![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
What body cavities must be developed?
|
There are two major cavities: the Thoracic and Abdominopelvic Cavities. Subdivided: Thoracic has the pleural and pericardial cavity and Abdominopelvic cavity has the peritoneal and retroperotoneal cavities.
|
|

Name 1 and 2 and what tissue layer they associate with. And name the space in 3.
|

1. Somatic Mesoderm (ectoderm)
2. Splanchnic mesoderm (endoderm) 3. Intraembryonic coelom NOTE: that these are the earliest cavities derived from the lateral plate mesoderm |
|
|
Between which weeks does the embryo begin to fold?
|
Between weeks 3 and 4.
|
|

Not that this cross-section goes up and down the length of the embryo and as it grows, the intraembryonic coeoloms become bigger and bigger and coalesce into that U-shape. What begins to happen then and what week is this?
|
The embryo begins to fold in the 4th week.
|
|
|
What does the intraembryonic coelom become?
|
Pericardial cavity.
|
|
|
Note - you largely skipped 9/15 10a lecture 13:29 to 22:41 bc of the confusing detail.
|
Note - you largely skipped 9/15 10a lecture 13:29 to 22:41 bc of the confusing detail.
|
|
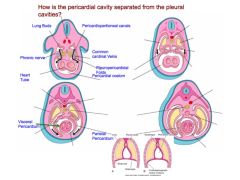
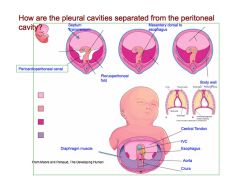
Review this slide explaining how the pericardial cavity is separated from the pleural cavity. It works like this:
Outgrowths from the lungs dissect the lateral wall of the pericardioperitoneal canal. These outgrowths eventually fuse with the other side and the mesoderm of developing esophagus to form the perietal layer of the paricardial sac. (see 9/15 lecture pre 30:00 mark p. 14) Note: When does this all happen? |
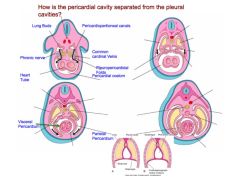
Review this slide explaining how the pericardial cavity is separated from the pleural cavity. It works like this:
Outgrowths from the lungs dissect the lateral wall of the pericardioperitoneal canal. These outgrowths eventually fuse with the other side and the mesoderm of developing esophagus to form the perietal layer of the paricardial sac. Note: End of week 4 |
|
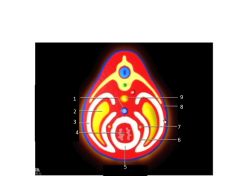
Name the structures. Where did the white and red layers derive from?
|
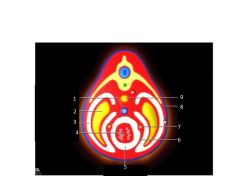
1. IVC
2. Lung 3. Pleaural cavity 4. heart 5. pericardial cavity 6. Fibrous pericardium 7. phrenic nerve 8. thoracic wall 9 esophagus White layers are from the somatic membrane and form the perietal pleura and perietal pericardia. The red layer is from the splanchnic layer and forms the visceral pleura. |
|
|
The mediastinum is located between the ___a___ and contains the __b__.
|
a. Pleural cavity
b. Pericardial cavity |
|
|
What is a synonym for peritoneal cavity?
|
Abdominal cavity.
|
|
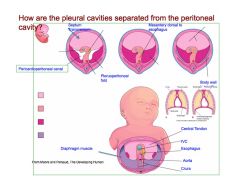
How the pleural cavity is separated from the peritoneal cavity:
The diaphragm has several component parts that come together in the pericardioperitoneal cavity: 1. Pluroperitoneal membrane 2. Septum transversum - a lg mass of mesoderm that is caudal to the heart and forms an incomplete partition bn the thoracic cavity and the abdominal cavity. 3. Dorsal mesentary of esophagus 4. Somatic myoblasts that invade the developing diaphragm via "crura" attached to the vertebral column to form the muscular layer of diaphragm. **These parts merge together to form the diaphragm. Note: When does this all happen? |
How the pleural cavity is separated from the peritoneal cavity:
The diaphragm has several component parts that come together in the pericardioperitoneal cavity: 1. Pluroperitoneal membrane 2. Septum transversum - a lg mass of mesoderm that is caudal to the heart and forms an incomplete partition bn the thoracic cavity and the abdominal cavity. 3. Dorsal mesentary of esophagus 4. Somatic myoblasts that invade the developing diaphragm via "crura" attached to the vertebral column to form the muscular layer of diaphragm. **These parts merge together to form the diaphragm. Happens at end of week 5. |
|
|
1. What happens if the caudal opening of the pericardioperitoneal opening remains patent?
2. What problems arise from this? 3. What precursor did not close completely? |
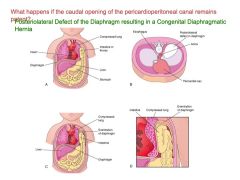
1. Bowel, and/or stomach and/or liver might end up in the pleural space.
2. Causes hypoplastic lung development and/or problems in pleural circulation. 3. The pleuroperitoneal cavity does not close completely. |
|
|
What the condition called when the pericardioperitoneal membrane doesn't close completely and bowel, or stomach, or liver enters the pleural space?
|
Diaphragmatic hernia.
|
|
|
What are typically included in the "lower respiratory system'?
|
The lungs and trachea. (Sometimes the larynx is included)
|
|
|
What does the lung derive from?
|
Endoderm and splanchnic mesoderm. The endoderm forms the larynx, trachea, bronchi, and lungs. The mesoderm forms the wall structures of bronchi, cartilage, and elastic tissues.
|
|
|
The lung first develops from the lung primordium. What is that and where does it grow out of?
|
The primordium arises as a diverticulum from the ventral midline foregut.
|
|
|
What does the initial diverticulum from the ventral midline foregut turn into?
|
The trachea.
|
|
|
When the trachea branches what do the branches turn into? What does the that brach into?
|
The first branches off the trachea is the primary bronchi then it's the lobar bronchi (there are 2 for the left and 3 for the right).
|
|
|
What can happen if the lung development is affected during embryonic period?
|
Inadequate partitioning - causing a Tracheoesophageal Fistula.
|
|
|
If you found that your donor body has an extra lobe in its left lung, what phase of development would this have occured?
|
Embryonic (bn 4-7 weeks)
|
|
|
1. In regard to lung development, what comes after the embryonic phase? 2. How long does it last? 3. Why is it called this? 4. What is primarily forming during this phase?
|
1. Pseudoglandular phase
2. Between weeks 6 and 16. 3. It like a gland at this phase 4. A lot of branching is happening during this period. |
|
|
1. In lung development, it's embryonic phase, pseudoglandular phase, and then the...?
2. What weeks does this happen? 3. What two things happen in this phase? |
1. Canalicular phase
2. Between weeks 16-26 3. Capillary density increases and endodermal epithelium will form two types of pneumocytes: flat and cuboidal |
|
|
1. After the canalicular phase, what is the next phase of lung developement?
2. When does it occur? 3. What is the major characteristic of this phase? |
1. Terminal sac phase.
2. week 26-birth 3. Epithelium in terminal sacs becomes very thin and close to capillaries. |
|
|
1. What is the phase after terminal sac phase?
2. How long does it last? 3. What is major characteristic? |
1. Alveolar phase.
2. 32 weeks - 8 years. 3. It's when alveolar development is really proliferative. Alveolar formation begins by subdivision of terminal sacs (septation) and alveolar septum (walls) become thinner. |
|
|
Although covered on previous NC, describe how alveoli form.
|
They form by subdivisions of terminal sacs (septation) and their walls become thinner.
|
|
|
What percentage of alveoli are formed postnatally?
|
~95%
|
|
|
What three changes must occur in the lungs at birth to allow breathing?
|
1. Pulmonary changes: fluid replaced by air
2. Circulatory changes: cardiac shunts close, pulmonary vessels fill 3. Neural: breathing, sympathetic activation. |
|
|
What disorder is caused by insufficient fluid production in the prenatal lung?
|
Hypoplastic lung
|
|
|
What condition is caused when all the fluid is not removed from the lung at birth?
|
Transient tachypnea (or wet lung)
|
|
|
What does pulmonary surfactant do? What is it produced by?
|
It modulates the air/liquid interface to reduce the surface tension. It is produced by Type II cells.
|
|
|
Production of surfactant begins toward the end of which period? What does this mean in terms of survival potential of pre-mature babies?
|
It begins toward the end of the canalicular period. There's a significant increase in production of PS at 35 weeks which means that's the earliest a baby can survive.
|
|
|
Pulmonary surfactant is a mixture of what three components?
|
1. Phospholipid
2. Protein 3. Antioxidant |
|
|
Bottom line: what does surfactant do?
|
It prevents the alveoli from collapsing on itself after exhalation. If it did, it would be extremely hard to open the alveoli up again after inhaling.
|
|
|
What are the symptoms of respiratory distress in babies?
|
Rapid breathing
flaring nostrils chest retractions expiratory grunt often cyanotic (blue) rapid heart rate anxious expression |
|
|
Which newborns are most at risk to experience respiratory distress?
|
Premature infants, males, mothers with poorly controlled diabetes
|
|
|
What is hyaline? How is it formed?
|
It is a acellular debris and serum. It is formed when you have type I alveolar cell injury, then a breakdown of air/capillary barrier then serum leaks into alveolar lumen and finally you have hyaline membrane with disrupted surfactant function.
|
|
|
What causes RDS?
|
It's an inability to keep alveoli filled with air. Usually from a decrease in surfactant production that results in poor compliance of lung tissue, atelectasis due to alveolar collapse, engorgement of pulmonary capillaries, and formation of a hyaline membrane.
|
|
|
How can surfactant related RDS be predicted?
|
By measuring the ratio between lecithin/sphingomyelin. If greater than 2, ok. If bn 1.5-1.9, 50% with RDS, if less than 1.5, 73% with RDS.
|
|
|
What single molecule is the best predictor of lung maturity?
|
Phosphatidylglycerol (PG)
|
|
|
How can fetal lung maturation be enhanced?
|
1. Administering glucocorticoid to mother before delivery
2. Administer artificial surfactant to newborn. |

