![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
What is HTN a risk factor for?
|
- Coronary artery disease (CAD)
- Stroke - Heart disease leading to Congestive Heart Failure (CHF) |
|
|
What are the types of HTN?
|
- Primary / Essential (95%)
- Secondary (eg, renal, endocrine, cardiovascular, neurologic) - Malignant / Accelerated (5%) |
|
|
What are the types of secondary HTN / causes?
|
- Renal (majority): parenchymal and vascular
- Endocrine: adrenocortical, thyroid, and pregnancy - Cardiovascular: structural (coarctation of aorta), vasculitis - Neurlogic: sleep apnea, increased intracranial pressure |
|
|
What percentage of hypertensive patients have the malignant / accelerated type?
|
~5%
|
|
|
What are the genetic factors that contribute to primary / essential HTN?
|
Rare single gene disorders affecting:
- Aldosterone metabolism - Distal tubular resorption of Na+ Polymorphisms affecting: - Ang II Receptor - Na+ Handling - Smooth Muscle Cell Growth |
|
|
What are the environmental factors that contribute to primary / essential HTN?
|
- Stress
- Salt intake - Obesity - Smoking - Physical inactivity |
|
|
What is the mechanism of pathogenesis of primary / essential HTN??
|
- ↓ renal Na+ excretion → ↑ fluid volume
- ↑ vascular resistance d/t vasoconstriction and/or thickening of vessel walls |
|
|
What factors affect Cardiac Output?
|
- Blood volume (Na+, mineralocorticoids, ANP)
- Cardiac factors (HR, contractility) |
|
|
What factors affect Peripheral Resistance?
|
Humoral Factors
- Constrictors: AngII, catecholamines, thromboxane, leukotrienes, endothelin - Dilators: prostaglandins, kinins, NO Neural factors: - Constrictors: α-adrenergic - Dilators: β-adrenergic Local factors: - Autoregulation - pH - Hypoxia |
|
|
What are the characteristics of malignant hypertension?
|
- Uncommon (5% of patients w/ HTN)
- Diastolic >120 mmHg - Renal failure - Retinal hemorrhages, exudates, ± papilledema - More commonly younger patients, men, African-Americans * Rapidly progressive course (over 1-2 years) |
|
|
What is the HTN history of someone with malignant HTN?
|
- It can either begin in someone who was always normotensive
- It can also be superimposed on long-standing essential / primary HTN |
|
|
Which arteries does HTN affect?
|
- Large/medium arteries
- Small arteries/arterioles |
|
|
What are the characteristics of large/medium arteries in HTN?
|
- Accelerated atherogenesis (plaque-formation)
- Degenerative changes in vascular walls - Increased risk of aortic dissection and cerebrovascular hemorrhage |
|
|
What are the characteristics of small arteries / arterioles in HTN?
|
- Hyaline arteriolosclerosis may be present (more common in elderly)
- Hyperplastic arteriolosclerosis may be present (more common in malignant HTN) |
|
|
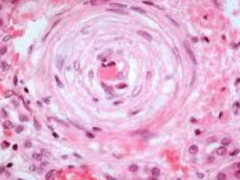
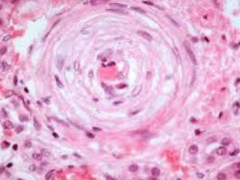
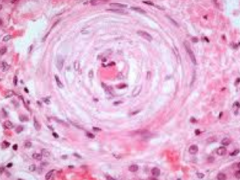
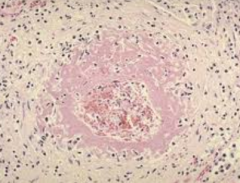
What are the characteristics of Hyaline Arteriolosclerosis
|
- Homogenous pink, thickening of vessels w/ narrowing of lumen
- Leakage of plasma across endothelium d/t HTN - Excess matrix production by smooth muscle cells occurs secondarily - "Benign" nephrosclerosis |
|
What kind of patients get Hyaline Arteriolosclerosis?
|
- Elderly patients
- Similar changes in diabetics (microangiopathy) |
|
|
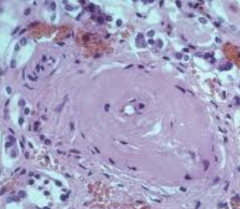
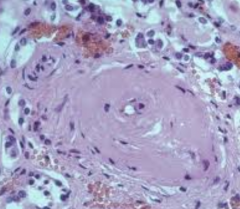
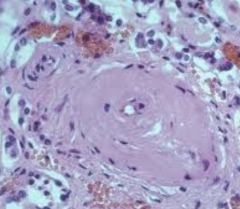
What are the characteristics of Hyperplastic Arteriolosclerosis
|
- Onion-skinning: concentric laminated walls with luminal narrowing
- D/t re-duplicated basement membrane and smooth muscle cells - Characteristic of malignant HTN |
|
What kind of patients get Hyperplastic Arteriolosclerosis?
|
Patients with malignant HTN
|
|
|
What are the characteristics of Necrotizing Arteriolitis?
|
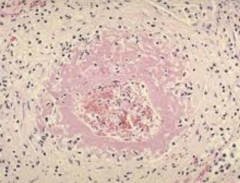
- Fibrinoid necrosis of arterioles (fibrin is leaking out of vessel wall, presence of inflammatory cells)
- Characteristic of malignant HTN |
|
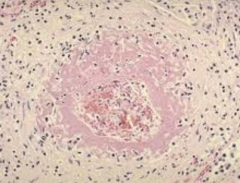
What kind of patients get Necrotizing Arteriolitis?
|
Patients with malignant HTN
|
|
|
What is the difference between systemic and pulmonary hypertensive heart disease?
|
- Systemic causes left sided heart changes
- Pulmonary causes right sided heart changes |
|
|
How do you diagnose a patient with systemic hypertensive heart disease?
|
- Concentric left ventricular hypertrophy in absence of other CV pathology
- Evidence of HTN >140/90 mmHg |
|
|
What are the morphologic characteristics of systemic hypertensive heart disease?
|
- Cardiomegaly: concentric hypertrophy w/o dilatation, >1.5 cm wall thickness, 500-600g
- Thickness of LV wall impairs diastolic filling and causes LA enlargement - Myocyte hypertrophy: increased myocyte size and nuclear enlargement |
|
|
What are the possible clinical outcomes of systemic hypertensive heart disease?
|
- Normal longevity
- Progressive ischemic heart disease (HTN potentiates ischemic heart disease) - Progressive renal damage or stroke - Progressive heart failure - Sudden cardiac death |
|
|
What happens to the brain in systemic hypertensive heart disease?
|
- Cerebral vessels affected by arteriolosclerosis are weakened and more likely to rupture → intracerebral hemorrhage
- Lacunar infarcts - Hypertensive encephalopathy (headaches, confusion, vomiting, convulsions, ↑CSF pressure) |
|
|
What happens to the kidneys in systemic hypertensive heart disease?
|
Benign HTN:
- Atrophic; granular, pitted surfaces - Hyaline arteriolosclerosis → ischemia and atrophy - Glomeruli may become sclerosed - Some of this is expected with age, but in HTN it is accelerated Malignant HTN: - Pinpoint petechial hemorrhages on surface - Fibrinoid necrosis of arterioles - Hyperplastic arteriolosclerosis and microthrombi → global ischemia |
|
|
What is Cor Pulmonale?
|
Another term for pulmonary hypertensive heart disease
|
|
|
What are the causes and morphology of acute pulmonary hypertensive heart disease?
|
- Cause: Massive pulmonary embolism
- Dilatation of RV w/o hypertrophy |
|
|
What are the causes and morphology of chronic pulmonary hypertensive heart disease?
|
- Cause: Chronic lung disease
- RV hypertrophy (up to 1 cm in thickness), secondary to pressure overload (almost or as big as LV) - Obstruction of pulmonary arteries / arterioles / septal capillaries |
|
|
What is the term for the inability of the heart to pump blood at a rate to meet the needs of active tissues?
|
Congestive Heart Failure (CHF)
|
|
|
What are the characteristics of Congestive Heart Failure (CHF)?
|
- Inability of heart to pump blood at a rate to meet needs of active tissues
- Slowly developing intrinsic deficit in contraction - Or it can only do at an elevated filling pressure |
|
|
What is the leading discharge diagnosis in hospitalized patients over 65 years?
|
Congestive Heart Failure (CHF)
|
|
|
What is the rate at which patients with symptomatic Congestive Heart Failure (CHF) die within 1 year?
|
45%
|
|
|
What are the possible mechanisms of Congestive Heart Failure (CHF) pathogenesis?
|
Abnormal load presented to heart:
- Acute: fluid overload, MI, valve dysfunction - Chronic: ischemic heart disease, dilated cardiomyopathy, hypertension Impaired ventricular filling: - Acute: pericarditis or tamponade - Chronic: restrictive cardiomyopathy, severe LV hypertrophy Obstruction d/t Valve Stenosis: - Chronic: Rheumatic valve disease (usually mitral valve) |
|
|
What are the acute causes of abnormal load presented to the heart? Outcome?
|
- Fluid overload
- MI - Valve dysfunction - Leads to Congestive Heart Failure (CHF) |
|
|
What are the chronic causes of abnormal load presented to the heart? Outcome?
|
- Ischemic heart disease
- Dilated cardiomyopathy - Hypertension - Leads to Congestive Heart Failure (CHF) |
|
|
What are the acute causes of impaired ventricular filling? Outcome?
|
- Pericarditis
- Tamponade - Leads to Congestive Heart Failure (CHF) |
|
|
What are the chronic causes of impaired ventricular filling? Outcome?
|
- Restrictive cardiomyopathy
- Severe LV hypertrophy - Leads to Congestive Heart Failure (CHF) |
|
|
What are the chronic causes of obstruction d/t valve stenosis? Outcome?
|
- Rheumatic valve disease (usually mitral valve)
- Leads to Congestive Heart Failure (CHF) |
|
|
What is the difference between systolic and diastolic Congestive Heart Failure (CHF)?
|
- Systolic: progressive deterioration of cardiac contractile function
- Diastolic: inability of heart to relax, expand, and fill sufficiently during diastole |
|
|
What are the causes of systolic Congestive Heart Failure (CHF)?
|
- Ischemic Heart Disease
- Pressure or volume overload - Dilated cardiomyopathy |
|
|
What are the causes of diastolic Congestive Heart Failure (CHF)?
|
- Massive left ventricular hypertrophy
- Amyloidosis - Myocardial fibrosis - Constrictive pericarditis |
|
|
What are some rapidly occurring compensatory mechanisms for Congestive Heart Failure (CHF)?
|
- Frank-Starling Mechanism
- Activation of Neurohumoral Systems |
|
|
What happens in the Frank-Starling Mechanism of rapid compensation to Congestive Heart Failure (CHF)?
|
- ↑Preload dilation → ↑end diastolic filling volume
- Helps sustain cardiac performance by enhancing contractility - Lengthened fibers contract more forcibly - Does result in increased wall tension and O2 requirements |
|
|
What happens in the activation of neurohumoral systems to rapidly compensate for Congestive Heart Failure (CHF)?
|
- Release of NE by cardiac nerves → ↑HR, ↑contractility, ↑vascular resistance
- Activation of Renin-Ang-Aldosterone system → ↑Na+ and ↑H2O resorption → ↑CO and ↑vasoconstriction - Release of ANP: secreted from atrial myocytes when dilated, causing vasodilation, diuresis |
|
|
What are some slow occurring compensatory mechanisms for Congestive Heart Failure (CHF)?
|
Cardiac Hypertrophy:
- Response to ↑ load occurring over weeks-months - Increased numbers of sarcomeres makes fibers visibly bigger - No hyperplasia |
|
|
How does the extent of hypertrophy vary with the cause of Congestive Heart Failure (CHF)?
|
- 600g: pulmonary HTN and ischemic heart disease
- 800g: systemic HTN, aortic stenosis, mitral regurgitation, dilated cardiomyopathy - 1000g: aortic regurgitation, hypertrophic cardiomyopathy |
|
|
What can cause a heart to hypertrophy to 600g?
|
- Pulmonary HTN
- Ischemic Heart Disease |
|
|
What can cause a heart to hypertrophy to 800g?
|
- Systemic HTN
- Aortic Stenosis - Mitral Regurgitation - Dilated Cardiomyopathy |
|
|
What can cause a heart to hypertrophy to 1000g?
|
- Aortic Regurgitation
- Hypertrophic Cardiomyopathy |
|
|
What are the patterns of hypertrophy?
|
- Concentric Hypertrophy
- Hypertrophy accompanied by Dilatation |
|
|
What causes Concentric Hypertrophy w/o Dilatation?
|
Pressure Overload:
- HTN - Aortic Stenosis |
|
|
What causes Hypertrophy w/ Dilatation?
|
Volume Overload:
- Mitral Regurgitation - Aortic Regurgitation |
|
|
What is the mechanism of pressure overload causing changes in the heart? What changes?
|
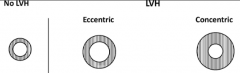
PRESSURE overload
→ ↑ SYSTOLIC wall stress → mechanical transducers → extracellular and intracellular signals → ventricular remodeling → PARALLEL sarcomeres → CONCENTRIC hypertrophy** |
|
|
What is the mechanism of volume overload causing changes in the heart? What changes?
|
VOLUME overload
→ ↑ DIASTOLIC wall stress → mechanical transducers → extracellular and intracellular signals → ventricular remodeling → SERIES sarcomeres → ECCENTRIC hypertrophy** |
|
|
What is pressure overload associated with (that makes it unique from volume overload)?
|
- ↑ Systolic wall stress
- Parallel Sarcomeres - Concentric Hypertrophy |
|
|
What is volume overload associated with (that makes it unique from pressure overload)?
|
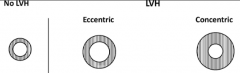
- ↑ Diastolic wall stress
- Series Sarcomeres - Eccentric Hypertrophy |
|
|
What are the characteristics of a myocyte in physiologic hypertrophy? Cause?
|
- Lengthens and stays same width
- Nucleus lengthens too - Eg., someone who runs marathons, pregnant woman |
|
|
What are the characteristics of a myocyte in concentric hypertrophy? Cause?
|
- Does not lengthen, just widens
- Nucleus widens - Due to pressure overload |
|
|
What are the characteristics of a myocyte in eccentric hypertrophy? Cause?
|
- Lengthens and gets narrower
- Nucleus widens (not as much as in eccentric hypertrophy) - Due to volume overload |
|
|
When the heart undergoes cardiac hypertrophy, what are the outcomes?
|
- Often evolves to cardiac failure
- ↑ myocyte size results in ↓ capillary density, ↑ inter-capillary distance, and ↑ fibrous tissue - ↑ Cardiac O2 consumption - Altered gene expression and proteins - Loss of myocytes d/t apoptosis - LV hypertrophy is a risk factor for sudden death |
|
|
What heart conditions lead to heart failure?
|
- Hypertension (pressure overload)
- Valvular disease (pressure and/or volume overload) - Myocardial Infarction (regional dysfunction w/ volume overload) - All lead to hypertrophy and/or dilation - Leads to cardiac dysfunction, characterized by: heart failure (systolic or diastolic), arrhythmias, neurohumoral stimulation |
|
|
What are some causes of left sided heart failure?
|
- Ischemic heart disease
- Hypertension - Aortic and mitral valve disease - Non-ischemic myocardial diseases (cardiomyopathies and myocarditis) * Primarily d/t progressive damming of blood w/in pulmonary circulation and diminished peripheral blood pressure and flow * |
|
|
What are some effects on the heart of left-sided heart failure?
|
- LV hypertrophy and often dilation
- Often results in mitral valve insufficiency - Secondary enlargement of LA → A Fib → stagnant blood in atrium → thrombus, embolic stroke |
|
|
What are some effects on the lungs of left-sided heart failure?
|
- ↑ Pressure in pulmonary veins → transmitted to capillaries and arteries
- Pulmonary congestion and edema - Presence of heart failure cells (hemosiderin-containing macrophages) - Dyspnea (shortness of breath), orthopnea (dyspnea when recumbent / lying down), and paroxysmal nocturnal dyspnea - When supine, venous return increases and diaphragms elevate - Rales (rattling sound) on exam |
|
|
What are some effects on the kidneys of left-sided heart failure?
|
- ↓ Renal perfusion activates Renin-Angiotensin-Aldosterone System → ↑ blood volume
- If perfusion deficit is severe → prerenal azotemia (impaired kidney function d/t low perfusion) |
|
|
What is the term for impaired kidney function d/t low perfusion?
|
Pre-renal Azotemia
|
|
|
What are some effects on the brain of left-sided heart failure?
|
- Cerebral hypoxia
- Encephalopathy |
|
|
What are the causes of right-sided heart failure?
|
- Usually secondary to left-sided failure
- Pulmonary hypertension - Primary myocardial disease - Tricuspid or pulmonary valvular disease |
|
|
What are the effects of right-sided heart failure usually due to?
|
Engorgement of systemic and portal venous systems
|
|
|
What are some effects on the heart of right-sided heart failure?
|
- RV responds to increased workload w/ hypertrophy and often dilatation
- Pericardial effusion |
|
|
What are some effects on the liver and portal system of right-sided heart failure?
|
↑ Pressure in portal vein leads to:
- Congestive hepatosplenomegaly - Cardiac cirrhosis - Ascites (abdominal swelling) |
|
|
What is cardiac cirrhosis?
|
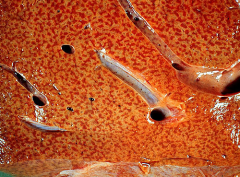
- Congestive hepatopathy, also known as nutmeg liver and chronic passive congestion of the liver
- Liver dysfunction due to venous congestion, usually cardiac dysfunction (right-sided heart failure) |
|
|
What are some effects on the kidneys of right-sided heart failure?
|
- Congestion
- Fluid retention - Peripheral edema - Azotemia (insufficient filtering of blood by the kidneys) |
|
|
Is Azotemia (insufficient filtering of blood by the kidneys) more prominent in left or right sided heart failure?
|
* More prominent in right sided heart failure
- R-sided HF causes venous congestion of kidneys - More impairment of function, secondary to lack of removal of metabolites in venous circulation (and if severe, decrease and/or stasis on arterial side) - L-sided HF causes low arterial flow to kidneys, but less severe impairment - Damage d/t decreased and/or lack of nutrient supply to kidneys (less damage than lack of metabolite removal) |
|
|
What are some effects on the brain of right-sided heart failure?
|
- Venous congestion
- Hypoxic encephalopathy |
|
|
What are some effects on the lungs of right-sided heart failure?
|
- Pleural effusion
- Atelectasis (partial or complete collapse of the lung) |
|
|
What are some systemic effects of right-sided heart failure?
|
- Peripheral edema (at ankle / pedal and presacral)
- Eventual anasarca (extreme generalized edema) |

