![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back
|
Systemic Lupus Erythematosus (SLE) - general characteristics |
1. An autoimmune disorder leading to inflammation and tissue damage involving multiple organ systems
2. not completely understood. SLE is an idiopathic chronic inflammatory disease with genetic, environmental, and hormonal factors. Pathogenesis involves autoantibody production, deposition of immune complexes, complement activation, and accompanying tissue destruction/vasculitis 3. Types - a. spontaneous SLE, b. drug-induced SLE, c. discoid lupus (skin lesions without systemic disease) d. ANA-negative Lupus- associated findings include (arthritis, Raynaud's, subacute cutaneous lupus, serology- Ro (anti-SS-A) antibody positive, ANA negative + risk of neonatal lupus in infants of affected women |
|
|
Clinical features of SLE (Lupus)
|

1. Constitutional symptoms- fatigue (often the sign of an impending exacerbation and a prominent finding in most patients), malaise, fever and weight loss
2. Cutaneous- butterfly rash (erythematois rash over the cheeks and the bridge of the nose, found in 1/3 of patients), photosensitivity, discoid lesions (erythematous raised patches with keratotic scaling), oral and nasopharyngeal ulcers, alopecia, Raynaud's phenomenon 3. musculoskeletal - joint pain (may be the first symptom - found in 90% of patients), arthritis (inflammatory and symmetric, not erosive as in RA), arthralgias, myalgia with or without myositis 4. cardiac - pericarditis, endocarditis (libman-sacks endocarditis = serious complication), myocarditis 5. pulmonary- pleuritis (most common pulmonary finding), pleural effusion, pneumonitis (may lead to fibrosis), pulmonary HTN 6. hematologic - hemolytic anemia with reticulocytosis or chronic disease, leukopenia, lymphopenia, and thrombocytopenia 7. renal- proteinuria > 0.5 mg/day (may have nephrotic syndrome), cellular casts, glomerulopnephritis (may have hematuria), azotemia, pyuria, uremia, HTN 8. Immunologic- impaired immune response due to many factors, including autoantibodies to lymphocytes, abnormal T cell function and immunosupressive medications 9. GI- n/v, dyspepsia, dysphagia, peptic ulcer disease 10. CNS - seizures, psychosis, depression, HAs, TIA, CVA 11. other findings include conjunctivitis and increased incidence of Raynaud's phenomenon and Sjorgen's syndrome |
|
|
Cutaneous symptoms of SLE/Lupus
|

butterfly/malar rash (erythematois rash over the cheeks and the bridge of the nose, found in 1/3 of patients), photosensitivity, discoid lesions (erythematous raised patches with keratotic scaling), oral and nasopharyngeal ulcers, alopecia, Raynaud's phenomenon
|
|
|
MSK symptoms of SLE/Lupus
|
musculoskeletal - joint pain (may be the first symptom - found in 90% of patients), arthritis (inflammatory and symmetric, not erosive as in RA), arthralgias, myalgia with or without myositis
|
|
|
Cardiac complications/symptoms of SLE/ Lupus
|
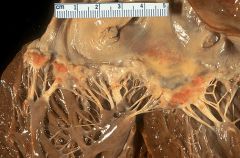
cardiac - pericarditis, endocarditis (libman-sacks endocarditis = serious complication), myocarditis
|
|
|
Pulmonary complications/symptoms of SLE/Lupus
|
pleuritis (most common pulmonary finding), pleural effusion, pneumonitis (may lead to fibrosis), pulmonary HTN (rare)
|
|
|
hematologic complications/symptoms of SLE/Lupus
|
pulmonary- hemolytic anemia with reticulocytosis or chronic disease, leukopenia, lymphopenia, and thrombocytopenia
|
|
|
Immunologic complications/symptoms of SLE/Lupus
|
impaired immune response due to many factors, including autoantibodies to lymphocytes, abnormal T cell function and immunosupressive medications
|
|
|
Epidemiology of SLE/Lupus
|
- women of childbearing age account for 90% of cases
- African-American patients are more frequently affected than Caucasian patients - very mild in elderly patients, more severe in children - usually appears in childhood or adolescence. |
|
|
Clinical findings associated with neonatal lupus
|
- skin lesions
- cardiac abnormalities (AV block, transposition of the great vessels) - valvular and septal defects |
|
|
Clinical course of SLE
|
- a chronic disease characterized by exacerbations and remissions
- malar rash, joint pain, and fatigue are the most common initial findings. With more advanced disease, renal, pulmonary, cardiovascular and nervous systems are affected |
|
|
renal complications/symptoms of SLE/Lupus
|
renal- proteinuria > 0.5 mg/day (may have nephrotic syndrome), cellular casts, glomerulopnephritis (may have hematuria), azotemia, pyuria, uremia, HTN
|
|
|
Diagnosis of SLE/Lupus
|
1. Positive ANA screen- sensitive but not specific- almost all patients with SLE have elevated ANA levels
2. Anti-ds DNA (in 40%) and anti-Sm Ab (in 30%). Tje presence of either of these is diagnostic of SLE- very specific 3. Anti-ss DNA(in 70%) 4. Antihistone Abs (in 70%) are present in 100% of cases of drug-induced lupus. If negative, drug induced lupus can be excluded 5. Ro (SS-A) and La (SS-B) are found in 15-35% -- associated with Sjogrens syndrome, subactue cutaneous SLE, and neonatal lupus with congenital heart block, d. complement deficiency (C2 and C4), e. ANA-negative lupus 6. positive LE preparation - ANAs bind to nuclei of damaged cells, producing LE bodies 7. False positive test results for syphilis 8. complement levels are usually decreased 9. CBC, renal function, UA, electrolytes 10. anticardiolipin and lupus anticoagulant |
|
|
Useful Criteria for diagnosing SLE/Lupus
|
A patient has SLE if 4 or more of these 11 criteria are positive at any time
1. mucocutanous signs (each counts as one)- butterfly rash, photosensitivity, oral and nasopharyngeal ulcers, discoid rash 2. arthritis 3. pericarditis, pleuritis 4. hematologic disease - hemolytic anemia with reticulocytosis, leukopenia, lymphopenia, thrombocytopenia 5. renal disease- proteinuria > 0.5 mg/day, cellular casts 6. CNS- seizures, psychosis 7. immunologic manifestations- positive LE prep, false positive test result for syphilis, anti-ds DNA, anti-Sm Ab 8. ANAs |
|
|
Conditions in which antinuclear antibodies (ANAs) are elevated
|
1. SLE
2. RA 3. Scleroderma 4. Sjogren's syndrome 5. Mixed connective tissue diseas 6. polymyositis and dermatomyositis 7. drug-induced lupus |
|
|
What blood test is always elevated in drug-induced lupus
|
Anti-histone antibodies-- if this is not elevated, then you can rule out the diagnosis
|
|
|
Conditions with positive RF
|
- RA (70% of patients)
- healthy populations (up to 3%) - neither sensitive nor specific for RA |
|
|
C-ANCA associated conditions
|
Wegener's granulomatosis - sensitive and specific
|
|
|
P-ANCA associated conditions
|
Polyarteritis Nodosa- 70-90% sensitive for microscopic PAN- not specific
|
|
|
Lupus anticoagulant
|
Antiphospholipid antibody syndrome
|
|
|
conditions associated with elevated ESR (erythrocyte sedimentation rate)
|
- infection (acute or chronic)
- malignancy - rheumatologic diseases - miscellaneous (tissue necrosis, pregnancy) - lower sensitivity and specificity, mostly used to diagnose an inflammatory process and monitor course of inflammatory conditions |
|
|
conditions associated with elevated C-reactive protein (CRP)
- compared to usefulness of elevated ESR - what if levels are markedly elevated? |
- inflammatory states and infection
- miscellaneous conditions (e.g. MI, vasculitis, trauma, malignancy, pancreatitis) - primarily used for infection- much more sensitive and specific than ESR - if levels are markedly elevated (>15) bacterial infection is likely present |
|
|
HLA Associations with Rheumatic Diseases
1. SLE 2. Sjogren's Syndrome 3. Rheumatoid Arthritis 4. Ankylosing spondylitis, Reiter's syndrome, psoriatic arthritis |
1. HLA-DR2 and HLA-DR3
2. HLA DR3 3. HLA - DR4 4. HLA- B27 |
|
|
Treatment of SLE/Lupus
|
1. Avoid sun exposure because it can exacerbate cutaneous rashes
2. NSAIDs -for less severe symptoms 3. Either local or systemic corticosteroids 4. Systemic corticosteroids for severe manifestations 5. Best long-term therapy is anti-malarial agents such as hydorxychloroquine- for consitutional, cutaneous and articular manifestations. It is continued as a preventive measure even after resolution of symptoms. Annual eye exam is needed because of retinal toxicity 6. Cytotoxic agents such as cyclophosphamide- for active glomerulonephritis 7. monitor the following and treat appropriately- Renal disease- produces the most significant morbidity associated with the disease, and HTN |
|
|
Scleroderma
1. definition 2. pathophysiology 3. who is most commonly affected 4. two types |

1. A chronic connective tissue disorder that can lead to widespread fibrosis
2. pathophysiology- cytokines stimulate fibroblasts, causing an abnormal amount of collagen deposition. It is the high quantity of collagen that causes the problems associated with this disease (composition of collagen is normal) 3. scleroderma is more common in women. The average age of onset is 35-50 years 4. There are two types of sclerodema : Diffuse (20%) and limited (80%) |
|
|
Clinical features of Scleroderma
|

1. Raynaud's phenomenon- present is almost all patients, usually appears before the other findings. caused by vasospam and thickening of vessel walls in the digits. This can lead to digital ischemia, with ulceration and infarction/gangrene. Cold temperature and stress bring about color changes of the fingers- blanching first, then cyanotic, and then red
2. cutaneous fibrosis- tightening of the skin of the face and extremities (sclerodactyly refers to the claw-like appearance of the hand). Can lead to contractures, disability, and disfigurement 3. GI involvement - occurs in most patients (both diffuse and limited). Findings include dysphagia/reflux from esophageal immobility (up to 90% of patients), delayed gastric emptying, constipation/diarrhea, abdominal distention, and pseudo-obstruction. Prolonged acid-reflus may eventually lead to esophageal strictures 4. pulmonary involvement- most common cause of death from scleroderma. Interstitial fibrosis and/or pulmonary HTN may be present 5. Cardiac involvement- pericardial effusions, myocardial involvement that can lead to CHF, arrhythmias 6. Renal involvement (renal crisis- rapid malignant hypertension) occurs in patients with diffuse disease (rare today) |
|
|
What is the most common cause of death in scleroderma?
|
pulmonary involvement (interstitial fibrosis or pulmonary HTN)
|
|
|
Diagnosis of scleroderma
|
1. diagnostic tests are of limited utility. Almost all patients have elevated ANAs (high sensitivity, low specificity)
2. Anticentromere antibody- very specific for the limited form 3. antitopoisomerase I (antiscleroderma-70) Ab is very specific for diffuse form 4. barium swallow (esophageal dysmotility) and pulmonary function tests are used to detect complications |
|
|
Treatment for scleroderma
|
1. No effective cure
2. Treat symptoms - NSAIDs for musculoskeletal pains, H2 blockers or PPIs for esophageal reflux 3. Raynaud's phenomenon- avoid cold and smoking, keep hands warm. If severe, use calcium-channel blockers 4. treat pulmonary and renal complications as they arise |
|
|
Sjorgen's Syndrome
|
1. autoimmune disease most commonly seen in women. Lymphocytes infiltrate and destroy the lacrimal and salivary glands
2. a multiorgan disease (can also involve the skin, lungs, thyroid, vessels and liver) |
|
|
Primary versus secondary Sjogrens syndrome
|
- Primary- dry eyes and dry mouth, along with lymphocytic infiltrations of the minor salivary glands (on histology), patients do not have another rheumatologic disease
- secondary - dry eyes and dry mouth along with connective tissue disease (RA, systemic sclerosis, SLE and polymyositis) |
|
|
What are patients with Sjogren's syndrome at an increased risk for? What is the most common cause of death in Sjogrens?
|
- patients have increased risk of non-Hodgkins lymphoma. malignancy is the most common cause of death
|
|
|
Clinical features of SJogrens syndrome
|
- dry eyes- burning, redness, and blurred vision
- dry mouth - arthralgias, arthritis, and fatigue - many extraglandular manifestations (more common in primary disease), such as chronic arthritis, interstitial nephritis, and vasculitis |
|
|
Diagnosis of Sjogren's syndrome
|
1. ANAs present in 95% of patients.
2. Rheumatoid factor is present in 50-75% of patients with secondary disease 3. Ro (SS-a) is present in 55% of patients, and La (SS-B) Abs are present in 40% of patients 4. Non-specific findings - increased ESR, normocytic normochromic anemia, leukopenia 5. Schirmer test- filter paper inserted in eye to measure lacrimal gland output (degree of wetting in a specified time period)-- high sensitivity and specificity 6. salivary gland biopsy (lip or parotid) is the most accurate but not needed for diagnosis |
|
|
Treatment of Scleroderma
|
1. Pilocarpine or Cevimeline 9enhance oral and ocular secretions)
2. Artificial tears for dry eyes 3. good oral hygiene 4. NSAIDs, steroids for arthralgias, and arthritis 5. Patients with secondary Sjogren syndrome- therapy for connective tissue disease |
|
|
Mixed Connective Tissue Disease
|
- MCT Disease is an "overlap" syndrome with clinical features similar to those of SLE, RA, systemic sclerosis, and polymyositis. Findings consistent with each of the disease do not necessarily occur simultaneously. It usually takes some time for a pattern to be identified and diagnosis of mixed connective tissue disease to be made
- clinical findings include pulmonary involvement, esophageal dysfunction, polyarthritis, sclerodactyly, cutaneous malformations, myopathy, and Raynaud's phenomenon. - the presence of anti-U1 RNP Abs is the key laboratory finding. High ANA and RF may be present - treatment varies according to which specific disease predominates |
|
|
Patients with SLE/Lupus and what specific blood test result are at an increased risk of having a child with neonatal SLE with congenital heart block
|
Ro (SS-A)
|
|
|
Rheumatoid Arthritis- general characteristics
1. definition 2. what type of disease is it? 3. epidemiology 4. severity of disease 5. etiology |
1. Ra is a chronic inflammatory disease autoimmune disease involving the synovium of the joints. The inflamed synoviym can cause damage to the cartilage and bone
2. It is a systemic disease that has many extra-articular manifestations 3. The usual age of onset is 20-40 years-- it is more common in women than in men (3:1) 4. Disease severity is variable- some patients have moderate restrictions and are capable of performing ADLs, whereas others are confined to a wheelchair or bed 5. Etiology is uncertain. It may be caused by an infection or a series of infections (most likely viral), but genetic predisposition is necessary |
|
|
Clinical features of Rheumatoid arthritis -- joint symptoms
|
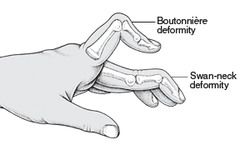
1. Inflammatory polyarthritis (joint swelling is the most common sign)- can involve every joint in the body except the distal interphalangeal (DIP) joints
- pain on motion of the joints/tenderness in the joints - joints most commonly involved are the joints of the nads (PIP, MCP), wristes, knees, ankles, alebows, hips and shoulders -characteristic hand deformities - ulnar deviation of the MCP joints. Boutinnere deformities of the PIP joints (PIP flexed, DIP hyperextended). Swan-neck deformity of the fingers (MCP flexed, PIP hyperextended, DIP flexed) - cervical spine involvement is common at C1-C2 (subluxation and instability)- but is less common in the lower cervical spine. a. Instability of teh cervical spine is a potentially life-threatning complication of RA. Most patients do NOT have neurologic involvement, but if they do, it can be progressive and fatal if not surgically treated. b. This is seen in 30-40% of patients. All patients with RA should have C-spine films before undergoing any surgery (due to risk of neurologic injury during intubation) |
|
|
Clinical features of Rheumatoid arthritis -- constitutional symptoms
|
1. morning stiffness - present in all patients - improves as the day progresses
2. low-grade fever, weight loss 3. fatigue can be prominent because it is a systemic disease (morning stiffness, symmetrical joint involvement, and nodules are no longer needed for a diagnosis of RA) |
|
|
Clinical features of Rheumatoid arthritis
a. cardiac b. pulmonary c. ocular d. soft tissues e. mucous membranes f. nodules |

a. cardiac- pericarditis, pericardial effusions, conduction abnormalities and valvular incompetence
b. pulmonary- pleural effusions, interstitial fibrosis may occur c. ocular- episcleritis or scleritis d. soft tissue swelling (rather than bony enlargement e. drying of the mucous membranes - Sjogrens xerostomia f. subQ rheumatoid nodules over extensor surfaces may also occur in visceral structures - e.g. lungs, pleura, pericardium- pathognomic for RA. Nearly always occurs in seropositive patients (ie those with RF) |
|
|
Diagnosis of Rheumatoid Arthritis - lab findings
|
1. Laboratory findings- high titers of RF are associated wtih more severe diseae and are generally non-specific. RF is eventually present in 80% of patients with RA (may be absent early in the disease), but also present in up to 3% of healthy population. RF titers rarely change with disease activity and are not useful in following patients. It is, however, helpful in determining prognosis as high titers indicate more severe disease
b. anti-citrullinated peptide/protein antibodies (ACPA)- sensitivity is 50% to 75% and specificity is over 90% c. elevated ESR, and CRP d. normocytic normochromic anemia (anemia of chronic disease) |
|
|
Diagnosis of Rheumatoid arthritis- X-rays and synovial fluid analysis
|

1. Loss of juxta-articular bone mass (periarticular osteoporosis) near the finger joints
2. Narrowing of the joint space (due to thinning of the articular cartilage) is usually seen late in the disease 3. bony erosions at the margins of the joint 4. synovial fluid analysis is non-specific |
|
|
Treatment of rheumatoid arthritis
|
1. Principles of treatment- the goals of treatment are to prevent or halt joint destruction and to come as a close to clinical remission as possible while avoiding the toxicity of the anti-RA medication. Treatment must be individualized to the patient. A treatment regiment that works for one patient may not work for another.
2. exercise helps to maintain range of motion and muscle strength 3. Symptomatic treatment - NSAIDS are the drug of choice for pain control. Corticosteroids (low dose) - use these if NSAIDs do not provide adequate relief. Short-term treatment may be appropriate but avoid long-term use. 4. Disease-modifying antirheumatic drugs (DMARDS)- general principles- can reduce morbidity and mortality (by nearly 30%) - by limiting complications, slowing progression of disease, and preserving joint function. Should be initiated early (at the time of diagnosis). They have slow onset of action (6 weeks or longer for any effect to be seen), so begin treating RA while waiting for the disease-modifying therapy to take effect. Once the effect is evident, gradually taper and discotinue NSAIDs and corticosteroids and continue the disease-modifying program ** much of the joint damage that ultimately leads to disability occurs early in the course of the disease so early treatment with DMARDs is critical |
|
|
Extra-articular symptoms of rheumatoid arthritis
1. cutaneous 2. pulmonary 3. cardiac |
1. cutaneous- skin becomes thin and atrophic and bruises easily. Vasculitic changes/ulcerations involving the finger, nail folds. SubQ rheumatoid nodules (elbows, sacrum, occiput) -- pathognomic for RA
2. pulmonary- Pleural effusions (very common) - pleural fluid characteristically has very low glucose and low complement. Pulmonary fibrosis with restrictive pattern on PFTs and honeycomb pattern on CXR. Pulmonary infiltrates. Rheumatic nodules in the lungs (similar to those on the skin) - can cavitate or become infected 3. Cardiac- rheumatic nodules in the heart can lead to conduction disturbances (heart block and bundle branch nblock). Pericarditis in 40% of patients with RA, and pericardial effusion |
|
|
Extra-articular manifestations of RA
1. eyes 2. nervous system 3. felty's syndrome |
1. scleritis, scleromalacia -softening of the sclera, if not treated my perforate, leading to blindness. Dry eyes and mucous membranes (may develop Sjogrens syndrome)
2. Nervous system- mononeuritis multiplex -infraction of the nerve trunk. Patient canno move the arm or leg, which implies systemic vasculitis, which is a bad sign 3. felty's syndrome- triad of RA, neutropenia, and splenomegaly. Also see anemia, thrombocytopenia, and lymphadenopathy. Associated with high titers of RF and extra-articular disease. Increased susceptibility to infection. Usually occurs failrey late in the disease process |
|
|
Extra-articular manifestations of RA
1. Blood 2. Vasculitis |
1. Blood - anemia of chronic disease: mild, normocytic, normochromic anemia, and thrombocytosis
2. Vasculitis-- a microvascular vasculitis- can progress to mesenteric vasculitis, Polyarteritis Nodosum, and other vascular syndromes |
|
|
If joint distribution is NOT symmetric or DIP is involved or constitutional symptoms (including morning stiffness) are absent, how likely is the diagnosis of RA?
|
NOT likely
|
|
|
What is the clinical course like in most patients with RA?
|
Patient has episodes of exacerbations and remissions but remissions are really only improvements, as patients are symptomatic all the time to some extent
|
|
|
Diagnosis of RA
|
1. inflammatory arthritis of three or more joints- MCP, PIP, wrist, elbow, knee, ankle, MIP joints
2. symptoms lasting at least 6 weeks 3. Elevated ESR and CRP 4. positive RF or ACPA (anti-citrullinated peptide/protein antibodies) 5. Radiologic changes consistent with RA (erosiions and periarticular decalcification) |
|
|
Poor prognostic indicators in RA
|
1. High RF titers
2. subQ nodules 3. erosive arthritis 3. autoantibodies to RF |
|
|
Variants of RA
1. Felty syndrome 2. Juvenile RA |
1. Anemia, neutropenia, splenomegaly and RA
2. begins before age 18. Extra-articular manifestations may predominate (still's disease) or arthritis may predominate |
|
|
Treatment of RA
1. first-line agents - DMARDs 2. surgery |
1. Methotrexate- best initial DMARD. Initial improvement is seen in 4-6 weeks. Nearly 80% of treated patients will experience moderate-to-excellen symptomatic benefit from treatment, however remission is rare. Side effect include GI upset, oral ulcers (stomatitis), mild alopecia, bone marrow suppression, hepatocellular injury, and indiosyncratic interstitial pneumonitis, which may lead to pulmonary fibrosis
- closely monitor LFTs and renal function - supplemnt with folate - lefluomide is alternative - hydroxychloroquine- alternative first-line agent but not as effective as MTX. It requires eye exams q6 mo because of the risk of visual loss due to retinopathy (although quite rare) - sulfazalazine- alternate first-line agent, but less effective than MTX. - Anti-tumor necrosis factor (anti-TNF) inhibiting agents (entanercept, infliximab) - used if MTX does not fully control the disease 2. surgery in rare cases may include: synovectomy (arthroscopicv) decrease joint pain and swelling but does not prevent X-ray progression and does not improve joint ROM. Joint replacement surgery for severe pain refractory to more conservative measures |
|
|
2 types of crystal-induced arthritides
|
1. Gout
2. pseudogout (calcium pyrophosphate deposition disease) |
|
|
Gout- general characteristics
1. definition 2. epidemiology- who is predominantly affected |
1. inflammatory MONO-articular arthritis caused by crystallization of monosodium urate in joints. Hyperuricemia is a hallmark of the disease but does not by itself indicate gout
2. 90% of patients are men over age 30 years of age. Women are not typically affected until after menopause |
|
|
Pathogenesis of gout- 2 main ways it develops
|
1. increased production of uric acid - hypoxanthine-guanine phosphoribosytransferase deficiency - e.g. Lesch-Nyhan syndrome
- phosphoribosyl pyrophosphate synthetase overactivity - increased cell turnover associated with a number of conditions, including cancer chemotherapy, chronic hemolysis and hematologic malignancies 2. decreased excretion of uric acid - accounts for 90% of the cases-- renal disease, NSAIDs, diuretics, acidosis |
|
|
Pathophysiology of inflammation in gout
|
1. PMNs play a key role in acute inflammation of gout
2. It develops when uric acid crystal collect in the synovial fluid as the extracellular fluid become saturated with uric acid 3. IgGs coat monosodium urate crystals, which are phagocytized by PMNs, leading to the release of inflammatory mediators and proteolytic enzymes from the PMNS, which then result in inflammation |
|
|
Gout- clinical features
1. asx 2. acute gouty arthritis |

1. Asymptomatic hyperuricemia- increased serum uric acid level in the absence of clinical findings or gout, may be present without symptoms for 10-20 years or longer. Should not be treated because over 95% of patient remain asx
2. Acute gouty arthritis- peak age of onset is 40-60 yo in men. Initial attack usually involves one joint of the lower extremity. There is a sudden onset of exquisite pain- the patient may be unable to tolerate a bed sheet on the affected joint. Pain often awakens the patient from sleep. Most often affects the big toe in the first metotarsophalangeal joint (PODAGRA). Other commonly affected joints include the ankles and knees |
|
|
Gout - clinical features
1. Intercritical gout 2. chronic tophaceous gout- what is a tophi and where and when do they most commonly occur? |

1. An asymptomatic period after the initial attack. The patient may not have another attack for years. Sixty percent of patients have recurrence within 1 yr. Some patients (<10%) never have another acute attack. There is a 75% chance of a second attack within the first 2 years. Attacks tend to become polyarticular with increased severity over time
2. Chronic tophaceous gout- occurs in people with poorly controlled gout for more than 10-20 years. Tophi are aggregations of urate crystals surrounded by giant cells in an inflammatory reaction. Seen only after several attacks of acute gout, noted after an average of 10 years following the initial attack. Tophi cause deformity and destruction of hard and soft tissues. In joints, they lead to destruction of cartilage and bone, triggering secondary degeneration and development of arthritis. They may be extra-articular. common locations- extensor surface of forearms, elbows, knees, achilles tendons, and pinna of the external ear |
|
|
Diagnosis of gout
|

1. Joint aspiration and synovial fluid analysis (under a polarizing microscope) is the only way to make a definitive diagnosis - needle shaped and negatively birefringent urate crystals appear in the synovial fluid
2. serum uric acid is NOT helpful in making the diagnosis because be normal even during an acute gouty attack 3. Radiographs reveal punched-out erosions with an overhanging rim of cortical bone |
|
|
Treatment of gout
1. all stages 2. acute gout |
1. In all stages, avoid secondary causes of hyperuricemia- medications that increase uric acid levels (thiazide and loop diuretics). Obesity, reduce EtOH intake and dietary purine intake - limit intake of seafood and red meat
2. acute gout- bed rest is important as early ambulation may precipitate a recurrence. - NSAIDs- treatment of choice in acute gout (indomethacin is traditionally used, but other NSAIDs are effective). Very effective in relieving pain promptly, best if initiated early-- a delay in initiating therapy can impair response - colchicine - an alternative for patients who cannot take NSAIDs or did not respond to them. Effective but less favored because 80% of treated patients develop significant n/v, abdominal cramps, and severe diarrhea. Compliance therefore tends to be low. It is contraindicated in renal failure and cytopenia. -corticosteroids- oral prednisone (7-10 day coursE) if the patient does not respond to or cannot tolerate NSAIDs or colchicine. Intra-articular corticosteroid injections (if only one joint is involved) produces dramatic relief of symptoms |
|
|
Prophylactic therapy for gout
|
1. Wait until patient has had at least two gouty attack (or perhaps three), before initiating prophylactic therapy. Two attacks per year is sometimes used as a rough guideline. This is because the second attack may take years to occur (if at all), and so the risk-to-benefit ratio for prophylactic medication (allopurinol or uricosuric agents) is not favorable after one gouty attack. When giving prophylaxis, give either colchicine or an NSAID for 3-6 months to prevent an acute attack. These can then be discontinued and the patient can remain on a uricosuric agent or allopurinol indefinitely
- the choice of whether to use a uricosuric drug or allopurinol depends how much uric acid is excreted in the urine in a 24 hour period. if <800 mg/day this indicates undersecretion and a uricosuric should be used if the patient has normal renal function (probenecid or sulfinpyrazone) - CI if h/o renal stones - allopurinol - a xanthine oxidase inhibitor decreases uric acid synthesis- if the 24 hour urine uric acid is >800 mg/day this indicates overproduction. NEVER give this for acute gout as it makes it worse. Watch for SJS. |
|
|
Pseudogout (calcium pyrophosphate deposition disease)- general characteristics
1. what is it? 2. risk factors? |
1. calcium pyrophosphate crystal deposits in the joints, leading to inflammation.
2. risk factors include: deposition increases with age and with OA of the joints. Therefore pseudogout is common in elderly patients with degenerative joint disease. Other conditions that may increase crystal deposition include hemochromatosis, hyperparathyroidism, hypothyroidism, and Bartter's syndrome |
|
|
Clinical features of pseudogout (CPDD)
|

1. The most commonly affected joints are the knees and the wrists
2. this is classically monoarticular, but can be polyarticular as well ** Presentation is similar to gout but typically occurs in the larger joints (knee) |
|
|
Diagnosis of pseudogout (CPDD)
|
1. Joint aspiration is required for definitive diagnosis- weakly positively birefringent rod-shaped and rhomboidal crystals in synovial fluid (calcium pyrophosphate crystals)
2. radiographs- chondrocalcinosis (cartilage calcification) |
|
|
Treatment of pseudogout (CPDD)
|
1. Treat the underlying disorder (if identified)
2. Symptomatic management is similar to that for gout (NSAIDs, colchicine, and intraarticular steroid injections) 3. Total joint replacement is appropriate if sx are debilitating |
|
|
Idiopathic Inflammatory Myopathies- general characteristics
1. what is it? 2. epidemiology 3. classifications/types |
1. The term polymyositis is used when the condition does not involve the skin (usually occurs in adults). The term dermatomyositis is used when polymyositis is associated with a characteristic skin rash
2. more common in female patients 3. Polymyositis, dermatomyositis, childhood onset dermatomyositis - subQ calcifications, myositis associated with collagen vascular disease, and myositis associated with malignancy, inclusion body myositis - "oddball" for the following reasons-- affects males more than femals, there is absence of autoantibodies, distal muscle involvement and relatively low CK, prognosis is poor |
|
|
Clinical features of Idiopathic Inflammatory Myopathies - features common to both polymyositis and dermatomyositis
|
1. features common to both polymyositis and dermatomyositis
- symmetrical proximal muscles weakness that develops subacutely over weeks or several months - the earliest and most severely affected muscle groups are the NECK FLEXORs, shoulder girdle and pelvic girdle muscles. Distal extremity weakness is less frequent and typically less severe. Myalgia is present in 33% of patients and dysphagia is present in up to 30% of patients |
|
|
clinical features of dermatomyositis
|

1. heliptrope rash (butterfly) - around eyes, bridge of nose, and cheeks
2. gottron's papules- papular erythematous, scaly lesions over the knuckles (MCP, PIP, DIP) 3. V sign - rash on face, neck, and anterior chest 4. shawl sign- rash on the shoulders and upper back, elbows, knees 5. periungual erythema and telangiectasias 6. subQ calcifications in children - can be extremely painful |
|
|
Gottron's papules
|

seen in dermatomyositis - papular, erythematous, scaly lesions over the knuckles
|
|
|
Associated findings in polymyositis and dermatomyositis
|
- athralgias (common)
- CHF and conduction defects are rare - Interstitial lung disease (in the minority of patients) |
|
|
Associated findings of dermatomyositis
|
- vasculitis of the GI tract, kidneys, lungs and eyes (more common in children)
- there is increased malignancy in older adults (lung, breast, ovary, GI tract, and myeloproliferative disorders) - once dermatomyositis is diagnosed, make an effort to uncover an occult malignancy. Dermatomyositis associated with malignancy often remits once the tumor is removed. |
|
|
Diagnosis of polymyositis/dermatomyositis
1. Labs 2. Other |
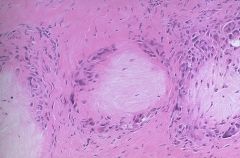
1. CK is significantly elevated. CK Levels correspond to the degree of muscle necrosis, so one can monitor the disease severity
- LDH, aldolase, AST, ALT elevated - ANA in over 50% - anti-sythethase antibodies (anti-Jo-1 antibodies)- abrupt onset of fever, cracked hands, Raynaud's phenomenon, interstitial lung disease, arthritis, does NOT respond well to therapy - Anti-signal recognition particle - cardiac manifestations (common, worst prognosis of all subsets) - anti-Mi-2 antibodies - better prognosis 2. EMG - abnormal in 90% of patients 3. Muscle biopsy - shows inflammation and muscle fiber fibrosis. dermatomyositis- perivascular and perimysial, polymyositis and inclusion body myositis- endomysial |
|
|
Treatment of polymyositis and dermatomyositis
|
1. Corticosteroids are the initial treatment. Continue until symptoms improve and slowly taper (may take up to 2 years)
2. Immunosuppressive- agents (for patients who do not respond to steroids) - MTX, cyclophosphamide, chorambucil 3. physical therapy |
|
|
Inclusion Body Myositis
|
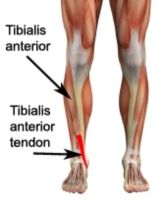
- more common in men (elderly)
- Insidious onset of slowly progressive proximal and distal weakness, often leads to a delay in diagnosis - There is early weakness and atropy of the quadriceps, forearm flexors, and tibialis anterior muscles. Involvement is asymmetrical. Facial weakness occurs in 1/3 of patients and dysphagia in 1/2 of patients - patients can also have loss of DTRs (nerves are NOT involved in dermatomysositis and polymyositis) - extramuscular manifestations are rare - diagnosis- slight elevation of CK levels (relatively low) - poor response to therapy |
|
|
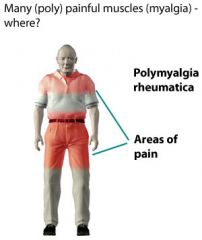
Polymyalgia Rheumatica - general characteristics
1. epidemiology- gender, age of onset etc 2. cause 3. course |
1. usually occurs in elderly patients (rare before age 50). The mean age of onset is 70 and it is more common in women
2. the cause is unknown, but autoimmune process may be responsible and there is a possible association with HLA-DR4 - genetic link 3. self-limited disease (duration of 1-2 years) |
|
|
Clinical features of polymyalgia rheumatica (PMR)
|
1. hip and shoulder muscle pain (bilateral)- often begins abruptly but may be gradual. Stiffness in shoulder and hip regions after a period of inactivity is the most prominent symptom. Pain occurs on movement, but muscle strength is normal. Profound morning stiffness is common
2. constitutional symptoms- usually present. Malaise fever, depression, weight loss and fatigue 3. Joint swelling- up to 20% of patients have synovitis in knees, wrists or hand joints (can be confused with RA). Synovitis and tenosynovitis around the shoulder may lead to rotator cuff tendonitis and adhesive capsulitis ** associated with giant cell/temporal arteritis |
|
|
Diagnosis of polymalgia rheumatica
|
- this is essentially a clinical diagnosis
- ESR is usually elevated and aids in the diagnosis. It is almost always > 50 and frequently > 100. Correlates with disease activity |
|
|
Treatment of polymyalgia rheumatica (PMR)
|
1. Corticosteroids- response usually occurs within 1-7 days. they are not curative, but are effective in suppressing inflammation until the disease resolves itself
2. after 4-6 weeks, begin to taper slowly 3. most patients (60-70%) can stop corticosteroids within 2 years. A few may have sx for up to 10 yrs |
|
|
Fibromyalgia- general characteristics
1. epidemiology 2. course 3. key to diagnosis 4. etiology |
1. adult women account for 80-90% of cases
2. chronic non-progressive course with waxing and waning symptoms, but many patients improve with time 3. key to dx- multiple trigger points (points that are tender to palpation) - symmetrical, 18 characteristic locations have been determine including the occiput, neck, hsoulder, ribs, elbows, buttocks and knees 4. etiology is unknown and somatization is not a proven cause |
|
|
Clinical features of fibromyalgia
|
1. stiffness, body aches (MSK) and fatigue
- pain is constant and aching, and is aggravated by weather changes, stress, sleep deprivation, and cold temperature. It is worse in the morning. Rest, warmth and mild exercise improve the pain 2. sleep patterns are disrupted and sleep is unrefreshing 3. anxiety and depression are common |
|
|
Diagnostic criteria for fibromyalgia
|
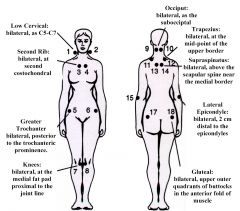
1. Widespread pain including axial pain for at least 3 months
2. pain in at least 11 of the 18 possible tender points 3. before confirming the diagnosis, r/o myofascial syndromes, rheumatoid disease, PMR, ankylosing spondylitis, spondyloarthropathy, chronic fatigue syndrome, Lyme disease, hypothyroidism, polymyositis, depression and somatization disorder, and hypertrophic osteoarthropathy |
|
|
Treatment/Management of fibromyalgia
|
1. Advise the patient to stay active and productive
2. medications are generally NOT effective. SSRIs and TCAs have shown some benefit and may be beneficial. Avoid narcotics. 3. CBT, exercise and consider psych eval |
|
|
Ankylosing Spondylitis - general characteristics
1. epidemiology 2. things to look for on hx 3. pre-req for dx 4. age of onet 5. classic characteristic 6. course |

1. strong association with HLA-B27 (90$ of patients). three times more common in men than women.
2. look for a positive fhx of ank spond, IBD or psoriasis 3. bilateral sacroiliitis is pre-req for making the dx 4. onset is in adolesence or young adulthood 5. It is characterized by "fusion" of the spine (bamboo-spine) in an ascending manner (from lumbar to cervical spine) 6. Course- slow progression, but course is highly variable. Acute exacerbations are common. Life expectancy is normal. The first 10 years of the disease can give an indication of long-term severity |
|
|
Clinical features of ankylosing spondylitis
|

1. Low back pain and stiffness (secondary to sacroiliitis) - limited motion in the lumbar spine
2. Neck pain and limited motion in the cervical spine- occurs later in the course of disease 3. enthesitis - inflammation at the tendinous insertions into the bone (achilles tendon and supraspinatus tendons) 4. with extensive spinal involvement, the spine becomes brittle and is prone to fractures with minimal trauma. Severe spinal cord injury can occur with such trauma 5. chest pain and diminished chest expansion - due to thoracic spine involvement 6. shoulder and hip pain- most commonly the peripheral joints are affected 7. constitutional features- fatigue, low-grade fever, weight loss 8. Extra-articular manifestations (eye involvement- acute anterior uveitis or iridocyclitis). Other features are rare but include- cardiac, rnelan pulmonary and nervous system involvement 9. Loss of lumbar lordosis can occur as disease advances , leading to inability to stand upright. When severe and symptomatic, this may require spine reconstruction |
|
|
Diagnosis of ankylosing spondylitis
|
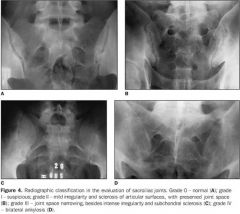
Imaging studies of the lumbar spin and pelvis (plain film, MRI and CT) reveal sacroiliitis - sclerotic changes in the sacroiliac area. Eventually, the vertebral columns fuse and produce a "bamboo spine"
2. Elevated ESR in up to 75% of patients due to inflammation- non-specific 3. HLA-B27 is not necessary for the diagnosis. Present in 8% of the general population |
|
|
Treatment of ankylosing spondylitis
|
1. NSAIDs (indomethacin) for symptomatic relief
2. Anti-TNF medications (etancercept, infliximab) 3. Physical therapy- maintaining good posture, extension exercises 4. surgery may be necessary in some patients with severe spinal deformity 5. Patients with ank spond who sustain even minor trauma and who complain of neck or back pain should be strictly immobilized to prevent spinal cord injury until thorough imaging studies are obtained |
|
|
Reactive arthritis- general characteristics
1. definition 2. associations 3. examples 4. associated organisms |
1. asymmetric inflammatory oligoarthritis of the lower extremities (upper extremities less commonly). This arthritis is preceded by an infectious process that is remote from the site of arthritis (1-4 weeks prior) usually after enteric or urogenital infections
2. It occurs mostly in HLA-B27 positive individuals 3. Reiter's syndrome= example. classic triad includes urethritis, arthritis, uveitis (can't see, can't pee, can't climb a tree)- but meeting the criteria for this triad is rare so it is usually called reactive arthritis now 4. associated with salmonella, shigella, campylobacter, chlamydia, and yersinia |
|
|
Clinical features of reactive arthritis
|
1. lookf for evidence of infection (GI or GU) 1 to 4 weeks before the onset of the symptoms
2. asymmetric arthritis - new joints may be involved sequentially over days. Joints are painful, with effusions and lack of mobility 3. fatigue, malaise, weight loss, and fever are common 4. joint pain may persist or recur over a long-period |
|
|
Diagnosis of reactive arthritis
|
1. send synovial fluid for analysis (to r/o infection or crystals)
|
|
|
Treatment of reactive arthritis
|
1. NSAIDs are first line therapy
2. If there is no response, then try sulfazalazine and immunosuppressive agents such as azathioprine (AZP) 3. Antibiotic use is controversial-- usually not given |
|
|
Psoriatic arthritis
|

1. develops in less than 10% of patients with psoriasis
2. It is typically gradual in onset. Patients usually have skin disease for months to years before arthritis develops 3. Usually asymmetric and polyarticular 4. Upper extremities are most commonly involved- smaller joints more commonly than larger joints 5. Initial treatment is NSAIDs, but persistent arthritis may require drugs used to treat RA - may see pencil-in-cup deformity or sausage digits |
|
|
Temporal Arteritis aka Giant Cell Arteritis
- etiology - what is affected - epidemiology |
vasculitis of unknown cause that typically presents in patients > 50 years of age and is twice as common in women as in men
- the temporal arteries are most commonly affected, but it may involve other arteries, such as the aorta and carotids - associated with an increased risk of aortic aneurysm and aortic dissection |
|
|
clinical features of temporal/giant cell arteritis
|

1. constitutional sx- malaise, fatigue, weight loss, and low grade fever
2. HA- can be severe 3. visual impairment - in only 25-50%. Caused by involvement of the ophthalmic artery. Optic neuritis, amarosis fugax may lead to blindness in up to 50% if not treated aggressively and quickly 4. Jaw pain with chewing- intermittent claudication of jaw/tongue when chewing 5. tenderness over the temporal artery, absent temporal pulse 6. palpable nodules 7. 40% of patients also have polymyalgia rheumatica (PMR) |
|
|
Diagnosis of temporal arteritis/giant cell arteritis
|
1. ESR is elevated (but a normal value does not exclude the diagnosis)
2. Biopsy of the temporal artery has a sensitivity of 90%. A single negative biopsy does not exclude the diagnosis |
|
|
Treatment of temporal arteritis
|
1. use high-dose steroids (prednisone) early to prevent blindness.
- start treatment immediately, even if temporal arteritis is only suspected. DO NOT wait for biopsy results. If visual loss is present, admit the patient to the hospital for IV steroids, otherwise start oral prednisone. - if the diagnosis is confirmed, continue treatment for at least 4 weeks, then taper gradually, but maintain steroid therapy for up to 2-3 years. Relapse is likely to occur is steroids are stroppy prematurely 2. Follow up on ESR levels to monitor effectiveness of treatment. 3. visual loss in one eye may be temporary or permanent. Prompt and aggressive steroid treatment is primary given to prevent involvement of the other eye, but it may improve outcome in the affected eye as well 4. Even if untreated, the disease is usually self-limiting in most patients, although vision loss may be permanent |
|
|
Keys to diagnosing temporal arteritis
|
1. age > 50 years
2. new headache 3. tender/palpable temporal artery 4. high ESR 5. jaw claudication |
|
|
Takayasu's arteritis - general characteristics
1. epidemiology 2. what is it? 3. how is it diagnosed? |
1. most common in young asian women
2. vasculitis of the aortic arch and its major branches - potentially leading to stenosis or narrowing of the vessels 3. diagnosed via arteriogram |
|
|
clinical features of takayasu's arteritis
|
1. constitutional symptoms - fever, night sweats, malaise, arthralgias, fatigue
2. pain and tenderness over the involved vessels 3. absent pulses in the carotid, radial or ulnar arteries: aortic regurgitation may be present 4. signs and symptoms of ischemia eventually develop in areas supplies by involved vessels 5. severe complications include limb ischemia, aortic aneurysms, aortic regurgitation, stroke and secondary HTN due to renal artery stenosis. The main prognostic indicator is the presence or absence of these conditions |
|
|
Treatment of Takayasu's arteritis
|
1. steroids may relieve the symptoms
2. treat HTN 3. Surgery or angioplasty may be required to recannulate stenosed vessels. Bypass grafting is sometimes necessary |
|
|
Churg-Strauss Syndrome
|
1. Vasculitis involving many organ systems (respiratory, cardiac, GI, renal, skin, neurologic)
2. Clinical features include constitutional findings (fever, fatigue, weight loss), prominent respiratory tract findings (asthma, dyspnea), and skin lesions (subQ nodules and palpable purpura) 3. diagnosis is made by lung or skin biopsy (prominence of eosinophils). It is associated with P-ANCA 4. The prognosis is poor with a 5 year survival of 25% (death is usually due to cardiac or pulmonary complications). With treatment (steroids), the 5-year prognosis improves to 50% |
|
|
What should you suspect in a young woman with decreased/absent peripheral pulses, discrepancies of BP (in arm vs leg) and arterial bruits?
|
Takayasu's arteritis
|
|
|
Wegener's Granulomatosis- general characteristics
|
vasculitis predominantly involving the kidneys and upper and lower respiratory tract (sometimes other organs as well)
|
|
|
Clinical features of wegener's granulomatosis
|
1. Upper respiratory symptoms (e.g. sinusitis), purulent or bloody nasal discharge
2. oral ulcers (may be painful) 3. pulmonary symptoms (cough, hemoptysis, dyspnea) 4. renal involvement (glomerulonephritis- may have rapidly progressive renal failure) 5. eye disease (conjuctivitis, scleritis) 6. MSK- arthralgias and myalgias 7. tracheal stenosis 8. constitutional findings (e.g. fever, weight loss) |
|
|
Diagnosis of Wegener's granulomatosis
|
1. CXR is abnormal (nodules or infiltrates)
2. Laboratory findings: Markedly elevated ESR, anemia (normochromic normocytic), hematuria, positive c-ANCA in 90% of patients - sensitive and specific, thrombocytopenia may be present 3. open lung biopsy confirms diagnosis ** may have a saddle nose deformity |
|
|
Prognosis and treatment of Wegener's granulomatosis
|

1. Prognosis is poor- most patients die within 1 year after the diagnosis
2. a combination of cyclophosphamide and corticosteroids can induce remissions in many patients, but relapse may occur any time 3. consider renal transplant if the patient has ESRD **renal disease accounts for the majority of the deaths |
|
|
Polyarteritis Nodosa (PAN)
|
1. Vasculitis of medium-sized vessels involving the nervous system and GI tract
2. Can be associated with hepatitis B, HIV, and drug reactions 3. Pathophys- PMN invasion of all layers and fibrinoid necrosis plus resulting intimal proliferation lead to reduced luminal area, which results in ischemia, infarction and aneurysms ** There is no pulmonary involvement with Polyerteritis Nodosa which distinguishes it from Wegeners |
|
|
Clinical findings of polyarteritis nodosum
|
1. early symptoms are fever, weakness, weight loss, myalgias, and arthralgias, and abdominal pain (bowel angina)
2. Other findings are HTN, mononeuritic multiplex, and livedo reticularis |
|
|
Diagnosis of Polyarteritis Nodosum
|
1. dx is made by biopsy of involved tissue or mesenteric angiography
2. ESR is usually elevated, and p-ANCA can be present 3. Test for fecal occult blood |
|
|
Prognosis and Treatment of Wegener's granulomatosis
|

1. The prognosis is poor, but improved to a limited extent with treatment. Start with corticosteroids. If PAN is severe, add cyclophosphamide
|
|
|
Behcet's syndrome
1. definition, cause 2. clinical features 3. diagnosis 4. treatment |

1. An autoimmune multisystem vasculitic disease, cause is unknown
2. Clinical features: recurrent oral and genital ulcerations (usually painful), arthritis (knees and ankles most commonly), eye involvement (uveitis, optic neuritis, iritis, conjuctivitis), CNS involvement (meningoencephalitis, itracranial HTN), fever and weight loss 3. Diagnosis is made by biopsy of the involved tissue (lab tests are not helpful) 4. Treatment is steroids, which are helpful |
|
|
buerger's Disease (thromboangiitis obliterans)
|

- occurs mostly in young men who smoke cigarettes
- acute inflammation of small and medium-sized arteries and veins, affecting arms and legs - may lead to gangrene - clinical features include ischemic claudication, cold, cyanotic and painful distal extremities, paresthesia of distal extremities and ulceration of digits - smoking cessation if mandatory to reduce progression - tissues can auto amputate secondary to infarction |
|
|
Hypersensitivity Vasculitis
|

- small vessel vasculitis that is a hypersensitivity reaction in response to a drug (penicillin, sulfa drugs), infection or other stimulus
- skin is predominantly involved - palpable purpura, macules or vesicles (common on lower extremities) can occur. Lesions can be painful - constitutional symptoms (fever, weight loss, fatigue) may be present - biopsy is required for diagnosis - prognosis is very good. Spontaneous remissions are common - withdrawal of the offending agents and steroids are the treatments of choice |

