![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
12 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are some differentials for primary scaling disorders?
|
Primary idiopathid seborrhea
Follicular dystrophy/dysplasia Vitamin A responsive dermatitis Sebaceous adenitits Ichtyosis Nasodigital hyperkeratosis Ear margin dermatosis |
|
|
|
What are some differentials for secondary scaling disorders?
|
Pruritic:
parasitic: cheyletiellosis, Sarcoptes hypersenitivity: insect, food atopy infection: pyoderma, Malassezia Non-pruritic: infection: demodecosis, dermatophytosis endocrine: hypothyroidism, hyperadrenocorticism, sex hormone nutritional: fatty acid deficiency, zinc responsive autoimmune: pemphigus foliaceus, pemphigus erythematous environmental: low humidity, excessive shampooing neoplasia: epithliothropic lymphoma, actinic keratosis, SSC |
|
|
|
How would you approach disorders of keratinisation diagnotically?
|
1) Signalment, history, PE & the usual
PRURITIC or NON-PRURITIC? 2) Assume scaling is secondary initially & do scarpingsm brushings, cytology, woods lamp & fungal culture 3) If scaling & pruritus: persistent evaluate for hypersensitivity 4) If non-ruritic or pruitus resolves but scaling perists: -> evaluate environment & any topicals used (shampoos etc.) -> biochem, CBC, UA +/- additional tests: > evaluate for endocrinopathy, metabolic disease, autoimmune & neoplasia |
|
|
|
What is the difference between a keratolytic and keratoplastic therapeutic agent?
|
Keratolytics promote softening and dissolution of the stratum corneum, while keratoplastics normalize keratinization
|
|
|
|
Which topicals would you consider to treat seborrheic disoders?
|
Elimination or control of underlying causes is essential in secondary scaling disorders. Specific management of seborrhea entails both topical and systemic therapy.
Topical therapy is symptomatic and is the major management strategy. |
|
|

|
Primary (idiopathic) seborrhea
|
probably genetic defect in epidermis metabolism, begins in young dogs and CS are progeressive
lesions primarily ventral thorax predipsoed to 2ndary bacterial and Malasezzia infections |
|
|

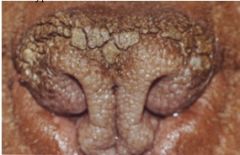
Nasodigital hyperkeratosis
Nasal planum: hard, dry, rough and scaly hard,crackedpads, fissures, erosions with pain on walking |
Syndromes of hyperkeratinisation or parakeratosis of the nasal planum, footpads or both can be
• a hereditary, congenital disorder in some breeds • idiopathic (primary keratinisation disorder) • a feature of underlying disorders, eg. distemper, pemphigus foliaceuas, lupus, cutaneous lyphoma... Management • Debridement of excess keratin under anaesthesia • Hydration, keratolytic agent • Topical medications such as petroleum jelly, dry skin lotions, prpylene glycol, tretinoin. • Consider retinoids. |
|

|

Sebaceous adenitis
group of uncommon idiopathic dermatoses in which an inflammatory reaction is directed against sebaceous glands likely hereditary, may improve and regress spontaneously |
Primarily young to middle aged dogs, generally bilaterally symmetrical, non-pruritic and dominated by abnormal keratinisation
|
|

|
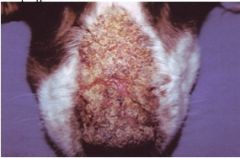
Zinc responsive dermatoses
Bilaterally symmetrical crusts around eyes, mouth, chin and ears, perineum, limbs Hyperkeratosis and crusts on elbows, pressure points, footpads Dry harsh dull coat Ceruminous otitis externa |
These are rare, nutritionally responsive scaling diseases due to either
• Defective Zinc absorption despite adequate Zn in diet: o A genetic defect in intestinal Zn absorption: huskies, malamutes, bull terriers. o High phytate diets (high calcium, high soy or corn diets) bind Zn • Rapidly growing puppies fed Zn-deficient diets Dx: S, Hx, PE & skin biopsy |
|
|
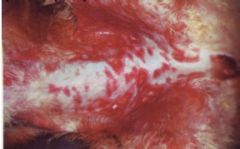
WWhat is the pemphigus complex and which is the most common form?
|
Pemphigus are uncommon immune mediated disorder in which autoantibodies are directed against keratinocyte desmosomal proteins. This causes loss of cohesiveness between keratinocytes and the formation of intraepidermal acantholysis and intraepidermal blister
Pemphigus foliaceous |
Dx: cytology to look for ancatholytic cells, skin biopsy to confirm
Tx: prednisolobe, tapering to lowest effective dose azathioprin(dogs)/chloramucil(cats) if no remission or unacceptable side effects |
|
|
Systemic Lupus Erythematosus (SLE)
|
SLE is an uncommon, multisystemic immune mediated disorder of dogs and cats in which a wide range of autoantibodies are produced against nuclear or cytoplasmic antigens
Cutaneous lesions can include alopecia, erythema, cutaneous or mucocutaneous vesicles, bullae and ulcers, footpad ulcers and hyperkeratosis, panniculitis and nasal dermatitis. Lesions may be multifocal or generalised, commonly involve sparsely haired skin and are induced or exacerbated by exposure to sunligh |
Systemic CS
• fever - always pressent • shifting lameness, joint swelling - very common • proteinuria - common • dermatologic signs - common • haemolytic anaemia • immune mediated thrombocytopenia • immune mediated leukopenia • polymyositis • pleuropericarditis • CNS signs |
|

|
Discoid Lupus Erythematiosus
DLE is a relatively common immune mediated disease of dogs but is rare in cats. It is a dermatologic disease with no systemic involvement depigmentation, erythema and scaling of the nose, which progresses to a smooth atrophy of the architecture of the nasal planum |
Diagnosis is made by biopsy and histopathology.
Treatment involves Avoidance of sun exposure, use of sunscreens topical therapy with glucocorticoids, tacrolimus or cyclosporine oral prednisolone and vitamin E oral doxycycline may be effective |

