![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
Stroke |
Sudden loss of neurological function caused by interruption of the blood flow to the brain |
|
|
What are the two types of strokes? |
1. Ischemic 2. Hemorrhagic |
|
|
Ischemic Stroke |
Results when a clot blocks or impairs blood flow |
|
|
What type of stroke is most common? |
Ischemic, 80% |
|
|
Hemorrhagic stroke |
Occurs when blood vessels rupture, causing leakage of blood around the brain |
|
|
To be classified as a stroke, neurological deficits must persists for how long? |
24 hours |
|
|
Paralysis in stroke is called |
Hemiplegia |
|
|
Weakness in stroke is called |
Hemiparesis |
|
|
For cells to survive, how much blood flow is required? |
20-25% |
|
|
What are major risk factors for CVA? |
Hypertension Heart Disease Diabetes Mellitus Disorders of heart rhythm (end stage renal disease) (sleep apnea) |
|
|
What are the five stroke warning signs? |
1. Sudden numbness or weakness of the face, arm or leg, one side of the body 2. Sudden confusion, trouble speaking or understanding 3. Sudden vision changes 4. Sudden trouble walking, dizziness, LOB, coordination 5. Sudden severe headache |
|
|
Cerebral edema |
ischemic strokes produce edema that maximizes by 3-4 days. Disappears by 2-3 weeks |
|
|
Circle of Willis |
Circular anastomosis that supplies blood the brain |
|
|
Name the Circle of Willis |
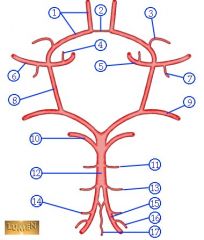
|
|
|
Circle of Willis Picture |
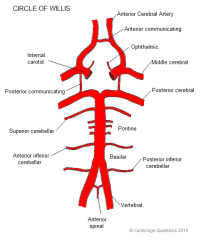
|
|
|
Vertebral Artery |
Branches off of subclavian, combines with other vertebral artery to make basilar artery |
|
|
Basilar Artery |
Arises from union of 2 vertebral arteries, bifuricates to form the posterior cerebral arteries |
|
|
Posterior Communicating Artery |
Connects the posterior cerebral arteries with the internal carotid arteries to complete the circle of Willis |
|
|
External Carotid artery |
Supplies circulation to the face |
|
|
Internal Carotid Artery |
Supplies cerebral hemispheres |
|
|
Anterior Cerebral Artery |
Branch of the internal carotid artery. |
|
|
What does the Anterior Cerebral Artery Supply? |
the superior border for the parietal and frontal lobes and subcortical structures |
|
|
Anterior Cerebral Artery Occlusion Results |
Contralateral weakness and sensory loss involving LE apraxia Incontinence Significant memory and behavioral deficits |
|
|
Blood Supply to brain |
|
|
|
Middle Cerebral Artery |
Branch of the internal carotid artery. |
|
|
What does the middle cerebral artery supply? |
The lateral surface of the brain and deep portions of frontal and parietal lobes |
|
|
What is the most common type of CVA? |
Middle Cerebral Artery Occlusion |
|
|
Middle Cerebral Artery Occlusion Results |
Contralateral weakness and sensory loss of the face and UE Aphasia Contralateral homonymous hemianopia
|
|
|
What do the vertebral arteries supply? |
The cerebellum, and medulla |
|
|
What does the basilar artery supply? |
Pons, internal ear, and cerebellum |
|
|
Vertebrobasilar Artery Occlusion |
Cranial nerves affected Ipsilateral and contralateral symptoms Often fatal |
|
|
What does the posterior cerebral artery supply? |
Occipital lobe and temporal lobe |
|
|
Posterior Cerebral Artery Occlusion Results |
Contralateral sensory loss Pain Memory Deficits Visual agnosia Cortical blindness |
|
|
Rood Approach |
involves superficial cutaneous stimulation using stroking, brushing, icing, or muscle stimulation with vibration tendon tapping and joint compression to evoke voluntary contraction or inhibition of proximal muscle |
|
|
Rood's Four Basic Principals |
1. Sensory input is required for normalization of tone and evocation of desired muscular response 2. Sensory motor control is based on development 3. Movement is purposeful; engagement in activities is required to produce a normal response 4. Repetition of movement is necessary |
|
|
Stages of Motor Recovery Post CVA |
1. flaccidity 2. Spasticity 3. Reflexes 4. Voluntary movements 5. coordination 6. motor programming |
|
|
Hypotonicity |
Presents immediately after a stroke and is due to cerebral shock. Short lived |
|
|
Hypertonicity |
Emerges in 90% of cases on affected side Generally in antigravity muscles |
|
|
facilitation |
Intervention to increase the likelihood of a desired response
|
|
|
Inhibition |
intervention to decrease the likelihood of an undesired response |
|
|
Facilitation for hypotonic muscles |
Quick stretch Tapping Vibration Brushing Icing Joint approximation |
|
|
Inhibition for hypertonic muscles |
Inhibitory pressure Slow stroking Neutral warmth Gentle rocking Prolonged stretch Prolonged Ice |
|
|
Initially in a stroke, what reflex response happens? |
Hyporeflexia with flaccidity |
|
|
When spasticity emerges, what reflex response happens? |
Hyperreflexia Ex: deep tendon reflex, clonus, clasp-knife reflex, positive babinski |
|
|
Tonic reflexes |
movement of head or position of body may elicit an obligatory change in resting tone or movement of the extremities: ATNR most common |
|
|
Associated reaction |
Unintentional movement of the hemiparetic limb caused by voluntary action of another limb or by other stimuli.
See in strong spasticity cases! |
|
|
What are the three main stages of recovery by Bobath? |
1. Flaccid stage 2. Spasticity 3. Selective recovery |
|
|
Brunnstrom Stages (UGHHH AGAIN??) |
Stage 1-flaccid Stage 2-spasticity begins, minimal voluntary movement Stage 3-Further increase in spasticity, voluntary control of synergies Stage 4-Some movement combinations out of synergy, spasticity beginning to decrease Stage 5- more difficult movement combinations are learned Stage 6-Spasticity disappears; joint movements become possible and coordination approaches normal |
|
|
Non-equilibrium coordination tests |
address components of limb movements |
|
|
Sharp/Dull Discriminations |
indicates function of protective sensation. Alternate between pin and dull end and patient tells you if it is a sharp or dull pain |
|
|
Light Touch test |
Lightly apply a cotton swab against patients skin. They say "yes/no" if they feel it. |
|
|
Kinesthesia |
Sense of movement |
|
|
Proprioception |
awareness of one's position of body in space |
|
|
2 point discrimination |
The ability to differentiate one stimulus from two |
|
|
Stereognosis |
The ability to recognize objects by touch |
|
|
orientation |
the ability to comprehend and to adjust oneself with regard to time, location, and identity of persons |
|
|
Modified Ashworth Scale |
Scale for grading spasticity |

