![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
4 categories of CVD
|
1) heart disease
2) hypertension 3) stroke 4) other CVD |
|
|
Circulatory system composed of:
|
1) the blood (circulating material)
2) the heart (pump) 3) blood vessels (conduit) |
|
|
Circulatory system
|
series of blood vessels that connects the heart to tissues. circulation of waste and nutrients carried by blood
|
|
|
Primary Function of Circulatory System
|
1) Transportation: oxygen, glucose, hormones, heat, and waste
2) Protection and repair: a) fight against invading microorganisms and cancerous cells b) wound repair, blood clotting |
|
|
Composition of Blood
|
Top: serum/plasma
middle: WBC, platelets bottom: RBC (heaviest) |
|
|
hematocrit
|
blood cells (99% RBC) as a % of total blood volume
|
|
|
Why is hematocrit in men>women?
|
Because of the male hormone testosterone which is responsible for hormone called erythopoitin by kidney, which is responsible for synthesis of RBC. This is why males have higher value of hematocrit.
Males have adapted to larger O2 consumption sometimes. |
|
|
Properties of Whole Blood: Fraction of body weight, volume, temperature, pH, viscosity (relative to water), mean RBC count, platelet counts, total WBC counts
|
Fraction of body weight= 8%
volume= Females: 4-5 L Males: 5-6 L temperature: 38 degrees C pH: 7.35-7.45 viscosity: whole blood: 3.5-5.5 plasma: 1.5-2.0 mean RBC count: Females: 4.8 million/microliter Males: 5.4 million/microliter Platelet counts: 130,000-360,000/microliter WBC count: 4-11k/microliter |
|
|
Plasma Components
|
water (92% by weight)
nutrients (glucose, lipoproteins, amino acids) proteins (albumin, IGs, fibrinogen, hormones, enzymes) ions- HCO3-, Ca++, etc respiratory gases: O2, CO2, NO |
|
|
Plasma Protein: Function and Production?
|
Function: -exert an osmotic pressure- maintain plasma volume
-buffer pH changes Production: in the liver, except antibodies (by lymphocytes) |
|
|
plasma vs serum
|
serum is plasma vs clotting factors (fibrin)
|
|
|
Blood cells
|
Erythrocytes (RBC)
platelets (cellular fragments) leukocytes (WBCs) -granulocytes: Neutrophils, basophils, eosinophils -agranulocytes: monocytes, lymphocytes |
|
|
RBC (Erythrocytes) Appearance
|
Biconcave disc shape
Why? increases SA to allow for diffusion of O2 to occur and also thin center allows O2 to readily diffuse into center of the cell. Flexible membrane- so RBC can bend and pass through thinnest capillaries |
|
|
RBC structure
|
Primary cell content is hemoglobin, a protein that carries O2, CO2, CO, and NO
no nucleus or mitochondria- no DNA or RNA life span ~120 days (because can't produce protein) replace RBC regularly |
|
|
Functions
|
1) primary functions: transport oxygen from the lung to tissue cells and carbon dioxide from tissues to the lung
2) buffer blood pH |
|
|
Production of Erythrocytes
|
Hematopoiesis
Erythropoiesis |
|
|
Hematopoiesis
|
whole blood cell production (WBC and RBC)
|
|
|
Erythropoiesis
|
refers specifically to red blood cell production
|
|
|
where are red and white blood cells produced?
|
red bone marrow
|
|
|
how much blood cells are made per day? (on average)
|
100 billion blood cells/day on average.
|
|
|
Hematopoiesis
|
stages:
embryonic: up to 2 months- yolk sac fetal: 2-7 months- liver, spleen, lymph nodes after birth: bone marrow -up to 5 years: bone marrow of essentially all bones -after 20 years: bone marrow of the membranous bones (vertebrae, sternum, ribs, ilia); proximal portions of humeri and tibiae. |
|
|
RBC stem cell
|
hemacytoblast
|
|
|
Stages of Erythropoiesis
|
Hemocytoblast-->proerthyroblast-->erythroblast -->normoblast-->reticuloblast--> erythrocyte
|
|
|
What happens to mature RBC
|
they exist bone marrow and enter blood
|
|
|
what is special about the capillaries near bone marrow?
|
they have large holes to allow the RBC produced in bone marrow to enter
|
|
|
Regulation of erythropoiesis
|
regulated by renal O2 content- by kidney that senses O2
when low O2 sensed in renal blood, kidneys secrete hormone erythropoietin. EPO acts on red bone marrow to stimulate production of RBC. in fetus- liver is EPO producer in adults- kidney is PRIMARY EPO producer |
|
|
epogen (procit)
|
used to boost RBC production in patients
|
|
|
Drop in renal blood oxygen level can result from:
|
1. reduced # of RBC
- due to excessive blood loss or RBC destruction in certain diseases 2. reduced availability of oxygen - if you are at higher altitude or patient with pneumonia 3. increased demands for oxygen - exercise all can stimulate production of EPO |
|
|
Ways to increase RBC count in sports:
|
Legal: raise RBC count by training athletes at high altitudes- body will adapt to reduced O2 supply to produce more RBC
Illegal: Use erthyropoietin, androgen, or their analogs- receptors located in kidneys- enhance release of EPO from kidneys. Blood doping- store blood, body compensates for loss of blood by making more RBC, put blood back in before competition and then have more RBC temporarily. |
|
|
Potential problem with HCT increase
|
increases blood velocity- increases resistance to blood flow and in turn increases blood pressure
|
|
|
polycythemia
|
disease where %RBC in total blood volume is larger than normal.
|
|
|
Erythrocyte disorders
|
Anemia: blood has abnormally low oxygen-carrying capacity
characterized by a low hematocrit Polycythemia |
|
|
Types of Anemia:
|
Nutritional- deficiency of Fe or folic acid- vegetarians at risk
Pernicious- lack of vitamin B12, important for absorption of Fe into RBC's Aplastic- deficiency of erythroid stem cells Renal- may occure during chronic KD or renal failure where EPO production is low Hemorrhagic- caused by excessive blood loss Hemolytic- cased by RBC rupture- seen with malaria and occasionally with severe prolonged exertion Abnormal Hb- eg thalassemias and sickle-cell anemia, which are caused by genetic defects. |
|
|
Polycythemia
|
increased erythrocytes that increases viscosity of blood, causing it to flow sluggishly
-reduces O2 delivery -increases resistance, increases blood pressure |
|
|
common causes of polycythemia
|
-bone marrow cancer
-high altitudes- response to low O2, patients with chronic lung disease or cardiac failure. |
|
|
Leukocytes
|
Granulocytes: contain specialized membrane bound cytoplasmic granules
Neutrophils, Basophils, Eosinophils Agranulocytes: lack obvious granules monocytes and lymphocytes |
|
|
Function of Leukocytes
|
defense against disease
Leukocytes form a mobile army that helps protect the body from damage by bacteria, viruses, parasites, toxins, and tumor cells |
|
|
Life span of Leukocytes
|
-several hours to several days for the majority
-many years for a few memory cells |
|
|
Neutrophils
|
40-70% WBCs
nucleus multilobed duration of development: 6-9 days life span: 6 days to a few days function: phagocytize bacteria |
|
|
Eosinophils
|
1-4% WBC
nucleus bilobed duration of development: 6-9 days life span: 8-12 days function: 1) kill parasite worms 2) destroy antigen-antibody complexes 3) inactivate some inflammatory chemical of allergy |
|
|
Basophils
|
0.5% WBC
nucleus lobed development: 3-7 days life span: a few hours to a few days function: 1) release histamine and other mediators of inflammation 2) contain heparin, an anticoagulant |
|
|
Lymphocytes
|
T and B cells
20-45% WBCs nucleus spherical or indented development: days to weeks life span: hours to years function: mount immune response by direct cell attack (T cells) or via antibodies (B cells) |
|
|
Monocytes
|
4-8 % WBCs
Nucleus U shaped Development: 2-3 days life span: months to years function: phagocytosis and develop into macrophages in tissues |
|
|
Leukemia
|
group of cancerous conditions of WBC
extraordinarily high number of abnormal (cancerous) leukocytes - abnormal immature cells reduction of RBCs and platelets - lead to internal bleeding and anemia because WBC immature, cannot perform defense even though there is a high number. most common cause of death is infection and hemorrhage from the low number of platelets in leukemia |
|
|
Platelets
|
not cells, cytoplasmic fragments of extraordinarily large (up to 60 micrometers in diameter) cells called megakaryocytes.
Normal platelet count= 130,000-400,000 microliters |
|
|
Function of platelets
|
1) secrete vasoconstrictors that cause vascular spasms in broken vessels
2) form temporary platelet plugs to stop bleeding 3) secrete chemicals that attract neutrophils and monocytes to the site of inflammation 4) secrete growth factors that stimulate mitosis in fibroblasts and smooth muscle and help maintain the linings of blood vessels 5) dissolve blood clots that have outlasted their usefulness |
|
|
hemostasis
|
stoppage of bleeding
|
|
|
Stoppage of Bleeding
|
1) vascular spasms: if you have injury of a vessel, first thing that happens in vasoconstriction.
2) platelet plug formation 3) blood clotting/coagulation |
|
|
Platelet Plug Formation
|
platelets stick to damage parts.
as you injure the vessel, collagen is exposed, because of this plasma protein called vWF can bind to exposed collagen and in turn the platelets can attach to vWF so we prevent wash away of platelets by blood flow. collagen also activates platelets to develop spiny processes to help them adhere to the collagen. activated platelets can release chemicals to make them attract more platelets to create a stronger plug- reinforce strongs platelet aggregation |
|
|
Blood clotting/coagulation
|
formation of blood clot over blood clot forms better seal over damaged vessel
many clotting factors in plasma are involved in clotting these factors are inactive in the blood activated when: 1) blood vessel is broke or 2) blood flow slows down sequential activation of the clotting factors finally leads to the formation of fibrin meshwork. blood cells are trapped in fibrin meshwork to form a hard clot |
|
|
Fibrinogen--> fibrin
|
catalyzed by thrombin
|
|
|
Coagulation disorders
|
Thrombosis, Thrombus, Embolus, Embolism, Infarction
|
|
|
Thrombosis
|
abnormal clotting of blood in unbroken vessel
|
|
|
Thrombus
|
clot that attaches to the wall of blood vessel
|
|
|
embolus
|
clot that comes off the wall of blood vessel and travel in the blood stream
(thrombus that has been mobilized) |
|
|
embolism
|
blockage of blood flow by an embolus that lodges in a small vessel
|
|
|
infarction
|
refers to cell death that results from embolism. infarction is responsible for most strokes and heart attacks
|
|
|
Bleeding disorders
|
1) thrombocytopenia
2) hemophilias 3) deficiency of clotting factors dure to impaired liver function |
|
|
Thrombocytopenia
|
number of circulating platelets is deficient (less than 50k)
causes spontaneous bleeding from small blood vessels all over the body. |
|
|
Hemophilias
|
hereditary bleeding disorder due to deficiency of clotting factors.
|
|
|
Functions of the heart
|
1) Generates blood pressure (push blood through the circulation)
2) routes blood - heart separates systemic and pulmonary cirulation 3) ensures one-way flow - heart valves ensure one-way flow 4) regulates blood supply - changes in contraction rate and force match blood delivery to changing metabolic needs -most healthy people can increase cardiac output by 300-500% |
|
|
Heart failure
|
inability of heart of provide enough blood flow to maintain normal metabolism
|
|
|
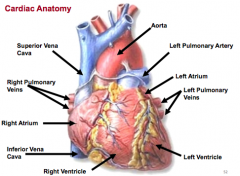
Cardiac Anatomy
|
|
|
|
Why are there no valves between the atria and veins?
|
because atrial pressure if often times relatively low, not much higher than venous pressure. the pressure difference is not big, dont need a valve to ensure unidirectional flow. during atrial contraction, sites where vena cava enter atria are collapsed a little so the cross sectional area is small, small orphes prevents back flow
|
|
|
atrioventricular valves
|
located between the atria and ventricles: tricuspid and bicuspid
|
|
|
semilunar valves
|
shaped like half moons- separate ventricle and vessels: aortic and semilunar
|
|
|
atria of the heart
|
receiving chambers of the heart
|
|
|
where does blood enter the heart from
|
the right atria from superior and inferior vena cava and coronary sinus (from heart)
|
|
|
where does blood enter left atria from?
|
pulmonary veins
|
|
|
Why are atrial walls thin?
|
Litter resistance to flow in atria
|
|
|
Ventricles
|
discharging chambers of heart
|
|
|
Right ventricle
|
pumps blood into the pulmonary trunk
Pulmonary circulation |
|
|
Left ventricle
|
pumps blood into the aorta and into all the issues
|
|
|
Why are ventricular walls so thick especially LV?
|
there is a high resistance to flow from higher ventricular pressure. left side has higher pressure than right side. LV working against higher pressure to push blood through- so it needs a strong muscle wall.
|
|
|
What is the major difference between the right and left side?
|
The after load which is also the pressure of which you have to push blood through. left side has much higher after load of pressure than right side
|
|
|
endocardium
|
inner layer and consists of endothelial tissue that lines the inner surface of the heart and cardiac valves
|
|
|
myocardium
|
middle layer and is composed of muscle fibers that enable the heart to pump
|
|
|
epicardium
|
outer layer, is tightly adherent to the heart and the base of the great vessels.
|
|
|
pericardium
|
thin, fibrous, double-layered sac that surrounds the heart
|
|
|
Coronary arteries
|
are perfused during diastole (opposite as systemic system)
an increase in HR shortens diastole and can decrease myocardial perfusion patients, particularly those with coronary artery disease, can develop myocardial ischemia (inadequate O2 supply) when heart rate accelerates. |

