![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
What is the resting membrane potential?
|
Negative intracellular electrical potential difference across the plasma membrane (relative to extracellular fluid) varies between -55 and -90 mV
|
|
|
What can preserve the resting membrane potential?
|
1) Conc. gradient (or activity) across the plasma membrane for specific permeable ions
2) Relative permeability of plasma membrane for these specific ions 3) Na+/K+ ATPase - electrogenic pump that uses ATP to extrude Na+ and accumulate K+ against their gradient |
|
|
What are the intra and extracellular ion concentrations for Na+?
|
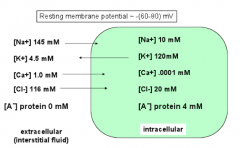
Out: ~145 mM
In: ~10 mM |
|
|
What are the intra and extracellular ion concentrations for K+?
|
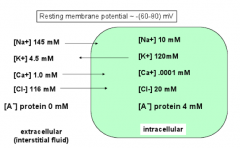
Out: ~4.5 mM
In: 120mM |
|
|
What are the intra and extracellular ion concentrations for Ca2+?
|
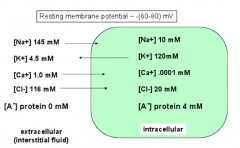
Out: ~1.0 mM
In: ~0.0001 mM |
|
|
What are the intra and extracellular ion concentrations for Cl-?
|
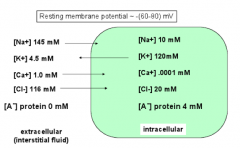
Out: ~116 mM
In: ~20 mM |
|
|
What do the terms reliability and adaptability refer to for the heart beat?
|
- Reliability - heart manages to beat constantly throughout entire life (hopefully!)
- Adaptability - heart can change rate due to activity/demand |
|
|
Which types of channels are used in a Cardiac AP?
|

- Rapid depolarizing Na+ channels (non-nodal)
- Depolarizing Ca2+ (nodal and myocyte contraction) - Repolarizing K+ (all myocytes) - Funny channels (Na+/K+) |
|
|
What are the phases of the ventricular/atrial myocyte and Purkinje fiber action potentials? What ions are important for each phase?
|
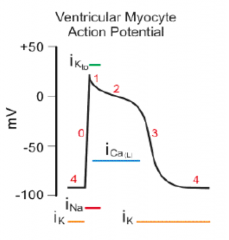
0) depolarization via fast Na+ channels
1) slight repolarization by K+ 2) plateau phase due to Ca2+ 3) repolarization by K+ 4) return to resting |
|
|
What are the phases of the SA and AV nodal cell action potentials? What ions are important for each phase?
|
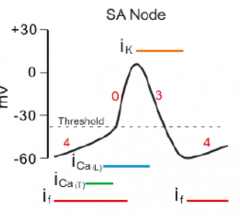
0) depolarization via slow Ca2+ channels
3) repolarization by K+ 4) hyperpolarization and return to resting potential by funny channels |
|
|
What is the resting membrane potential in atrial/ventricular myocytes and Purkinje fibers VS SA/AV nodal cells? What is the AP upstroke velocity?
|
- Atrial/Ventricular myocytes and Purkinje fibers: RMP = -80 to -90 mV, AP upstroke velocity >100-500V/sec
- SA/AV nodal cells: RMP = -40 to -70 mV (more depolarized); AP upstroke velocity 1-10V/sec |
|
|
What explains why the myocytes and purkinje fibers have faster upstrokes than the pacemaker (SA/AV nodal) cells?
|
Absence of fast Na+ channels in nodal cells and spontaneous opening of slow Ca2+ channels in pacemaker cells may explain why they have a slower time course and automaticity
|
|
|
What is the largest current in the heart?
|
Na+ current
|
|
|
How are fast Na+ channels activated/inactivated?
|
- At resting membrane potential channels closed
- Upon depolarization they rapidly activate - If Vm stays positive, channels start to inactivate - Some remain activated (or slowly inactivate) during the plateau phase |
|
|
What is the major current spreading through gap junctions? Why?
|
Na+ - this allows the depolarization to spread to neighboring cells
|
|
|
What kind of Ca2+ channels are important for SA and AV nodes?
|
L-type Ca2+ channels primaril
|
|
|
How are Ca2+ channels activated/inactivated?
|
- Slow depolarization for phase 0 (upstroke) of SA and AV nodes
- Slow spread of depolarization to neighboring cells which contributes to electrical delay between SA and AV nodes - Channels rapidly activate in atrial and ventricular cells, but slow inactivation (phase 2) which prolongs the plateau - Ca2+ entry triggers Ca2+ induced Ca2+ release to initiate contraction |
|
|
What are the types of K+ currents?
|
- Early outward K+ current (phase 1) - Ito
- Repolarizing K+ current (phase 3) - rapid (Ik and Ikr-) and slow (Iks-) - G-protein activated K+ current (SA and AV nodes) - GIRK K+ channels - K_ATP current - ATP sensitive K+ channels |
|
|
What is the function of the early outward K+ current? When?
|
- Phase 1
- Atrial and ventricular cells activated by depolarization and rapidly inactivates - Kv4.3 channel (Ito current) |
|
|
What is the function of the repolarizing K+ current? When?
|
- Phase 3
- Two currents underlie (Ik and Ikr-) the rapid component and one undrlies (Iks-) the slow component - Ik slowly activates, but does not inactivate |
|
|
What is the function of the G-protein activated K+ current? Where?
|
- Outward K+ current mediated by GIRK K+ channels and regulated by ACh
- Prominent in SA and AV nodal cells - Decreases pacemaker rate and slows conduction through AV Node |
|
|
What is the function of the K_ATP current?
|
ATP sensitive K+ channels play a role in electrically regulating contractile behaviors
|
|
|
Which kind of cells have I_f current? What kind of channel gives rise to this current?
|
- Pacemaker current found in SA, AV and Purkinje fibers
- Mediated by a non-selective cation channel = HCN (Hyperpolarization activated Cyclic Nucleotide-gated) - Conducts both K+ and Na+ |
|
|
How are Funny channels (giving rise to I_f current) regulated? Function?
|
- Not activated by depolarization
- Activated by hyperpolarization during phase 3 - Slow activation produces a slow inward depolarizing current and does not inactivate |
|
|
What characteristic divides cardiac cells into slow response cells and fast response cells?
|

Speed of AP upstroke
|
|
|
What determines cardiac function?
|
Electrical excitation triggers contraction and determines cardiac function
|
|
|
What is the primary intrinsic pacemaker?
|
SA node
|
|
|
What takes place at the SA node?
|
- Spontaneous depolarization --> AP
- Fastest intrinsic pacemaker activity, therefore they are dominant - Normal resting rates: sinus rhythm 60-100 bpm |
|
|
What takes place at the AV node? Location?
|
- Slowly conducting, introduces delay between atrial and ventricular activation
- Located above AV ring, secondary pacemaker |
|
|
What takes place at the His-Purkinje Fibers?
|
- Fibers originate at AV node w/ Bundle of His
- Split to form left bundle branch (conducts to LV) and right bundle branch (conducts to RV) - Left bundle branch further divides into left anterior fascicle and left posterior fascicle - Slow intrinsic pacemaker activity, but very rapid conduction |
|
|
What is the sequence of depolarization in cardiac tissue?
|
1. Depolarize atria (starting at SA node--> spread to AV node)
2. Depolarize septum from L-->R 3. Depolarize anteroseptal region of myocardium toward apex 4. Depolarize bulk of ventricular myocardium from endocardium to epicardium 5. Depolarize posterior portion of base of LV |
|
|
What are the conduction velocities through the SA/AV nodes, atria/bundle of His/ventricles, and Purkinje fibers?
|
- SA and AV nodes: ~0.05 m/sec
- Atria, Bundle of His, and Ventricles: ~0.08-1m/sec - Purkinje fibers: ~5 m/sec (100x faster than SA and AV nodes) |
|
|
How long does it take for the AP to spread through these sites?
- SA node - AV node - Bundle of His - Ant surface of RV - Apical surface - Posterior LV |
- SA node: 0 msec
- AV node: 66 msec - Bundle of His: 130 msec - Ant surface of RV: 190 msec - Apical surface: 220 msec - Posterior LV: 260 msec |
|
|
How does the amount of time for an AP to spread through the atria and ventricles compare? Why?
|
- Both take ~130 msec for the AP to spread, but disproportionate amount of tissue
- AV node delays propagation in atria - Purkinje fibers speed up propagation in ventricles |
|
|
Why is it important for the AV node to delay the propagation of the AP through the atria?
|
To allow contraction and complete emptying of the atria
|
|
|
Why is it important for the Purkinje fibers to speed up the propagation of the AP through the ventricles?
|
So that there is coordinated contraction of the entire ventricular mass
|
|
|
What is the normal PR interval, time between P wave (atrial depolarization) and QRS complex (ventricular depolarization)?
|
0.16 seconds (4 little squares) = Normal
>0.20 seconds (5 little squares) = Prolonged |
|
|
What are 3 mechanisms to slow SA firing rate and pacemaker activity (lowering HR)?
|
1. Decrease steepness of phase 4, thereby increasing time to reach threshold --> diastole is longer --> HR falls
2. Make maximum diastolic potential more negative, starting at a lower Em takes longer to reach threshold 3. Make threshold more positive, takes longer to reach threshold |
|
|
How can you decrease the ventricular rate in atrial flutter or atrial fibrillation without medication? Why is this important?
|
- Valsalva maneuver = forced expiration against closed airway to raise intrathoracic pressure --> opening airway allows pressure to drop leading to a transmural pressure increase in aorta, activating aortic baroreceptors reflex --> activation of vagus nerve (releases ACh)
- OR massage carotid sinus - The rapid atrial contraction leads to some transmission of APs to AV node that may make ventricles try to contract at a rate that leads to ineffective pumping |
|
|
What is the Valsalva Maneuver? Function?
|
- Forced expiration against closed airway to raise intrathoracic pressure
- Opening airway allows pressure to drop - Leads to a transmural pressure increase in aorta - Activates aortic baroreceptors reflex - Activation of vagus nerve (releases ACh) |
|
|
What is the action of ACh from the Vagus nerve on the heart?
|
- ACh decreases I_f in SA node, reducing the steepness of phase 4
- Opens GIRK channels, increasing K+ to make diastolic potential more negative - Reduces Ica2+, reducing steepness of phase 4 and moves threshold to a more positive value *All of these things act to SLOW conduction velocity* |
|
|
What is the action of Norepinephrine on the heart?
|
- From adrenal glands, it acts on beta-adrenergic receptors in SA and AV nodes
- Increases I_f --> increased steepness of phase 4 - Increase Ica2+ --> increased steepness of phase 4 and makes threshold more negative - No effect on maximum diastolic potential *All of these things act to QUICKEN conduction velocity* - On atrial and ventricular cells it has an inotropic effect (increases force of contraction) - Increases Ica2+ --> more release from SR --> more Ca2+ intracellularly to bind to troponin - Also enhanced SR pumping by stimulating SERCA Ca2+ pumps *All of these things act to INCREASE force of contraction* |
|
|
What is the effect of Temperature on the heart?
|
- Increasing body temperature increases SA node firing by increasing the slope of phase 4
- Approx. 10 bpm increase w/ 1 deg. C elevation in temp. - Cooling has the opposite effect (slows HR) |
|
|
What is the effect of Hyperkalemia on the heart?
|

- Increased extracellular K+ results in depolarization of the membrane potentials of cells
- Depolarization opens some voltage-gated Na+ channels, but also increases the inactivation at the same time - Since depolarization due to concentration change is slow, it never generates an action potential by itself instead, it results in accommodation - Above a certain level of K+ the depolarization inactivates Na+ channels, opens K+ channels, thus the cells become refractory - This leads to the impairment of neuromuscular, cardiac, and gastrointestinal organ systems - Of most concern is the impairment of cardiac conduction which can result in ventricular fibrillation or asystole |
|
|
How does Hyperkalemia affect the EKG?
|

- Reduction of P wave amplitude
- Widening of PR interval - Widening of QRS complex - Decreased force of contraction - Accelerates repolarization, shortening duration of AP - Shortens QT interval *Characteristic tall T wave peaks |
|
|
What is the effect of Hypokalemia on the heart?
|
- Hypokalemia causes hyperpolarization in the myocytes' resting membrane potential
- The more negative membrane potentials in the atrium may cause arrhythmias because of more complete recovery from sodium-channel inactivation, making the triggering of an action potential more likely. - In addition, the reduced extracellular K+ (paradoxically) inhibits the activity of the IKr potassium current[13] and delays ventricular repolarization - This delayed repolarization may promote re-entrant arrhythmias |
|
|
How does Hypokalemia affect the EKG?
|

- Slowing of repolarization, prolonging AP duration
- Flattening of T wave or inversion - Increased amplitude of P wave - Pronounced U wave - Prolongation of PR and QT intervals - Can cause AV block and ventricular fibrillation |
|
|
What is the effect of Hypercalcemia on the heart?
|
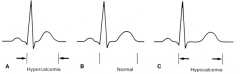
- Shortens the ventricular AP duration by shortening phase 2 of AP
- Shortens ST segment and QT interval |
|
|
What is the effect of Hypocalcemia on the heart?
|
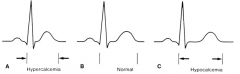
- Prolongs phase 2 of AP
- Prolongs ST segment and QT interval |
|
|
What is the effect of Tetrodotoxin (TTX) on the heart?
|
- Blocks voltage-dependent changes in Na+ permeability
- No effect on K+ permeability - Reduces phase 0 and slope of depolarization |
|
|
What is the effect of Tetraehylammonia (TEA) on the heart?
|
- Blocks voltage-dependent changes in K+ permeability
- No effect on Na+ permeability - Increases AP duration and extends refractory period (phase 3) |
|
|
What is Tetrodotoxin (TTX) used for?
|
- Slows rate and magnitude of depolarization in non-nodal cells
* Treats tachycardia * - Extends effective refractory period |
|
|
What is Tetraethylammonia (TEA) used for?
|
- Slows repolarization and extends effective refractory period
- Extends QT interval on ECG * Helpful in preventing tachyarrhythmias from re-entry mechanism * |
|
|
What is the molecular basis of cardiac arrhythmias?
|
- Reduced K+ conductance
- Decreased Na+ channel inactivation |
|
|
What are calcium channel blockers used for? Mechanism?
|
- Angina
- Hypertension - Arrhythmias - Mechanism: decrease entry of Ca2+ and delay depolarization of SA and AV nodes |
|
|
What are beta-blockers used for? Mechanism?
|
- Hypertension (inhibits renin)
- Angina and MI - Arrhythmias (slows rate of depol) Mechanism: prevents Ca2+ entry into cell, decreases HR, decreases conduction velocity, decreases strength of contraction |
|
|
What is the length of the absolute refractory period in ventricles and atria? Relative refractory period?
|
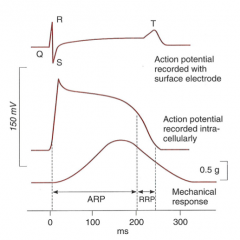
- Ventricles: 0.25-0.3 seconds
- Atria: 0.15 seconds - Relative refractory period: 0.05 seconds |
|
|
How low does the membrane potential need to get before a new AP can be initiated? Why?
|
< -50 mV
(because of inactivation of Na+ channels) |
|
|
What are the limb leads?
|
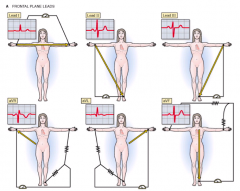
I, II, III, aVR, aVL, aVF
|
|
|
What are the precordial leads?
|
V1-V6 (placed on chest)
|
|
|
What do leads record?
|
- Changes in voltage differences between two electrodes over time
- Each record a different angle and plane of the heart |
|
|
What plane do the limb leads assess? What plane do the precordial leads assess?
|
- Limb leads: frontal plane
- Precordial leads: transverse plane |
|
|
What does lead I connect?
|

- Right arm ---> + Left arm
|
|
|
What does lead II connect?
|

- Right arm --> + Left leg
|
|
|
What does lead III connect?
|

- Left arm --> + Left leg
|
|
|
What does lead aVR connect? aVL? aVF?
|

aVR: - Mid heart --> + Right arm
aVL: - Mid heart --> +Left arm aVF: - Mid heart --> + Left foot |
|
|
How do you measure the heart rate from an EKG?
|
Rate (BPM) = 60 (sec/min) / R-R interval (sec/beat)
Measure number of large boxes forming RR interval: 300, 150, 100, 75, 60, 50 bpm corresponds to intervals of 1, 2, 3, 4, 5, and 6 large boxes |
|
|
What are the mechanisms of arrhythmias?
|
- Increased automaticity
- After-depolarizations - Re-entry |
|
|
What causes increased automaticity?
|
Decrease in time from depolarization from maximal diastolic potential to threshold potential via:
- Increased slope of phase 4 - Threshold potential is more negative - Maximum diastolic potential is more positive |
|
|
What is an "after-depolarization"? Cause?
|
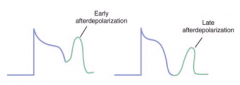
- Spontaneous AP during or immediately after phase 3 repolarization
- Caused by abnormal Ca2+ influx during or after phase 3 of ventricular AP leading to premature ventricular contractions and V. Tach. |
|
What conditions promote after-depolarizations?
|
Digoxin toxicity and conditions that prolong QT interval
|
|
|
What is "re-entry"? Cause?
|

- Re-excitation of a localized region of cardiac tissue by the same impulse, "circus movement"
- Occurs in presence of bifurcating conduction pathways, requiring: 1) unidirectional block 2) slow conduction through retrograde pathway, exceeding refractory period |
|
|
What can cause a unidirectional block and retrograde conduction? What is this called?
|

- Ischemic tissue w/ decremental conduction
- Em is reduced, fast Na+ channels are inactivated, and conduction velocity is slowed - Leads to unidirectional block - Can lead to re-entry in ventricular tissue |
|
|
What is the most common mechanism causing supraventricular tachycardia?
|

Re-entry in AV node
|
|
|
What are the pathways of the AV node?
|
- Fast pathway: long refractory period and rapid conduction velocity
- Slow pathway: short refractory period and slow conduction velocity |
|
|
What happens in re-entry of the AV node?
|

- Premature atrial contraction may penetrate slow pathway in antegrade direction
- May block antegrade in still-refractory fast pathway - Upon reaching turn-around point, if fast pathway has recovered from refractory period, impulse penetrates fast pathway in retrograde direction |

