![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
157 Cards in this Set
- Front
- Back
|
When do the right and left sides of the heart become completely separate?
|
Shortly after birth
|
|
|
What are the initial precursor cells for the cardiovascular system? Derived from?
|
Angioblasts or Hemangioblasts - from mesenchyme cells w/in extraembryonic and intraembryonic mesoderm
|
|
|
Where do angioblasts (precursor cells for CV system) appear first?
|
Walls of yolk sac - soon they appear in wall of other extraembryonic membranes and body stalk
|
|
|
Angioblast (precursor cells for CV system) specification and migration is influenced by signals from what?
|
Anterior Endoderm
|
|
|
What happens to angioblasts (precursor cells for CV system)?
|
- Aggregate into blood islands
- Differentiate into endothelial cells and hematopoietic stem cells - Adjacent blood islands merge to form vascular plexus (network of primary blood vessels / endothelial tissues) |
|
|
What is the structure of the endothelial cells that are derived from angioblasts? What happens to them?
|
- Flat epithelial cells
- Form internal lining layer of all blood vessels and heart |
|
|
What is the term for blood cell formation? Where does it occur / timeframe?
|
- Hematopoiesis
- Begins in blood islands - During development: yolk sac (months 1-2), spleen/liver (months 2-7), and bone marrow (month 4 - adult) |
|
|
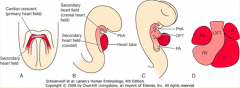
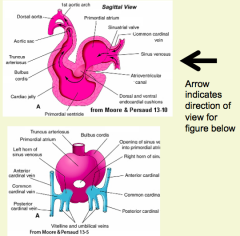
What is the heart derived from?
|
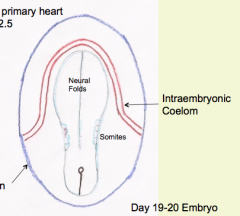
- U-shaped region of Splanchnic Mesoderm known as Cardiogenic Crescent aka Primary Heart Field
- Found in medial wall of entraembryonic coelom at its cranial end |
|
|
What portion of the intra-embryonic coelom does the cardiogenic crescent / primary heart field (future heart) get derived from?
|
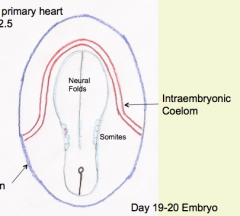
Medial wall of intra-embryonic coelom at cranial end = Primitive Pericardial Coelom
|
|
|
What happens to the cells in the Cardiogenic Crescent?
|

- Migrate into space between foregut endoderm and cardiogenic crescent - forms Endothelial Plexus
- Endothelial Tube will form called Endocardium, which becomes the epithelial lining inside the heart - Mesoderm will mold around endocardium to form the Myocardium (future muscle layer of heart) * Mediated by signals from Anterior Endoderm * |
|
|
What are the effects of the Cranial-Caudal folding of the embryo on the cardiac primordium?
|

Leads to a ventrally located heart (before folding the heart tube was cranial to the primordial brain and the septum transversum (ST) was cranial to heart primordium)
|
|
|
What is cranial to the heart tube before cranial-caudal folding? What is caudal to heart tube? Location after folding?
|

- Cranial: Septum Transversum (ST) - future diaphragm - after folding it is caudal to heart tube
- Caudal: Primordial Brain - future brain - after folding it is cranial to heart tube |
|
|
What is the Septum Transversum? What does it become?
|

- Accumulation of mesoderm derived mesenchyme adjacent to transverse portion of U-shaped intraembryonic coelom
- Once folding is complete it lies caudal to forming heart - Becomes part of diaphragm |
|
|
What are the effects of the Lateral / Transverse folding of the embryo on the cardiac primordium?
|
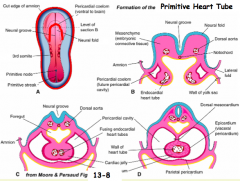
- Limbs of cardiac crescent are brought together
- Forms initial segments of primitive heart tube in midline |
|
|
After lateral folding of the embryo, what is the primitive heart tube suspended from?
|
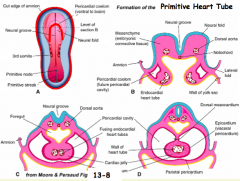
Dorsal Mesocordium --> eventually disappears and leaves a communication between the sides of the pericardial cavity known as the Transverse Pericardial Sinus
|
|
|
What happens to the Intraembryonic Coelom?
|
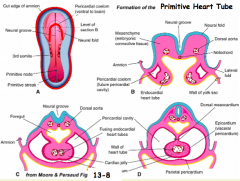
Becomes known as the Pericardial Cavity
|
|
|
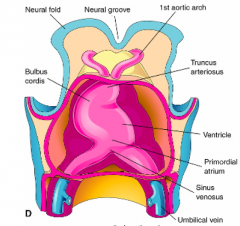
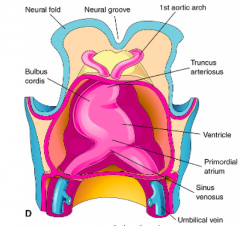
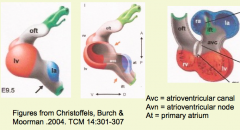
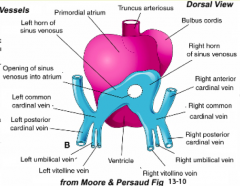
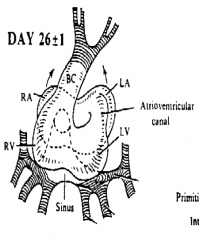
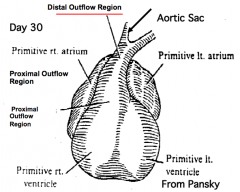
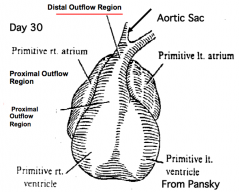
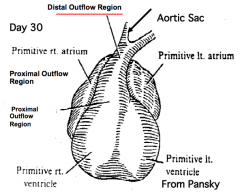
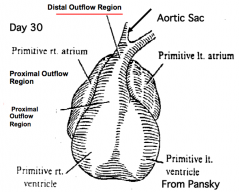
What is derived from the primitive heart tube?
|
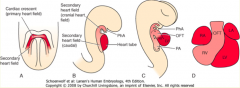
- Mostly primitive left ventricle
- Small portion of primitive right ventricle - Most of Primordial Atrium - Atrioventricular (AV) Canal |
|
|
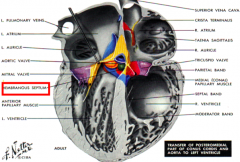
What is derived from the Aortic Arch? Where is it located?
|
- Pharyngeal arch arteries
- Adjacent to cranial or outflow end of primitive heart tube |
|
|
What happens to the Primitive Heart Tube?
|
- Elongation of heart tube occurs as additional segments are formed from cells contributed by primary and secondary heart fields
- As it lengthens, the outflow region will elongate and be subdivided into Proximal and Distal Segments |
|
|
What is the secondary heart field important for?
|
- Source of cardiac progenitor cells (dorsal/medial to primary heart field)
- Important for contributing to elongation of heart tube |
|
|
What is derived from the Secondary Heart Field?
|
- Most of primitive R ventricle
- Outflow region (tract) - Sinus Venosus |
|
|
How do the segments of the primitive heart tube compare to the chambers of adult heart?
|
They are NOT equivalent (lots of additions and modifications to primitive chambers)
|
|
|
What is the master gene for the Secondary Heart Field?
|
Isl-2 (allows for elongation of primitive heart tube)
|
|
|
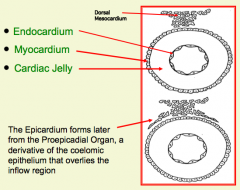
What are the tissues of the primitive heart tube?
|
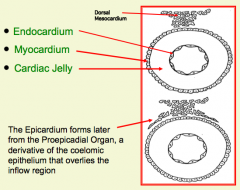
1. Cardiac Endothelium (Endocardium)
2. Myocardium 3. Cardiac Jelly 4. Epicardium |
|
|
What organization is helpful for thinking about the primitive heart tube?
|
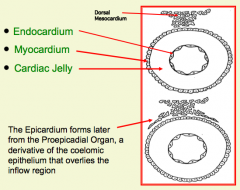
Tube within a Tube
|
|
|
What tissue from the primitive heart tube lines the lumen of the heart?
|
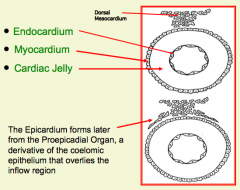
Cardiac Endothelium (Endocardium)
|
|
|
What tissue from the primitive heart tube forms the outer epithelial tube? What happens to this structure?
|
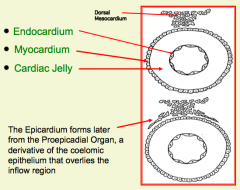
Myocardium - this layer eventually becomes bistratified, and its cells will differentiate into cardiac myoblasts that form from the muscle of the heart wall
|
|
|
What tissue from the primitive heart tube forms between the endocardium and myocardium? What is this?
|
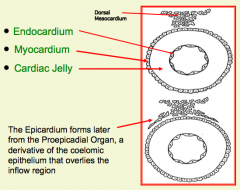
Cardiac Jelly - accumulation of ECM
|
|
|
Swellings in the cardiac jelly occur where? What do they look like?
|
- In AV canal and outflow regions
- Look like primitive valves - In AV canal they are called Endocardial Cushions - In outflow region they are called Bulbar or Conotruncal Ridges |
|
|
What tissue from the primitive heart tube forms an epithelial layer over the external surface of the myocardium? What is it derived from?
|
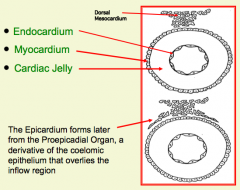
Epicardium - derived from Proepicardial Organ (cluster of coelomic epithelial cells adjacent to the sinus venosus)
|
|
|
What is a derivative of the Epicardium?
|
Epithelium and underlying fibrous CT of the visceral pericardium; also contribute to the formation of the coronary vessels
|
|
|
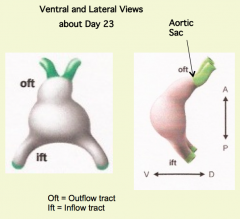
Where does the venous inflow enter the primitive heart tube?
|
Sinus Venosus Region
|
|
|
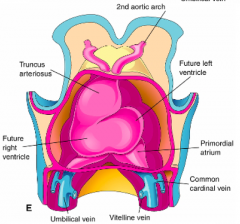
What venous channels enter the Sinus Venosus Region ("Venous Inflow") of the Primitive Heart Tube?
|
- Umbilical Veins (contain oxygen-rich placental blood)
- Vitelline Veins (contain oxygen-poor blood from gut) - Common Cardinal Veins (contain oxygen-poor blood from head and trunk via anterior and posterior cardinal veins) |
|
|
Where does the outflow leave the primitive heart tube?
|
Primitive Right Ventricle
|
|
|
What channels leave the Primitive Right Ventricle ("Venous Outflow") of the Primitive Heart Tube?
|
Aortic Sac (continuous with right ventricle)
- Pharyngeal Arch Arteries / Aortic Arches (originate from aortic sac) |
|
|
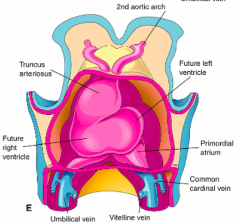
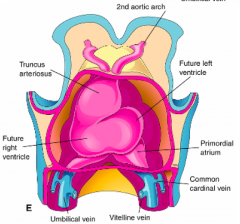
What happens almost immediately after the initial heart tube segment appears?
|
- Elongating heart tube begins to bend to the right = Cardiac Looping
- Driven by addition of cells from the primary and secondary heart fields at cranial and caudal ends |
|
|
Which direction does the heart loop to?
|

Almost always to the RIGHT
|
|
|
What is the location of the apex or bend of the heart tube loop?
|

Between the primitive left and right ventricles
|
|
|
What is in the cranial limb of the loop (looping heart tube)?
|
- Initially: Primitive right ventricle
- Later: Outflow region |
|
|
What is in the caudal limb of the loop (looping heart tube)?
|
- Initially: Primitive left ventricle
- Later: AV canal, primordial atrium, and sinus venosus are added to caudal limb of loop |
|
|
What happens during the early phase of cardiac looping?
|
- Proper anatomical relationships between heart segments are established
- Venous inflow and arterial outflow regions are brought together - Outflow region forms and elongates into proximal and distal regions - Distal outflow region continuous w/ aortic sac |
|
|
What does the elongating outflow region become subdivided into during the early phase of cardiac looping?
|
- Proximal (conus arteriosus)
- Distal (truncus arteriosus) |
|
|
What happens during the late phase of cardiac looping?
|
- Both limbs of loop (cranial and caudal) contact each other along bulboventricular groove (at level of AV canal)
- Occurs via bending at inner curvature - Proximal portion of outflow region is "wedged" (shoved to left) into AV canal |
|
|
What is the hinge for contact between the cranial and caudal limbs of the heart loop?
|
Inner curvature located along apex of bulboventricular groove
|
|
|
What is the proper cardiac looping necessary for?
|
- Alignment of all cardiac segments and for forming septa
- Failure leads to retention of embryonic pattern of blood flow through heart |
|
|
When does the heart begin to beat?
|
21-22 days
|
|
|
What is the initial blood flow pattern through the primitive heart?
|
Sloshing back and forth movement
|
|
|
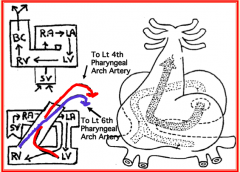
What happens later to the blood flow pattern through the primitive heart?
|
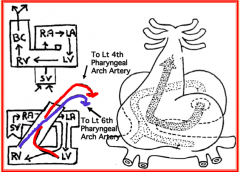
- Becomes unidirectional from inflow to outflow regions
- L and R blood streams enter heart and spiral around each other - 2 streams are physically separated w/o a morphological separation |
|
|
Where does the stream from the left ventricle exit the primitive heart?
|
Left pharyngeal arch artery 4 (will become part of the aorta)
|
|
|
Where does the stream from the right ventricle exit the primitive heart?
|
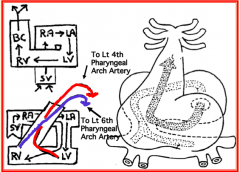
Left pharyngeal arch artery 6 (will become the ductus arteriosus)
|
|
|
What tissues are used for partitioning the primitive heart?
|
- Cardiac Muscle
- Cardiac Mesenchyme (Endocardial Cushion Tissue) - Extracardiac Mesenchyme (mesoderm origin) - Neural Crest |
|
|
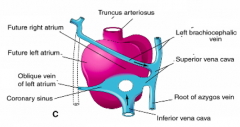
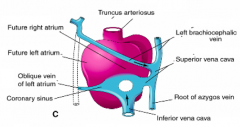
What does the definitive right atrium form from?
|
- Primitive R atrium
- Parts of Sinus Venosus (SV) |
|
|
What do the horns of the Sinus Venosus open into?
|
- Opens into its own side of the primordial or common atrium (R horn --> R side; L horn --> L side)
- Soon a common SV opens into the primordial atrium at the Sinoatrial opening - Sinoatrial opening flanked by R and L valves |
|
|
What veins atrophy after the horns of the Sinus Venosus connect to the Primitive Atrium?
|
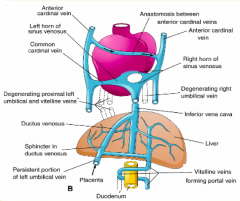
- L (proximal/cranial) and R umbilical veins
- L vitelline vein |
|
|
What forms the terminal segment of the inferior vena cava
|
R vitelline vein
|
|
|
What is the fate of the Vitelline Veins?
|
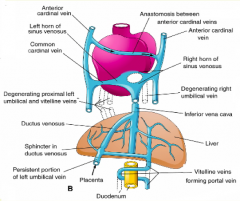
- L - atrophies
- R - cranial portion forms terminal segment of inferior vena cava |
|
|
What happens to the Sinus Venosus?
|
- L SV becomes a tributary to the R SV
- Sinoatrial opening then appears to be shifted to R so it can open exclusively into R side of atrium |
|
|
What flanks the SA opening?
|
- Flanked by R and L SV valves
- Valves fuse together cranially |
|
|
What happens to the R & L SV valves that flank the sinoatrial opening?
|
- Fuse together cranially
- L valve atrophies - R valve remains as two folds, the valves of the inferior vena cava and the coronary sinus |
|
|
What is the fate of the cardinal veins?
|
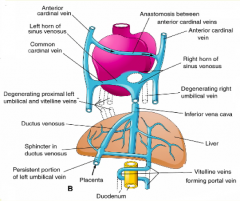
- Anastomosis forms between superior cardinal veins
- Most of L cardinal venous channels atrophy |
|
|
What changes lead to all systemic venous return entering right side of heart?
|
- L (proximal) and R Umbilical and L Vitelline vein atrophy
- L SV becomes tributary to R SV - Anastomosis forms between L and R Anterior Cardinal veins |
|
|
What structures are derived from the L Sinus Venosus?
|
Coronary Sinus
|
|
|
What structures are derived from the R Sinus Valve?
|
- Crista Terminalis
- Valve of IVC - Valve of Coronary Sinus |
|
|
What structures are derived from the R Sinus Venosus?
|
After it is absorbed into the wall of the R atrium it becomes the smooth area of Right Atrium
|
|
|
What structures are derived from the primitive R atrium?
|
- Trabeculated / Rough portion of R atrium - forms Pectinate Muscles
- Auricle |
|
|
What structures are derived from the R Vitelline Vein?
|
IVC (terminal segment)
|
|
|
What structures are derived from the R common cardinal vein?
|
SVC
|
|
|
What are the components of the Coronary Sinus derived from?
|
- L Sinus Venosus
- Valve: R Sinus Valve |
|
|
What is the Crista Terminalis derived from?
|
R Sinus Valve
|
|
|
What are the components of the IVC derived from?
|
- Terminal segment: R Vitelline Vein
- Valve: R Sinus Valve |
|
|
What are the components of the R Aterium derived from?
|
- Smooth area: absorbed R Sinus Venosus
- Trabeculated area + auricle: Primitive Atrium |
|
|
What are the components of the SVC derived from?
|
R Common Cardinal Vein
|
|
|
What are the components of the L Atrium derived from?
|

- Smooth part: absorbed Pulmonary Veins
- Trabeculated part + Auricle: Primitive Atrium |
|
|
What vein / how many grow out of the L atrium? What is the fate?
|
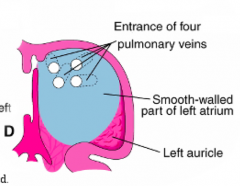
- 1 Pulmonary Vein
- Connects w/ pulmonary vascular plexus associated w/ branching lung buds - Initial pulmonary veins are absorbed into primordial L atrium to become smooth part of definitive L atrium - Eventually 4 pulmonary veins form |
|
|
What structure initially forms between the L side of primordial atrium and the primitive L ventricle? Implications?
|
Common AV canal - as a result there is no atrial inflow to primitive R ventricle (need to establish a connection between R side of common atrium and primitive R Ventricle)
|
|
|
How can you form a connection between the R side of the common atrium and the R ventricle?
|

- Not by splitting existing common AV canal into R and L sides (because these would both open into L ventricle)
- Must be a repositioning of the AV canal |
|
|
Why do you need to realign the common AV canal?
|

To create a connection between the R side of the common atrium and the R ventricle
|
|
|
How do you realign the common AV canal?
|
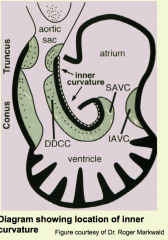
- Opening must be created from R side of common atrium into primitive R ventricle
- Occurs along inner curvature of heart - Encocardial cushion tissue replaced w/ cardiac muscle ("myocardialization") - Heart wall of inner curvature thins allowing AV canal to shift to R during late phase cardiac looping - Outflow region shifts to L and wedged into AV canal |
|
|
What does the division of the common AV canal depend on?
|
- Formation of cardiac mesenchyme (aka endocardial cushion tissue) which moves into cardiac jelly
- Epithelium to Mesenchyme Transformation |
|
|
Where does the cardiac mesenchyme form?
|
Forms in 2 segments of primitive heart tube: AV Canal and Outflow Region
|
|
|
What are the characteristics of the cardiac jelly in the AV canal and the outflow region of the primitive heart tube?
|
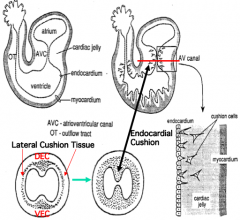
- Enlarged, forming pads and ridges on dorsal and ventral walls of AV canal
- Pads are populated by transformed endocardial cells, now known as cardiac mesenchyme cells or endocardial cushion tissue |
|
|
What is the name of the expansions of cardiac jelly in the outflow tract?
|
Bulbar ridges (also populated w/ cardiac mesenchyme cells)
|
|
|
What happens to the dorsal and ventral endocardial cushions?
|

- They fuse to form a centrally positioned mass of cushion tissue = Septum Intermedium
- Results in separate right and left AV canals connected to appropriate ventricle |
|
|
What is the function of the Septum Intermedium?
|

- Barrier within AV canal that allows separate canals to connect to appropriate ventricles
- Acts as a guide and glue for positioning and attachment of the forming septa during cardiac partitioning |
|
|
What happens to the distance between the septum intermedium and the superior edge of the muscular interventricular septum during heart growth?
|
It remains constant during the partitioning process
|
|
|
What is the fate of the cardiac mesenchyme in the mature heart?
|
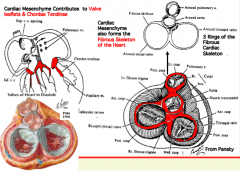
- Valve leaflets of Mitral, Tricuspid, Aortic, and Pulmonary Valves
- Chordae Tendinae - Cardiac Skeleton - All structures are made out of fibrous CT |
|
|
What separates the primitive ventricles? What are the components of this structure?
|
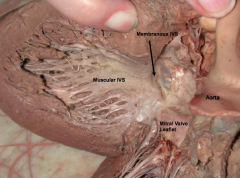
- Interventricular Septum (IVS)
- Made of muscular and membranous (fibrous) portions - Muscular portion makes up majority of septum (made of cardiac muscle) and forms trabeculae - Membranous portion is small (made of fibrous CT) and forms from cushion tissue of bulbar ridges (outflow tract) and septum intermedium (AV canal) |
|
|
What structure forms the opening into the aorta / aortic vestibule?
|
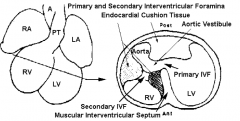
Primary Interventricular Foramen (IVF)
|
|
|
What is the fate of the Primary Interventricular Foramen (IVF)?
|
- Never closed by a septum
- Becomes opening into a tunnel-like corridor known as the Aortic Vestibule - Forms inlet from forming left ventricle to forming aorta |
|
|
What structure forms between the wall of the aortic vestibule and the forming right ventricle?
|
Secondary Interventricular Foramen (IVF)
|
|
|
What is the fate of the Secondary Interventricular Foramen (IVF)?
|
- Located between wall of aortic vestibule and forming right ventricle
- Closed by the membranous portion of the interventricular septum - Visible in cross-sections of forming heart at level of forming ventricles, but not coronal or sagittal sections |
|
|
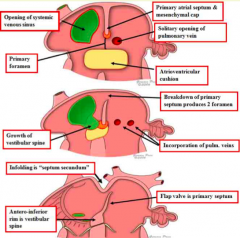
What are the requirements of the interatrial septum?
|

- Must separate the two atria
- Must allow for right-to-left shunting of blood - Must provide for only one-way shunting |
|
|
What is the traditional view on how the interatrial septa forms?
|

- Two septa (primum and secondum) form sequentially each having a foramen
- The foramina (primum and secondum) are in separate septum and offset from each other |
|
|
What is the first step of forming the interatrial septa in the traditional view?
|

Formation of Primary Atrial Septum / Septum Primum:
- Muscular outgrowth extends inferiorly from the roof of the common atrium towards the fusing AV endocardial cushions - Inferior edge is coated w/ mesenchyme called "mesenchyme cap |
|
|
What is the opening between the inferior edge of the Primary Atrial Septum (PAS) and the superior surface of the fusing cushions?
|

Primary Atrial Foramen or Ostium Primum
|
|
|
What happens in the second step of forming the interatrial septa in the traditional view, after formation of the septum primum?
|
Formation of Dorsal Mesocardial Projection or Vestibular Spine:
- As PAS expands, a projection of extracardiac mesenchyme extends inward from the dorsal wall of the common atrium just medial to the inferior edge of the sinoatrial opening - This mesenchyme (believed to be from dorsal mesocardium) is called Dorsal Mesocardial Projection or Vestibular Spine |
|
|
What happens in the third step of forming the interatrial septa in the traditional view, after formation of the Dorsal Mesocardial Projection / Vestibular Spine?
|
Closure of Primary Atrial Foramen:
- Dorsal mesocardial projection / vestibular spine merges w/ mesenchyme cap of the primary atrial septum and the cushion tissue forming the septum intermedium |
|
|
What happens in the fourth step of forming the interatrial septa in the traditional view, after closure of the primary atrial foramen?
|
Formation of Secondary Atrial Foramen / Ostium Secondum:
- Primary Atrial Septum detaches from the roof of the atrium, creating the secondary atrial foramen - Traditional view has the ostium secondum in the primary atrial septum |
|
|
What happens in the fifth step of forming the interatrial septa in the traditional view, after formation of the secondary atrial foramen?
|
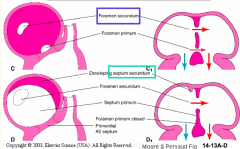
Formation of the Superior Interatrial Fold:
- Forms in the roof of the common atrium to the right of the primary atrial septum - Marks boundary between the right and left atria |
|
|
What structure marks the boundary between the right and left atria, in the traditional view?
|

Superior Interatrial Fold: interatrial muscular ridge
(ridge where septum secundum grows) |
|
|
What happens in the sixth step of forming the interatrial septa in the traditional view, after formation of the superior interatrial fold?
|
Formation of the Septum Secundum and Foramen Ovale:
- Ridge (superior interatrial fold) grows downward forming the septum secondum - Septum secundum is incomplete at its inferior border defining an opening called the Oval Foramen |
|
|
What are the steps of forming the septation of the atrium?
|
1. Formation of Primary Atrial Septum / Septum Primum
2. Formation of Dorsal Mesocardial Projection or Vestibular Spine 3. Closure of Primary Atrial Foramen 4. Formation of Secondary Atrial Foramen / Ostium Secondum 5. Formation of the Superior Interatrial Fold 6. Formation of the Septum Secundum and Foramen Ovale |
|
|
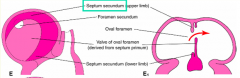
What is different about the alternative view of atrial septation?
|
- Primary atrial septum forms a flapper valve (controls blood flow across interatrial septum from R to L)
- No downward growth of a septum secondum (NO septum secondum) - Ovale foramen bounded by two folds (superior interatrial fold cranially and anterio-inferior rim caudally) - Anterio-inferior rim is the area where the mesenchyme cap of PAS merged w/ septum intermedium and vestibular spine |
|
|
What is the function of the Interatrial Septum?
|
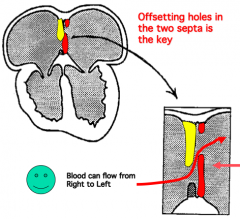
Acts as a unidirectional flapper valve that only allows blood flow from right to left between the atria; when the left atrium contracts or fills, the septum primum is pushed against the septum secundum preventing left-to-right blood flow
|
|
|
What are the portions of the definitive ventricle?
|
- Each has an Inflow Portion and an Outflow Portion
- Outflow portion of R ventricle is connected to Pulmonary Trunk - Outflow portion of L ventricle is connected to Aorta - Each outflow portion contains a semilunar valve |
|
What is the adult derivative of the primitive right and left ventricles?
|
Inflow portion of right and left ventricles (i.e., trabeculated portions)
|
|
What is the adult derivative of the proximal outflow region (conus arteriosus)?
|
Outflow portion of R and L ventricles (i.e., smooth portions)
|
|
What is the adult derivative of the distal outflow region (truncus arteriosus)?
|
Pulmonary and Aortic Valves and part of the roots of aorta and pulmonary trunk
|
|
What is the adult derivative of the aortic sac?
|
Parts of Pulmonary and Aortic Root
|
|
|
What forms the walls of the proximal and distal outflow regions?
|
Cardiac muscle - each have a pair of ridges made of endocardial cushion tissue = BULBAR RIDGES
|
|
|
Where are the Bulbar Ridges? What happens to them?
|
- Endocardial cushion tissue
- Extend into lumen of proximal and distal outflow regions - Proximal: run along dorsal and ventral walls - Distal: run along superior and inferior walls - Adjacent ridges in proximal and distal outflow tract fuse w/ each other - Opposing ridges within each portion of outflow tract fuse w/ each other |
|
|
What forms the Conotruncal Septum?
|
- Fusion of bulbar ridges in proximal and distal outflow regions
- Adjacent ridges in proximal and distal outflow tract fuse w/ each other - Opposing ridges within each portion of outflow tract fuse w/ each other |
|
|
What is the function of the Conotruncal Septum? Organization?
|
Separates the outflow region into right and left channels; spiral septum because during looping, outflow region twists about 90 degrees
|
|
|
What does the cushion tissue in the distal outflow region contribute to the formation of?
|
Aortic and Pulmonary Valves
|
|
|
What is the function of the Neural Crest Cells in the distal outflow region?
|
- Migrate into aortic sac and distal outflow region
- Contribute to formation of valves and septum |
|
|
What direction do the proximal outflow region and the AV canal shift?
|
- Proximal outflow region shifts LEFT during late phase of looping
- AV Canal shifts RIGHT |
|
|
What kind of tissues are in the aortic sac before it divides?
|
- Wall of aortic sac is smooth muscle
- Mass of mesenchyme (Arterial Spine) extends from dorsal wall of aortic sac into lumen <-- derived from Neural Crest |
|
|
What structure divides the Distal Outflow Region?
|
Conotruncal Septum
|
|
|
What structure divides the Aortic Sac? What are the new compartments?
|
Aorticopulmonary Septum:
- Divides it into ventral and dorsal compartments - Ventral: root of pulmonary trunk - Dorsal: root of the aorta |
|
|
What happens to the Aorticopulmonary Septum once formed?
|
Fuses w/ the superior edge of the conotruncal septum that divides the distal outflow region
|
|
|
What forms the membranous interventricular septum (IVS)?
|
Fusion of two components derived from Endocardial Cushion Tissue:
- Inferior edge of Conotruncal Septum (dividing proximal outflow region) - Part of Ventral Endocardial Cushion of Septum Intermedium - Cushion tissue is transformed into Fibrous CT - Membranous portion of IVS fuses w/ superior edge of Muscular IVS - This fusion of membranous and muscular portions closes the SECONDARY Interventricular Foramen |
|
|
What closes the Secondary Interventricular Foramen?
|
Fusion of Membranous Interventricular Septum with Muscular Interventricular Septum
|
|
|
What closes the Primary Interventricular Foramen?
|
Trick question, it always remains open because it is the opening into the aorta
|
|
|
What is the inlet portion of the definitive R ventricle derived from?
|
Primitive R Ventricle
|
|
|
What is the outlet portion of the definitive R ventricle (infundibulum) derived from?
|
Proximal Outflow Region
|
|
|
What is the inlet portion of the definitive L ventricle derived from?
|
Primitive L Ventricle
|
|
|
What is the outlet portion of the definitive L ventricle (aortic vestibule) derived from?
|
Proximal Outflow Region
|
|
|
Before / After partitioning, where did blood enter the heart?
|
Before:
- Entered R & L side of common atrium - No pulmonary circulation established After: - Systemic venous return shifted to R side of atrium - Pulmonary return established on L side of atrium |
|
|
Before / After partitioning, how were the atria organized?
|
Before:
- Common atrium After: - Common atrium is subdivied |
|
|
Before / After partitioning, how were the atria and ventricles communicating?
|
Before:
- No communication between R side of common atrium and R ventricle - Common AV canal joining common atrium and L ventricle After: - Communication between R atrium and R ventricle - Common AV canal is subdivided |
|
|
Before / After partitioning, how were the ventricles organized?
|
Before:
- Opening between R & L ventricles After: - Separate R & L ventricles |
|
|
Before / After partitioning, how was the outflow region organized?
|
Before:
- Common outflow region After: - Subdivide the outflow region |
|
|
What are the characteristics of Fetal Circulation?
|
- Blood is shunted around liver from R-->L in heart
- Pulmonary circulation of fetus is inactive - Pressure in R side of heart is greater than in L side - Blood returns to placenta through Umbilical Arteries |
|
|
How does O2 rich blood (80% saturation) get from the placenta to the fetus?
|
Via the Umbilical Veins
|
|
|
How is the blood in the fetus shunted around the liver?
|
- Via the Ductus Venosus
- Connects Umbilical Vein w/ Inferior Vena Cava - Valve in D.V. controls amount of blood flowing through shunt and amount going to liver |
|
|
Where does blood in the fetus go after the R. atrium?
|
Shunted across Foramen Ovale to L atrium (avoids being pumped to lungs, although some still goes to R ventricle)
|
|
|
Where does blood in the fetus go after the R. ventricle?
|
Shunted into Aorta via Ductus Arteriosus (connects pulmonary trunk and aorta) - avoids blood being pumped to lungs
|
|
|
How large is the Ductus Arteriosus in the fetus? What does it connect?
|
- As large as the Pulmonary Trunk
- Connects the Pulmonary Trunk and the Aorta |
|
|
Why is the pulmonary circulation in the fetus inactive?
|
Resistance int he pulmonary blood vessels is very high because the lungs are full of fluid, as a result there is minimal blood flow here
|
|
|
Why is the pressure int he R side of the heart greater than the L side in the fetus?
|
Partly d/t the high pulmonary vascular resistance
|
|
|
What is the saturation of blood leaving the placenta? Returning to the placenta?
|
- Umbilical Veins (leaving placenta): 80%
- Umbilical Arteries (returning to placenta): 58% |
|
|
What circulation changes occur in a newborn?
|
- Shunts close
- Pulmonary vascular resistance falls - Pressure changes occur in heart - Umbilical arteries and veins obliterated |
|
|
What shunts close in the newborn? What happens to them?
|
- Ductus Venosus - forms Ligamentum Venosum on inferior side of liver
- Foramen Ovale - closes when two components of interatrial septum fuse, leaves Fossa Ovalis (depression in septum) - Ductus Arteriosus - forms Ligamentum Arteriosum that tracks between pulmonary trunk and aorta |
|
|
What happens to the pulmonary vascular resistance in a newborn?
|
Drops as fluid in lung is replaced with air; allows pulmonary circulation to fill w/ blood
|
|
|
What happens to the pressure within the heart in a newborn?
|
- Reduced pulmonary vascular resistance and filling of pulmonary circulation causes pressure to decrease on R side of heart
- Increased pressure on L side of heart |
|
|
What happens to the umbilical veins and arteries in a newborn?
|
- Inferior portion of umbilical vein becomes obliterated --> Ligamentum Teres of liver
- Distal portion of umbilical arteries becomes obliterated --> Medial Umbilical Ligaments (inner surface of ventral wall of abdomen) |
|
|
Do physiological changes or anatomical changes occur more rapidly in the transition from fetus to newborn circulation?
|
Physiological changes happen more rapidly than anatomical changes
|
|
|
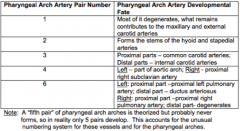
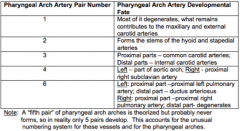
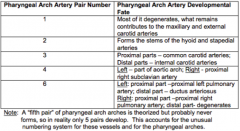
Describe the general features of pharyngeal arch artery development?
|
- Series of 5 paired vessels = Pharyngeal Arch Arteries supply pharyngeal arches
- Vessels originate in Aortic Sac (outflow region) - Empty into Dorsal Aortas - Cranial pairs form earliest and are remodeling by the time the caudal pairs have formed - Initially two dorsal aortas form and run length of embryo, eventually they form a single aorta caudal to the heart and cranially the R regresses while L becomes definitive aorta |
|
|
What is derived from the Pharyngeal Arch Artery Pair 1?
|
- Mostly degenerates
- What remains contributes to MAXILLARY and EXTERNAL CAROTID arteries |
|
|
What is derived from the Pharyngeal Arch Artery Pair 2?
|
Forms stems of HYOID and STAPEDIAL arteries
|
|
|
What is derived from the Pharyngeal Arch Artery Pair 3?
|
- Proximal parts: COMMON CAROTID arteries
- Distal parts: INTERNAL CAROTID arteries |
|
|
What is derived from the Pharyngeal Arch Artery Pair 4?
|
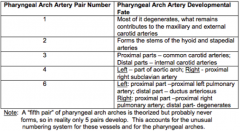
- Left: part of AORTIC ARCH
- Right: proximal R SUBCLAVIAN artery |
|
|
What is derived from the Pharyngeal Arch Artery Pair 6?
|
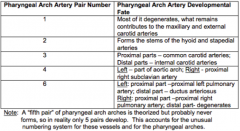
- Left proximal: proximal L PULMONARY artery
- Left distal: DUCTUS ARTERIOSUS - Right proximal: proximal R PULMONARY artery - Right distal: degenerates |
|
|
What are the major anomalies involving the great arteries?
|
- Coarctation of the aorta
- Double pharyngeal arch artery - Right arch of the aorta - Anomalous R subclavian artery |
|
|
What are the outcomes of a double pharyngeal arch artery anomaly? Cause?
|
- Presence of a vascular ring surrounding the trachea and esophagus
- Cause: failure of distal portion of R dorsal aorta to atrophy |
|
|
What are the outcomes of a right arch of the aorta anomaly?
|
- Persistence of R dorsal aorta accompanied by atrophy of L dorsal aorta (usually L becomes definitive aorta)
- 1st possibility: R arch is ventral and lateral to trachea and esophagus - no retro-esophageal component - 2nd possibility: R arch passes behind trachea and esophagus = retro-esophageal component --> ligamentum arterosum completes a ring that could constrict esophagus and trachea |
|
|
What are the outcomes of an anomalous right subclavian artery?
|
- Instead of arising from Brachiocephalic A, R subclavian A originates from distal part of Aortic Arch
- Passes posterior to trachea and esophagus (retro-esophageal) to gain access to right upper limb |

