa and ERb receptors. (Therefore, CYP inhibitors can decrease the bioavailability of the drug) - Complex mechanism “mixed agonist/antagonist” Antagonist of ER in breast & hypothalamus Agonist in blood & endometrial tissues. (Increases blood coagulation and is proliferative to endometrium) Partial agonist in bone: Decreases bone resorption but not likely to increase bone mass (does not increase bone loss) |
|
|
Mechanism of Action of Tamoxifen:
|
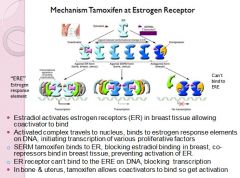
|
|
|
TOREMIFENE:
|
- A SERM
- alternative in ER+ breast cancer resistant to tamoxifen - Similar agonist/antagonist profile to tamoxifen - Toremifene more bioactive than its cyp450 metabolites - Good alternative drug to tamoxifen for someone who is on a strong CYP inhibitor!! |
|
|
RALOXIFENE:
|
- A SERM
- Approved for breast cancer prevention/ reoccurrence - MAJOR Difference: raloxifene is an antagonist in uterus; Don’t get endometrial hyperplasia so long-term use- doesn’t increase risk endometrial cancer - More potent agonist in bone than tamoxifen *Primary clinical use is for treatment of osteoporosis in post-menopausal women |
|
|
What are two adverse effects of the SERM's?
|
Hot flashes and increased risk of blood clots and venous thromboembolism.
|
|
|
Chart of SERM side effects and/or benefits:
|
|
|
|
Aromatase inhibitors come in what two types?
|
Steroidal type I: irreversible
Non-steroidal type II: reversible |
|
|
Why would you use an aromatase inhibitor in a post-menopausal woman with ER+ breast cancer?
|
Because post -menopausal women get their estrogen from aromatase
|
|
|
In a ER+ breast cancer patient who has a family history of hypercoagulability, which drug should you give preference to; SERM's or Aromatase inhibitors?
|
An aromatase inhibitor; because they do not increase the risk of clotting while the SERM's do!
|
|
|
ANASTRAZOLE
|
- Aromatase Inhibitor
- Non- steroidal Type II - Mechanism: Competitive inhibitor aromatase; Blocks conversion of androstenedione into estrone and blocks major path of estrogen synthesis in post-menopausal women - Estrogen levels are depleted throughout the body - Adverse effects: Lose estrogen protective effects on blood lipids Hot flashes/flushes, CNS effects (depression) Major effects on bone health (Bone pain, increased fracture risk Loss of bone mass/ osteoporosis) - Beneficial effects: Shuts of endogenous estradiol synthesis to decrease growth of ER+ breast tumors *Effective alternative in many cases of tamoxifen-resistant ER+ breast cancer in post-menopausal women *Long-term use decreases risk of endometrial cancer *Doesn’t increase the risk of VTE, doesn’t increase blood coagulability |
|
|
EXEMESTANE:
|
- An Aromatase Inhibitor
- Steroidal type I class - Mechanism: Irreversible “suicide” inhibitor aromatase - Alternative –depletes aromatase - Androgenic effects reported - Other side effects similar to non-steroidal type II AI’s |
|
|
Which hormonal breast cancer drug is associated with an increased risk of endometrial cancer?
|
Tamoxifen
|
|
|
FULVESTRANT:
|
- Competitive antagonist at ERα & ERβ receptors
- Effects not tissue specific –blocks all estrogen receptors- adverse effects of estrogen depletion - Down-regulates ER in tumor - Indication: Alternative postmenopausal woman if SERM’s or aromatase inhibitor failure |
|
|
Progesterone is released in the ______ phase of the menstrual cycle after _____?
|
Luteal, ovulation
|
|
|
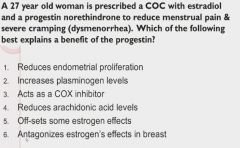
How does progesterone increase the risk of clots?
|
By decreasing plasminogen activation
|
|
|
Reduces endometrial proliferation
|
|
|
Pharmacology of Estrogen:
|
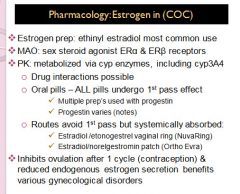
|
|
|
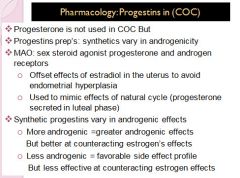
Pharmacology of Progestin:
|
|
|
|
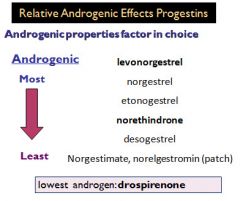
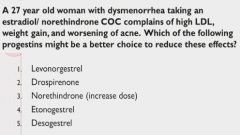
Androgenic effects of different progesterones:
|
|
|
|
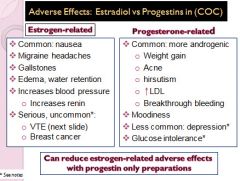
Adverse effects of Estrogen vs. Progesterone:
|
|
|
|
Drospirenone and Desogestral
|
|
|
Progesterin only preparations:
|
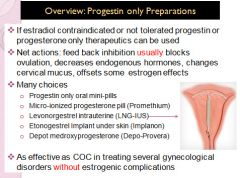
|
|
|
Danazol:
|
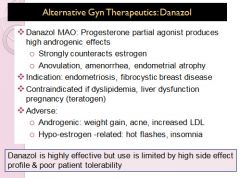
|
|
|
GnRH agonists:
|
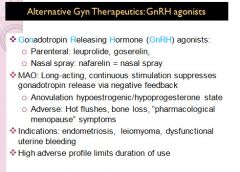
|
|
|
Therapuetics for endometriosis:
|
- COC or progestin only therapeutics common 1st line pharmacologic treatments:
COC & progestins decrease estrogen - Reduce endometrial proliferation in uterine & non-uterine areas - Minimize pain/ both types effective - Can be used long-term in patients not desiring pregnancy - Cost effective/ low adverse effects - Alternative pharmacologics: Danazol, GnRH agonists Aromatase inhibitors |
|
|
GnRH agonist vs Danazol for treatment of endometriosis:
|
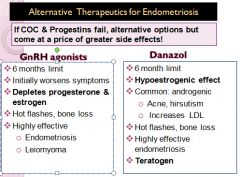
|
|
|
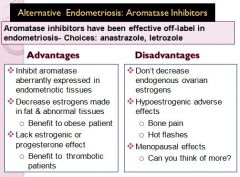
Aromatase Inhibitor treatment for endometriosis:
|
|
|
|
Treatment of uterine fibroids:
|
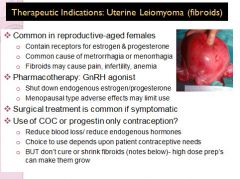
|
|
|
Treatment of Mestrual disorders:
|
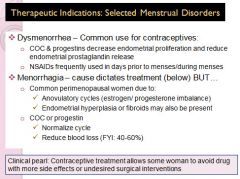
|
|
|
Treatment of Menorrhaghia when estrogen is contraindicated:
|
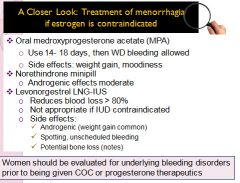
|
|
|
Treatment of severe uterine Bleeding:
|
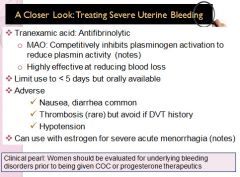
|
|
|
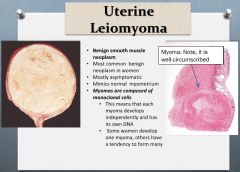
Leiomyomas are also called?
|
Fibroids, fibromas and myomas
|
|
|
Characteristics of uterine leiomyomas:
|
|
|
|
Pathogenesis of Leiomyomas:
|
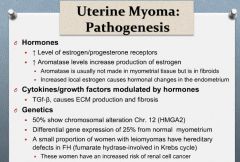
|
|
|
Presenting symptoms of leiomyomas:
|
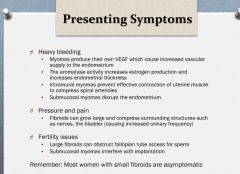
|
|
|
Medical treatment of leiomyomas:
|
Initial therapy is usually directed at symptom control.
Oral contraceptives, progesterone, and progesterone containing IUDs are used to control menorrhagia from myomas, but they do not cause fibroids to shrink or regress |
|
|
GnRH treatment of fibroids:
|
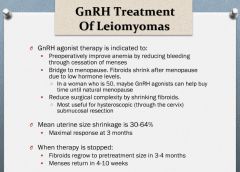
|
|
|
What are some surgical treatment options for uterine fibroids?
|
1. Uterine artery embolization
2. Hysterectomy 3. Myomectomy |
|
|
Uterine Leiomyosarcoma:
|
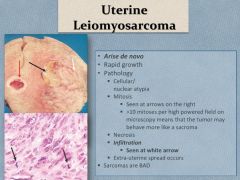
|
|
|
Malignant Mixed Mullerian Tumor:
|
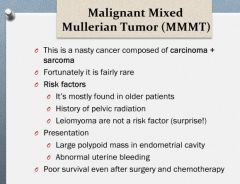
|
|
|
Histology of an MMMT:
|
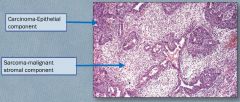
|

