![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
140 Cards in this Set
- Front
- Back
|
Sarcoidosis
1. definition 2. What population does it mostly affect 3. prognosis |
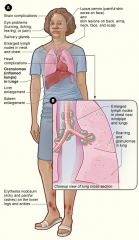
1. a chronic granulomatous disease characterized by non-caseating granulomas, involving multiple organ systems-- lungs are almost always affected
2. African Americans, especially women, usually <40 yo 3. usually good |
|
|
Symptoms of Sarcoidosis
|
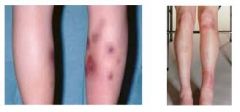
a. constitutional sx- malaise, fever, anorexia, weight loss
b. dry cough, dyspnea (esp with exercise) c. skin (25%)- erythema nodosum, plaques, subQ nodules, maculopapular eruptions d. eyes (25%)- anterior uveitis (75%), posterior uveitis (25%), conjuctivitis e.heart (5%) -- arrhythmias, condution abn (heart block etc), sudden death f. MSK- arthralgias, arthritis, bone lesions g. nervous system- CNVII (bell's palsy), optic nerve dysfunction, papilledema, peripheral neuropathy |
|
|
Diagnosis of Sarcoidosis
1. radiographic findings 2. lab findings 3. histiologic findings |
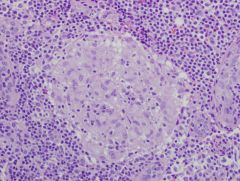
Based on clinical, radiological, and histiological findings
1. CXR- BILATERAL HILAR ADENOPATHY is hallmark, but not specific and only seen in 50% of cases-- 4 stages depending on what you see on CXR- stge 1 has no parenchymal infiltrates 2. Increased Angiotensin Converting Enzyme (ACE) levels in 50-80%--> not sensitive or specific, hypercalciuria and hypercalcemia are common 3. definitive dx requires transbronchial bx-- must see non-caseating granuloma (can be seen in other diseases) 4. PFTs- decreased lung volumes (VC and TLC), dec DLco, decreased FEV1/FVC |
|
|
Treatment of Sarcoidosis and indications for tx
|
- most cases resolve or significantly improve spontaneously within 2 years and do NOT require treatment
- systemic corticosteroids are the tx of choice- indications for treatment are unclear- but if symptomatic, lung disease, cardiac disease or severe skin or eye involvement then treat |
|
|
Histiocytosis X
1. definition 2. what patients is this typically seen in? 3. variants |
1. Chronic Interstitial pneumonia caused by abnormal proliferation of histiocytes
2. 90% are cigarette smokers 3. variants are eosinophilic granuloma, Letterer-Siwe disease, Hans-Schuller-Christian syndrome |
|
|
Histiocytosis X
1. common findings 2. other manifestations 3. CXR and CT appearance 4. prognosis 5. treatment |
1. dyspnea and nonproductive cough
2. spontaneous pneumothorax, lytic bone lesions, diabetes insipidus (excessive thirst and huge amounts of dilute urine) 3. CXR - honeycomb appearance, CT- cystic lesions 4. prognosis is highly variable 5. corticosteriods are sometimes effective, lung transplant may be necessary |
|
|
Wegener's granulomatosis
1. general characteristics- how common, histology? 2. what is affected? 3. clinical manifestations? 4. gold standard for diagnosis? 5. treatment |

1. rare disease of unknown origin characterized by necrotizing granulomatous vasculitis
2. affects vessels of lungs, kidneys, upper airway, and sometimes other organs 3. upper and lower respiratory infections, glomerulonephritis, and pulmonary nodules 4. gold standard for dx = tissue bx, but if patient has c-ANCA antibodies then probability of dz is high 5. tx- usually immunosuppression and glucocorticoids |
|
|
Churg-Strauss Syndrome
1. definition 2. typical presentation 3. Labs 4. Treatment |

1. granulomatous vasculitis seen in patients with asthma (allergic vasculitis)
2. pulmonary infiltrates, rash, eosinophilia- systemic vasculitis may result in skin, muscle and nerve lesions 3. eosinophilia, p-ANCA 4. glucocorticoids |
|

|
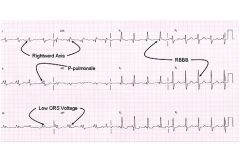
Sarcoidosis- bilateral hilar adenopathy
|
|
|
Coal worker's pneumoconiosis
1. definition 2. presentation 3. cause |
1. accumulation of dust in the lungs and the tissue reaction to its presence
- most of the time there is no significant respiratory disability - some patients may develop complicated pneumoconiosis, which is characterized by pulmonary fibrosis - causes- inhalation of coal dust which contains carbon and silica |
|
|
Asbestosis
1. characteristics 2. disease course 3. what are patients with this disease at increased risk for? 4. sx and physical exam findings 5. diagnosis 6. CXR 7. treatment |

1. diffuse interstitial fibrosis of the lung caused by inhalation of asbestos- predilection for the lower lobes
2. develops insidiously many years after exposure (>15-20 yrs) 3. increased risk for bronchogenic carcinoma (smoking is synergistic), and malignant mesothelioma 4. sx and physical findings are non-specific, restrictive lung disease 5. diagnosis is based on clinical findings and history of exposure to asbestos 6. CXR shows hazy infiltrates with bilateral linear opacities - PLEURAL PLAQUES 7. no specific tx |
|
|
Silicosis
1. definition 2. clinical course 3. associated with risk of what? 4. sources 5. symptoms 6. treatment |
1. restrictive lung disease with localized AND nodular peribronchial fibrosis - upper lobes most common
2. can be acute- massive exposure leading to rapid onset and death or chronic- symptoms years after exposure- up to 15 yrs or longer 3. associated with increased risk of TB 4. sources- mining, stone cutting, glass manufacturing 5. exertional dyspnea, cough productive of sputum can be seen 6. removal from exposure to silica |
|
|
Berylliosis
1. features 2. clinical course 3. dx 4. tx |
- like silicosis- has acute and chronic forms
- acute disease is a diffuse pneumonitis caused by massive exposure to beryllium, chronic disease is similar to sarcoidosis- granulomas, skin lesions, and hypercalcemia - dx -beryllium lymphocyte proliferation test - tx: glucocorticoids for both acute and chronic disease |
|
|
Hypersensitivity Pneumonitis (extrinsic allergic alveolitis)
1. definition 2. causes 3. dx 4. acute vs chronic forms 5. treatment |
1. inhalation of antigenic agent to the alveolar level induces immune-mediated pneumonitis- chronic exposure may lead to restrictive lung disease
2. variety of organic dusts and chemicals- farmer's lung (moldy hay), bird-breeder's lung (avian droppings), air conditioner etc-- often caused by spores of thermophilic actinomycetes 3. increased IgG and IgA to the inhaled antigen- some may have these antibodies with no disease 4. acute- flu like illness- fever, chills, cough, dyspnea, CXR- shows pulmonary infiltrates 5. chronic- insidious and difficult to diagnose 6. treatment- removal of offending agent, glucocorticoids |
|
|
Goodpasture's Disease
1. cause 2. clinical features 3. complications 4. diagnosis 5. prognosis 6. treatment |
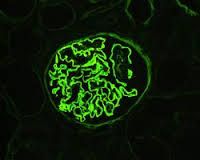
1. autoimmune disease caused by IgG antibodies directed against glomerlar and alveolar basement membranes (type II hypersensitivity reaction)
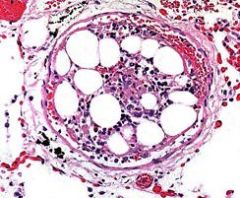
2. hemorrhagic pneumonitis and glomerulonephritis-- hemoptysis, dyspnea, hematuria 3. renal failure as result of proliferative glomerulonephritis 4. dx by tissue biopsy- serologic evidence of antiglomerular basement membrane antibodies 5. prognosis is poor 6. treatment is plasmapheresis, cyclophosphamide, and corticosteroids Picture = immunofluorescence - anti-glomerulobasement membrane antibodies-- ribbon-like |
|
|
Pulmonary Alveolar Proteinosis
|
- rare condition caused by accumulation of surfactant-like protein and phospholipids in the alveoli
- usually presents with dry cough, dyspnea, hypoxia, and rales - CXR typically has ground glass appearance with bilateral alveolar infiltrates that resembles the shape of a bat - lung biopsy needed for definitive diagnosis - lung lavage is the mainstay of treatment, but granulocyte-colony stimulating factor is a new tx - patients are at increased risk for infection so steroids should NOT be given |
|
|
Idiopathic pulmonary fibrosis
1. cause 2. who is most commonly affected? 3. presentation 4. clinical course |
1. etiology is unknown but it is more common in men and smokers
3. gradual onset of progressive dyspnea with nonproductive cough 4. devastating and unrelenting, however prognosis is variable- mean survival is 3-7 yrs after first diagnosis |
|
|
Diagnosis of idiopathic pulmonary fibrosis (IPF)
|

1. CXR- ground glass or honeycombed appearance, but may be normal
2. definitive diagnosis requires open lung biopsy, but even this may show non-specific findings 3. other causes of ILD must be excluded |
|
|
Treatment for idiopathic pulmonary fibrosis
|

1. No effective treatment is available- the majority of patients (>70%) do not improve with therapy and experience progressive and gradual respiratory failure... however the following may be of some benefit
- supplemental oxygen - corticosteroids with our without cyclophosphamide- taper after 1 year of use - lung transplant |
|
|
Cryptogenic Organizing Pneumonitis (COP)
1. definition 2. associations 3. symptoms 4. CXR 5. efficacy of abx? 6. treatment 7. relapse? |
1. inflammatory lung disease with similar clinical and radiographic features to infectious pneumonia
2. associated with many entitities-- viral infections, medications, connective tissue disease-- but MOST are idiopathic 3. features- cough, dyspnea, and flu-like symptoms 4. CXR- bilateral patchy infiltrates 5. antibiotics are ineffective 6. Spontaneous recovery may occur- but corticosteroid are used most commonly (>60% recover) 7. Relapse may occur after cessation of steroids - necessitating resumption of steroids |
|
|
Radiation pneumonitis
1. definition 2. what determines morbidity and mortality? 3. acute vs chronic form 4. clinical features 5. CXR 6. CT 7. treatment |

1. interstitial pulmonary inflammation -- occurs in 5-15% of patients that undergo thoracic radiation for lung cancer, breast cancer, lymphoma, or thymoma
2. mortality and morbidity are related to the irradiated lung volume, dose, patient status and concurrent chemotherapy 3. acute form- occurs 1-6 months after irradiation, chronic form develops 1-2 years later-- characterized by alveolar thickening and pulmonary fibrosis 4. low grade fever, cough, chest fullness, dyspnea, pleuritic chest pain, hemoptysis, acute respiratory distress 5. CXR is usually normal 6. CT is best study- diffuse infiltrates (hallmakr), ground glass density, patchy/homogenous consolidation, pleural/pericardial pleural effusions-- excellent for detecting recurrent cancer in irradiated area 7. treatment of choice = corticosteroids- prophylaxis is not helpful |
|
|
Acute Respiratory Failure
- definition-- cutoffs for hypoxia and hypercapnia |
- results when there is inadequte oxygenation of blood or ventilation (elimination of CO2) or both
- Hypoxia (PaO2 < 60 mmHg and PaCO2 > 50 mmHg) - Hypercapnia- partial pressure of CO2- > 50 mmHg |
|
|
Potential causes of respiratory failure by system
|
1. CNS- brain or spinal cord depression or insult- drug overdose, stroke, trauma
2. neuromuscular disease- myasthenia gravis, polio, guillan barre, ALS (amyotrophic lateral sclerosis- lou guerigs) 3. upper airway- obstruction due to a number of causes including stenosis, spasm and paralysis 4. thorax and pleura- mechanical restriction due to kyphoscoliosis, flail chest-broken rib, hemothorax 5. cardiovascular system and blood- CHF, valvular diseases, PE, anemia 6. lower airways and alveoli- asthma, COPD, pneumonia, ARDS |
|
|
Two major types of acute respiratory failure
|
there is often overlap
1. hypoxemic respiratory failure 2. hypercarbic respiratory failure |
|
|
hypoxemic respiratory failure
- PaO2 and PaCO2 - causes - pathophysiology |
- low PaO2 with a PaCO2 that is either low or normal-- present with oxygen sat less than 90% despite FiO2- >0.6 (fraction of inspired oxygen)
- causes include disease processes the involve the lung itself - ARDS, severe pneumonia, pulmonary edema - V/Q (ventilation to perfusion) mismatch and intrapulmonary shunting are the major pathophysiologic mechanisms |
|
|
Hypercarbic respiratory failure
- pathophysiology - respiratory causes - non pulmonic causes |
VENTILATORY respiratory failure
- decrease in minute ventilation or an increase in physiologic dead space leads to CO2 retention and eventually results in hypoxemia - may be caused by underlying lung disease (COPD, asthma, CF, severe bronchitis) - may occur in patients with no underlying lung disease who have impaired ventilation due to neuromuscular disease, CNS depression, mechanical restriction of lung inflation (extreme obesity), or any cause of respiratory fatiure (prolonged hyperventilation in DKA) |
|
|
Ventilation vs oxygenation
|
Ventilation is monitored by PaCO2- to decrease paCO2 you must either increase respiratory rate or increase tidal volume-- minute ventilation = RR x VT
Oxygenation is monitored by O2 saturation and PaO2- to decrease PaO2 in a ventilated patient you must decrease FiO2 or PEEP (positive end-expiratory pressure) |
|
|
Young patient presents with constitutional symptoms, respiratory complaints, erythema nodosum, blurred vision. On CXR she is found to have bilateral hilar adenopathy. What is the most likely diagnosis?
|
Sarcoidosis
|
|
|
what type of respiratory failure does a V/Q mismatch typically produce?
|
Hypoxia without hypercapnia- PaCO2 levels are usually low to normal
- most common mechanism of hypoxemia (especially in chronic lung disease) - responsive to supplemental oxygen |
|
|
Intrapulmonary shunting
1. definition 2. causes |
little or no ventilation in perfused areas- due to collapsed or fluid-filled alveoli- venous blood is shunted into the arterial circulation without being oxygenated
- causes of shunts- atelectasis or fluid buildup in the alveoli (pneumonia or pulmonary edema), direct right to left intracardiac blood flow in congenital heart disease - hypoxia due to a shunt is NOT responsive to supplemental oxygen-- the area is not ventilated so it does not matter how much oxygen is getting into the lungs-- it won't cross into the blood |
|
|
What type of respiratory failure does a diffusion impairment lead to?
|
hypoxemic respiratory failure-- oxygen cannot get into the blood-- but the CO2 can get out--> no hypercapnia.
|
|
|
clinical features/symptoms of acute respiratory failure
|
1. dyspnea- first symptom
2. cough may or may not be present depending on the underlying cause |
|
|
clinical features/physical exam signs of acute respiratory failure
|
- inability to speak in full sentences, use of accessory muscles of respiration
- tachypnea, tachycardia - cyanosis - impaired mentation (due to fatigue or hypercapnia- or if cause of respiratory failure is CNS depression) |
|
|
Diagnosis of Acute Respiratory Failure
|
1. ABG - arterial blood gas- analysis- may confirm diagnosis and help determine the severity of the condition- should be obtained in most cases of respiratory failure
- hypoxemia- mechanisms include V/Q mismatch, intrapulmonary shunting or hypoventilation -hypercapnia- caused by hypoventilation - secondary to a variety of causes - arterial pH- respiratory acidosis occurs when hypercapnia is present-- however if respiratory failure is chronic- renal compensation occurs and acidosis is less severe - CXR or CT chest - CBC and metabolic panel - If cardiogenic pulmonary edema is suspected--> cardiac enzymes-- CK-MB, troponins + ECG |
|
|
Treatment of acute respiratory failure
|
1. treat the underlying disorder- bronchodilators, corticosteroid, antibiotics etc
2. supplemental O2- if the patient is hypoxemic-- remember this will not help if the patient has an intrapulmonary shunt 3. Apply NPPV- non-invasive positive pressure ventilation via CPAP or BIPAP ONLY for conscious patients with possible impending respiratory failure-- if the patient cannot breathe on his or her own--> intubate 4. intubation and mechanical ventilation may be needed in both types of respiratory failure |
|
|
Supplemental oxygen use in hypoxemic respiratory failure
|
use the lowest concentration of oxygen that provides sufficient oxygenation to avoid oxygen toxicity due to free radical production
|
|
|
supplemental oxygen use in hypercarbic respiratory failure
|
- traditionally, it has been taught that high concentractions of oxygen can cause retention of CO2- especially in patients with COPD because hypoxia drives breathing so when a patient is no longer hypoxic, hypoventilation can result and hypercapnia can worsen-- causing respiratory acidosis-- however the validity of this theory is now in question
|
|
|
Techniques to improve tissue oxygenation
|
- increase Fio2- fraction of inspired oxygen
- increase PEEP (positive end expiratory pressure)-- keep airways open - extend inspiratory time fraction - decubitus, upright or prone positioning bronchodilation - improve oxygen delivery - increase cardiac output, increase hemoglobin - decrease oxygen requirements - decrease work of breathing, fever, agitation - remove pulmonary vasodilators such as nitroprusside |
|
|
Oxygen delivery system for Low Flow
|
- nasal cannula (1-6 L/min) , FiO2 up to 40%- easy to use and comfortable
- simple face mask (1-10 L/min)-, FiO2 40-60%- can deliver higher flow rates than nasal cannula |
|
|
Oxygen Delivery Systems for High Flow needs
|
Venturi Mask- 4-10 L/mn, up to 50% FiO2 but can determine exact FiO2 to deliver- preferred in CO2 retainers because one can precisely control oxygenation
Non-rebreathing Mask- up to 15 L/min- variable FiO2 up to 70-80%, can achieve higher FiO2 at lower flow rates |
|
|
What is the Alveolar-arterial oxygen gradient (A-a gradient) like in hypoxemia due to hypoventilation?
|
Normal-- all the oxygen that is getting into the lungs is getting into the blood-- there just is not enough
- A-a gradient is high in most other causes of hypoxemia |
|
|
ARDS (Adult Respiratory Distress Syndrome)
1. definition 2. mechanism |
1. diffuse inflammatory process that is not necessarily infectious involving both lungs. Due to neutrophil activation in the systemic or pulmonary circulations
2. Not a primary disease but rather a disorder that arises due to other conditions that cause a widespread inflammatory process. It is a CLINICAL DIAGNOSIS |
|
|
Pathophysiology of ARDS
|
- Massive intrapulmonary shunting of blood is key pathologic event in ARDS- severe hypoxemia with NO significant improvement on 100% oxygen
- shunting is due to widespread atelectasis, collapse of the alveoli and surfactant dysfunction - interstitial edema and alveolar collapse are due to increase in lung fluid, which leads to stiff lungs, an increase in alveolar=arterial oxygen difference (A-a gradient) and ineffective gas exchange - Note: the effects of the increase in pulmonary fluid are identical to those seen in cardiogenic pulmonary edema, but the cause is different: An increase in alveolar capillary permeability causes ARDS, whereas congestive hydrostatic forces cause cardiogenic pulmonary edema - Decreased pulmonary compliance-- leads to increased work of bleeding - increased dead space-- secondary to obstruction and destruction of pulmonary capillary bed - Low Vital Capacity, Low FRC |
|
|
Causes of ARDS
|
1. Sepsis is the most common risk factor- can be secondary to a variety of infections (e.g. pneumonia, urosepsis, wound infections)
2. aspiration of gastric contents 3. Severe trauma, fractures (e.g. femur, pelvis), acute pancreatitis, multiple or massive transfusions, near-drowning 4. drug overdose, toxic inhalations 5. Intracranial HTN 6. Cardiopulmonary bypass |
|
|
Clinical features of ARDS
|
1. dyspnea, tachypnea, and tachycardia due to increased work of breathing
2. progressive hypoxemia- not responsive to supplemental oxygen (ration of PaO2 to FiO2 < 200) 3. Patients are difficult to ventilate because of high peak airway pressures due to stiff, noncompliant lungs |
|
|
Diagnosis of ARDS
1. CXR findings 2. ABG findings 3. Pulmonary artery catheter 4. bronchoscopy- when used? What do you send the lavage fluids for? |

1. CXR - shows diffuse bilateral pulmonary infiltrates- there i variable correlation between findings on CSR and severity of hypoxemia or clinical response. Diuresis improves and volume overload worsens the pulmonary infiltrates. CXR improvement follows clinical improvement by 1-2 weeks or more
2. ABG- Hypoxemia (PaO2 < 60 mmHg), Initially, respiratory alkalosis (PaCO2 < 40 mmHg) is present which gives way to respiratory acidsosis as the work of breathing increases and the paCO2 increases. if the patient is septic ,metabolic acidosis may be present with or without respiratory compensation 3. pulmonary artery catheter- enables determination of pulmonary capillary wedge pressure (PCWP- LA Filling Pressure)- an indirect marker of intravascular volume status. PCWP is the most useful parameter in differentiating ARDS from cardiogenic pulmonary edema. If PCWP is low (<18 mmHg), ARDS is more likely, whereas if PCWP is high (>18mmHg) then cardiogenic pulmonary edema is more likely 4. bronchoscopy with bronchoalveolar lavage- this may be considered if patient is acutely ill and infection is suspected. Fluid collected can be cultured and analyzed for cell differential, cytology, gram stain, and silver stain |
|
|
Treatment of ARDS
|
1. Oxygenation- try to keep O2 saturation > 90%
2. mechanical ventilation with PEEP is usually required. It serves to increase lung volume by opening collapsed alveoli and decreasing shuting 3. Fluid management- volume overload should be avoided. A low-normal intravascular volume is preferred, the goal should be a PCWP of 12-15 mmHg. Vasopressors may be needed to maintain BP. On the other hand, patients with sepsis have high fluid requirements, so determining in the appropriate fluid management may be difficult 4. Treat the underlying cause (e.g. infection) 5. Do not forget to address the patient's nutritional needs. Tube feedings are preferred over parenteral nutrition-- always use the gut when you can |
|
|
Complications of ARDS
|
1. Permanent lung injury- resulting in lung scarring or honeycomb lung
2. complications associated with mechanical ventilation- barotrauma secondary to high pressure mechanical ventilation possibly causing a pneumothorax or pneumomediastinum. Nosocomial pneumonia 3. Line-associated infections- central lines and pulmonary artery catheters (line infection sepsis), urinary catheters (UTI), and nasal tubes (sinus infection) 4. renal failure- may be due to nephrotoxic medication, sepsis with hypotension, or underlying disease 5. Ileus, stress ulcers 6. Multiple organ failure 7. Critical illness myopathy |
|
|
Mechanical Ventilation- what are the 2 major goals of mech vent?
|
1. maintain alveolar ventilation
2. correct hypoxemia |
|
|
When should patients be initiated on mechanical ventilation?
|
The decision to initiate mechanical ventilation should be a clinical one. Generally, patients with the following require mechanical ventilation:
1. Significant respiratory distress (e.g. high RR) or respiratory arrest 2. Impaired or reduced level of consciousness with inability to protect airway (look for absent gag or cough reflex) 3. Metabolic acidosis (if the patient is unable compensate with adequate hyperventilation to blow off CO2) 4. respiratory muscle fatigue 5. Significant hypoxemia (paO2 <70 mmHg) or hypercapnia (PaCO2 > 50 mmHg), respiratory acidosis (pH < 7.2) with hypercapnia - ABGs are used to assess response to initiation of mech vent. Acceptable ranges of gas values include a PaO2 of 50 to 60 with PaCO2 of 40 to 50, and pH between 7.35 and 7.50. |
|
|
General principles of mechanical ventilation
|
1. Initial settings should rest the respiratory muscles
2. The goal is to reduce the likelihood of barotraumas (high static airway pressures, overinflation) and atelectasis (low static airway pressures, underinflation) 3. A volume-cycled ventilator is most commonly used |
|
|
Ventilator Settings- Assisted Controlled (AC) Ventilation
|
1. Assisted controlled (AC) Ventilation - this is the initial mode used in most patients with respiratory failure. Guarantees a "backup" minute ventilation that has been preset. The ventilator delivers a breath (of a predetermined tidal volume) when the patient initiates a breath. If the patient does not initiate a breath, the ventilator takes control and delivers a breath at a predetermined rate. In other words, the patient can go over the determined rate, but not under it. And every breath over the determined rate delivers the same predetermined tidal volume.. All breaths are delivered by the ventilator (in contrast to intermittent mandatory ventilation).
|
|
|
Ventilator Settings - synchronous Intermittent Mandatory Ventilation (SIMV)
|
- patients can breathe on their own above the mandatory rate without help from the ventilator (i.e. tidal volume of these extra breath is NOT determined by the ventilator, as it is in the assisted control mode)
- when the patient breathes spontaneously, there is no present volume of breath that is triggered, but he or she still gets the guaranteed predetermined rate - this method delivers the mandatory breath in synchrony with the patient's initiated breath so that the two do not overlap, which is possible with the intermittent mandatory ventilation alone - if no spontaneous breath is initiated by the patient, the predetermined mandatory breath is delivered by the ventilator - this is the appropriate mode for both support of ventilation and weaning |
|
|
Continuous Positive Airway Pressure (CPAP)
|
- Positive pressure (0-20 cm H2O) is delivered continuously (during expiration and inspiration) by the ventilator, but no volume breaths are delivered (patient breathes on his or her own)
- the only parameters to set are PEEP and pressure support - If the patient is being weaned, one can use CPAP to assess whether the patient is ready to be extubated |
|
|
Pressure-Support Ventilation (PSV)
|
- This is mostly used during weaning trials. Pressure is delivered with an initiated breath to assist breathing (pressure is not continuous-- only responds to initiated breath)
- It enhances respiratory efforts made by the patient - PEEP may be added |
|
|
Key Ventilator Parameters
1. Minute Ventilation -components 2. FiO2 3. Inspiratory:Expiratory (I:E ratio) 4. PEEP |
1. Minute Ventilation (RR x tidal volume)- this should be adjusted to achieve the patient's baseline PaCO2. An initial tidal volume of 8-10 mL/kg is appropriate in most cases (lower tidal volumes are recommended for patient with ARDS and COPD). A rate of 10-12 breaths/min is appropriate
2. FiO2- fraction of inspired oxygen- the initial FiO2 should be 100% and should be quickly titrated down and use the lowest possible FiO2 to maintain a PaO2 of 50 to 60 or higher (or saturation > 90%) to avoid oxygen toxicity. FiO2 of less than 60% is generally safe. If an FiO2 of 0.5 does not result in adequate PaO2 add either PEEP or CPAP, both of which allow one to reduce FiO2 (i.e. to support PaO2 at a lower FiO2) 3. I:E ratio- the duration of time allotted to inspiration compared with the time allotted to expiration in one delivered breath. Remember that the duration of each breath is determined by the set RR. Therefore, increasing the time spent inspiration will proportionately decrease the time spent in expiration and vice versa. 1:2 is the usual ratio used. 4. PEEP- positive pressure maintained at the end of passive exhalation- keeps alveoli open. 2.5-10 cm H2) is appropriate initial setting. Can be added to any of the modes of ventilation, used mostly in patients with hypoxemic respiratory failure (ARDS). It allows for increased lung compliance and oxygenation (improves gas exchange), Prevents alveolar collapse and atelectasis. Side Effects: barotrauma (injury to the airway = pneumothorax), Low cardiac output due to decreased venous return, especially in the setting of hypovolemia.-- PEEP- like any form of positive intrathoracic pressure, lowers venous return and increases pulmonary vascular resistance |
|
|
Complications of Mechanical Ventilation
|
1. Anxiety, agitation, discomfort- sedation is important, benzodiazepines are the preferred agents. Other options are opiods or induction agents such propofol. use opiods for analgesia.
2. Difficulty with tracheal secretions-- suction on a regular basis 3. Nosocomial pneumonia (especially if intubated for more than 72 hours) 4. Accidental extubation 5. Barotrauma- caused by high airway pressures 6. Oxygen toxicity- when FiO2 of >0.6 is required for prolonged period (2-3 days). 7. Hypotension- positive pressure ventilation results in creased intrathoracic pressures, leading to decreased venous return 8. trachelomalacia- softening of the tracheal cartilage- due to the prolonged presence of an endotracheal tube (ET) 9. Laryngeal damage during intubation 10. Gastrointestinal effects- stress ulcers and cholestasis- increased risk in mechanically ventilated patients. |
|
|
What patients have the highest risk of developing ARDS?
|
Patients with sepsis or septic shock
|
|
|
classic clinic criteria for diagnosing ARDS
|
1. hypoxemia- that is refractory to oxygen therapy: ratio of PaO2/FiO2 </= 200
2. bilateral diffuse pulmonary infiltrates on CXR 3. No evidence of CHF: PCWP </= 18mmHg |
|
|
After placing an ET (endotracheal tube) what should you always do?
|
Confirm correct placement by listening for bilateral breath sounds and checking a postintubation CXR
- On CXR- the tip of the ET tube should be approximately 3-5 cm above the carina |
|
|
Parameters to consider in extubation or weaning from a ventilator- the more criteria that are met, the more likely that extubation will be tolerated
|
- whether the patient has an adequate respiratory drive
- intact cough (when suctioning secretions) - PaO2 > 75, PaCO2< 45 - O2 saturation of > 90% with PEEP of 5 cm H20 or less and FiO2 < 40% to 50% - Tidal volume > 5 mL/kg - RR < 30 breath per min - Vital Capacity > 10 to 15 mL/kg - Negative inspiratory pressure <-20 cm H20 or more |
|
|
When should a tracheostomy be performed?
|
When a patient is ventilator dependent for 2 or more weeks, a tracheostomy should be done to prevent tracheomalacia
|
|
|
PEEP vs CPAP
|
PEEP is positive end expiratory pressure that is applied during mechanical ventilation, whereas CPAP is positive pressure during spontaneous breathing. Both serve to increase the PaO2 at a constant FiO2 (by lowering intrapulmonary shunting and V/Q mismatch)
|
|
|
What things should you always remember when assessing a patient with ARDS? (4)
|
1. Physical findings are usually non-specific
2. Because the patient is usually intubated and on a ventilator, decreased unilateral breath sounds may be due to the endotracheal tube being in the right main bronchus or possibly a pneumothorax 3. Look for potential sources of sepsis and check for any signs of infection: acute abdomen, IV lines, wounds, decubiti etc 4. Keep in mind that cardiogenic pulmonary edema has to be distinguished from ARDS- look for signs of volume overload, CHF, JVD, edema, and hepatomegaly |
|
|
Pulmonary Hypertension definition
|
1. Mean pulmonary arterial pressure > 25 mmHg at rest or 30 mmHg during exercise
|
|
|
Classifications of causes of pulmonary hypertension from a physiologic standpoint
|
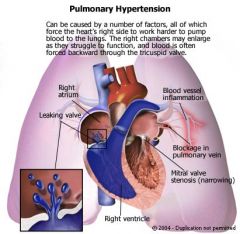
1. passive type- resistance to pulmonary venous drainage, no active disease in the pulmonary vascular bed ( passive reflection of a process further down) - e.g. mitral stenosis, LV failure, atrial myxoma, pulmonary veno-occlusive disease
2. hyperkinetic type- caused by high pulmonary blood flow (left-to-right shunt)- ventricular septal defect, atrial septal defect, PDA 3. Obstructive type- resistance to flow through large pulmonary arteries (E.g. PE, stenosis of pulmonary artery) 4. Obliterative type- resistance to flow through the small pulmonary arterioles due to some parenchymal inflammation that leads to fibrosis (e.d. primary pulmonary hypertension, collagen vascular disease, CREST syndrome) 5. Vasoconstrictive type- resistance to flow due to hypoxia-induced vasoconstriction (e.g. anything that causes chronic hypoxemia-- COPD, OSA etc) 6. Increased intrathoracic pressure- the increased intrathoracic pressure is transmitted to the pulmonary vasculature (e.g. mechanical ventilation with PEEP, COPD). 7. Increased blood viscosity (e.g. polycythemia vera) |
|
|
Classification of causes of pulmonary hypertension from an anatomic standpoint (2)
|
1. Postcapillary causes - associated with diseases of the left side of the left side of the heart that increase pulmonary venous pressures- ex- mitral stenosis, left ventricular dysfunction, atrial myxoma, constrictive pericarditis, pulmonary veno-occlusive disease)
2. Mixed capillary and pre-capillary causes associated with diseases of lung parenchyma or pulmonary vessels-- all obstructive and parenchymal diseases (e.g. COPD, ILD, PE, Primary pulmonary hypertension, kyphoscoliosis) |
|
|
Symptoms of pulmonary hypertension
|
1. Dyspnea on exertion
2. fatigue 3. chest pain 4. syncope- exertional (with severe disease) |
|
|
Signs of pulmonary hypertension
|
1. Loud pulmonic component of the second heart sounds (P2) and subtle lift of sternum- sign of RV dilitation-- these may be the only findings and the patient may have devastating disease
2. When RV failure occurs-- JVD, hepatomegaly, ascites, and peripheral edema |
|
|
Diagnosis of pulmonary hypertension
1. ECG 2. Echo 3. Right heart catheterization |
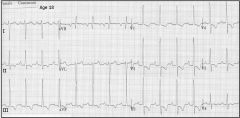
1. ECG- often suggest RV hypertrophy-specifically right axis deviation and right atrial abnormality
2. Echo - dilated pulmonary artery, dilatation/hypertrophy of RA and RV, abnormal movement of the IV septum-- due to increase right ventricular volume 3. right heart catherization- increased pulmonary artery pressure |
|
|
Treatment of pulmonary hypertension
|
No specific treatment plan because it depends largely on the cause
|
|
|
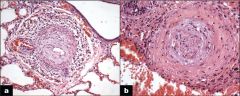
Primary Pulmonary Hypertension
1. definition 2. pathophysiology 3. Cause and who is usually affects? 4. prognosis and course of disease |
1. Pulmonary hypertension in the absence of diseases of the heart or lung-- DX OF EXCLUSION
2. An abnormal increase in the pulmonary ateriolar resistance leads to thickening of the pulmonary arterioral walls. This worsens the pulmonary hypertension, which in turn causes further wall thickening (due to increases wall stress, this leading to a vicious cycle 3. the cause is unknown and it usually affects young to middle aged women 4. prognosis is poor- mean survival is 2-3 years from the time of diagnosis. By the time a patient seeks medical attention, the disease is often irreversible. |
|
|
Clinical features of primary pulmonary hypertension
|
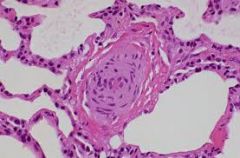
1. signs and symptoms similar to those from pulmonary HTN from another cause (dyspnea, CP, fatigue, syncope, RVH, edema, ascites, JVD, hepatomegaly)
2. exertional syncope is particularly common and is found in up to 50% of cases |
|
|
Diagnosis of Primary Pulmonary Hypertension
|
1. Cardiac catheterization establishes the diagnosis
2. CXR shows enlarged central pulmonary arteries, enlarged RV, and clear lung fields 3. PFTs show a restrictive pattern 4. ECG shows right axis deviation and RVH |
|
|
Treatment of Primary Pulmonary Hypertension
|
1. pulmonary vasodilators such IV prostacyclins (epoprostenol) and calcium channel blockers can lower pulmonary vascular resistance.
- perform a vasodilator trial - using inhaled nitric oxide, IV adenosine, or oral CCB under hemodynamic monitoring to predict response before initiating treatment. -Sildenafil (Viagra) may also be useful as a vasodilator 2. Anticoagulation with warfarin is generally recommended (keep INR around 2.0) due to venous stasis, physical inactivity, and increased risk of microvascular thrombosis 3. lung transplantation may be an option in qualified patients |
|
|
Cor pulmonale
1. definition |
1. Right ventricular hypertrophy with eventual RV failure resulting from pulmonary hypertension, secondary to pulmonary disease
2. this does NOT encompass any causes of pulmonary HTN due to left-sided heart disease (such as MS, or left to right shunts) |
|
|
Causes of cor pulmonale
1. most common 2. others |
1. most commonly due to COPD
2. other causes- recurrent PE, ILD, asthma, CF, sleep apnea, and pneumoconioses |
|
|
Clinical features of cor pulmonale
|
1. decrease in exercise tolerance
2. cyanosis and digital clubbing 3. signs of RV failure-- hepatomegaly, ascites, JVD, edema 4. parasternal lift 5. polycythemia is often present if COPD is the cause (secondary to chronic hypoxemia) |
|
|
Diagnosis of cor pulmonale
1. CXR 2. ECG 3. Echo |
1. CXR- enlargement of the RA, RV, and pulmonary arteries
2. ECG- right axis deviation, P pulmonale (peaked P waves), RVH 3. Echo- RV dilitation, but normal LV size and function-- useful in excluding LV dysfunction |
|
|
How do you determine the cause of pulmonary hypertension?
|
1. Perform a series of tests (CXR, PFTs, ABGs, serology, echo and cardiac cath). These tests will give you enough information to recognize heart or lung disease as the causes
2. If the cause is not revealed - neither heart nor lung cause, then obtain a V/Q scan- this indicates either PE or PPH-- PPH is a diagnosis of exclusion |
|
|
What is the right-sided heart disease that is pretty much equivalent to left-sided heart disease due to systemic hypertension?
|
Cor pulmonale-- secondary to pulmonary hypertension
|
|
|
What cardiac condition to patients with COPD often die from?
|
Right ventricular failure secondary to chronic pulmonary hypertension
|
|
|
Sources of emboli to the lungs
|
1. fat emboli- long bone fracture
2. amniotic fluid embolism- during or after delivery 3. air embolism- trauma to thorax, indwelling venous/arterial lines 4. septic embolism (IV drug use) 5. schistosomiasis- parasitic disease |
|
|
If patient with a long-bone fracture develops dyspnea, mental status changes and petechia, what diagnosis should you think of?
|
Fat embolism- respiratory failure and death can ensue rapidly
|
|
|
Pulmonary Embolism - general characteristics (pathophysiology etc)
|
A PE occurs when a thrombus in another region of the body embolizes to the pulmonary vascular tree via the RV and pulmonary artery. Blood flow distal to the embolus is obstructed.
- consider PE and DVT as a continuum of one clinical condition (venous thromboembolism)- diagnosis either PE or DVT is an indication for treatment |
|
|
Sources of emboli in PE
|
1. Lower extremity DVT- most pulmonary emboli arise from thomboses in the deep veins of the lower extremities above the knee (iliofemoral DVT)
2. pelvic venous thromboses 3. calf vein thrombi have a low incidence of embolizing to the lungs, however in many patients, these thrombi progress into the proximal veins, increasing the incidence of PE 4. Upper extremity DVT are a rare source of emboli (may be seen in IV drug users) |
|
|
Risk Factors for PE/DVT
|
1. Age >60
2. Malignancy--> hypercoaguability 3. Prior h/o PE/DVT 4. hereditary hypercoaguable states (Factor V Leiden, Protein C and S deficiency, antithrombin III deficiency) 5. prolonged immobilization, bed rest, long-distance travel 6. cardiac disease, especially CHF 7. obesity 8. nephrotic syndrome 9. major surgery- especially orthopedic e.g. pelvic surgery (immobility etc) 10. major trauma 11. pregnancy, estrogen use (OCPs) 12. smoking |
|
|
Pathophysiology of PE
|
- emboli block a portion of pulmonary vasculature, leading to increased pulmonary vascular resistance, pulmonary artery pressure, and RV pressure. If it is severe (large blockage)- acute cor pulmonale may result
- Blood flow decreases in some areas of the lung creating dead space (ventilation without perfusion). The resulting hypoxemia and hypercarbia drive respiratory effort leading to tachypnea - If the size of the dead space is large 9large PE), clinical signs are more overt (SOB and tachypnea) |
|
|
Clinical Course and Prognosis of PE
|
1. Most often PE is clinically silent. Recurrences are common, which can lead to development of chronic pulmonary hypertension and chronic cor pulmonale
2. when PE is undiagnosed, mortality approaches 30%. A significant number of cases are undiagnosed (50%) 3. When PE is diagnosed, mortality is 10% in the first 60 minutes. Of those who survive the initial event, approximately 30% of patients will die of a recurrent PE if left untreated. Most deaths are due to recurrent Pe within the first few hours of the initial PE. Treatment with anticoagulant decreases the mortality to 2% to 8%. |
|
|
Symptoms of PE
|
1. Dyspnea (73%)
2. Pleuritic Chest Pain (66%) 3. Cough (37%) 4. Hemoptysis (13%) 5. only 1/3 of patients with PE will have signs and sx of DVT 6. Syncope may be seen in large PEs |
|
|
Physical Exam Findings with PE
What is the most common finding? |
1. tachypnea (70%)
2. rales (51%) 3. tachycardia (30%) 4. S4 5. Increased P2 6. Shock with rapid circulatory collapse in massive PE 7. Other signs- low-grade fever, decreased breath sounds, dullness on percussion |
|
|
Diagnosis of PE
1. ABG 2. CXR 3. Venous Duplex US of LE |
1. ABG levels are not diagnostic- PaO2 and PaCO2 are low (PaCO2 is low due to hyperventilation) and pH is high from blowing off all the CO2-- respiratory alkalosis. The A-a gradient is usually elevated. A normal A-a gradient makes PE less likely, but cannot be relied upon for exclusion
2. CXR- usually normal. If any findings-- atelectasis, pleural effusion. The main utility is in excluding alternative diagnoses. Classic CXR signs like Hampton's hump and Westermark's sign are rarely present. 3. Venous duplex US of LE- If there is a positive result, treat with IV anticoagulation (heparin), treatment of DVT is the same as for PE. Keep in mind that with this approach, a false positive will lead to tx of some pts with no DVT or PE. A negative result is not helpful as this is the case in 50% of patients with proven PE. This test is very helpful when positive, but of little value when negative. |
|
|
Diagnosis of PE
1. V/Q scan 2. Helical CT chest with IV contrast 3. Pulmonary Angiography 4. D-Dimer assay What is the test of choice in most medical centers? What is the gold standard for diagnosis? |
1. V/Q scan- traditionally this WAS the most common test used when PE was suspected, but it has been replaced by helical CT as the initial study of choice in most medical centers unless there is C/I to CT. Is particularly useful when CXR is clear and there is no underlying cardiopulmonary disease. results-- either normal, low-probability, intermediate or high prob (see other card for interpretation of results).
2. Helical (spiral) CT chest with IV contrast- good sensitivity (90%) and specificity. can visualize very small clots (as small as 2 mm), but may miss clots in small subsegmental vessels (far periphery). Used to guide treatment in conjunction with clinical suspicion based on modified wells criteria. C/I in patients with significant renal insufficiency because of the IV contrast. 3. Pulmonary angiography- gold standard. Definitively diagnoses or excludes PE but is invasive. Contrast is injected into the pulmonary artery after percutaneous catherization of femoral vein. Consider this when noninvasive tests are equivocal and risk of anticoag is high or if the patint is hemodynamically unstable and embolectomy may be required. Angiography is rarely performed because it carries a 0.5% mortality 4. D-dimer assay- D-dimer is a specific fibrin degradation product so level can be elevated in patients with PE or DVT. It is fairly sensitive (90-98%). If results are normal and clinical suspicion is low, PE is very unlikely. Specificity is LOW- D-dimer results may also be elevated in MI, CHF, pneumonia, and post-op state. Any cause of clot or increased bleeding may elevate d-dimer level |
|
|
Interpretation of V/Q scan results
1. normal scan 2. high probability 3. Low to intermediate probability |
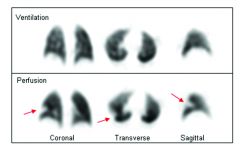
1. Normal scan- virtually rules out PE- no further testing is needed- but a scan is almost never normal in anyone
2. high probability- very high sensitivity for PE- treat with heparin 3. low to intermediate probability-- clinical suspicion determines the next step. If suspicion is high pulmonary angiography is indicated. if low then LE duplex US. If duplex positive then heparinize. if duplex negative--pulmonary angio. Basically the LE US allows you to avoid angio sometimes. |
|
|
Complications in patients with PE who survive the initial event (2)
|
1. Recurrent PE
2. Pulmonary HTN (up to 2/3 of patients) |
|
|
Reliability of signs and symptoms of PE?
|
NOT reliable. Often leads confusion and delay in treatment. However, if patient has signs and sx of PE and a DVT is found then one can make the diagnosis of PE without further testing.
|
|
|
What tests provide an adequate basis for treating PE with anticoagulation?
|
1. intraluminal filling defects in the central, subsegmental or lobular pulmonary arteries on helical CT (or high probability with a V/Q scan) and clinical suspicion.
2. DVT diagnosed with US and clinical suspicion 3. positive pulmonary angiogram (definitely proves PE) |
|
|
What tests can r/o PE?
|
1. low probability V/Q scan (or normal helical CT scan) and low clinical suspicion
2. Negative pulmonary angiography (definite) 3. Negative D-dimer and low clinical suspicion |
|
|
What if a CT- pulmonary angio is negative for PE but there is high clinical suspicion?
|
there is still a 5% chance that there is a PE-- so negative results should always be interpreted with caution in a patient with high clinical suspicion.
|
|
|
Modified Wells Criteria for suspected Acute Pulmonary Embolism
|
1. Symptoms and signs of DVT - 3.0
2. Alternative diagnosis less likely than PE - 3.0 3. Heart Rate > 100 bpm - 1.5 4. Immobilization > 3 days or surgery in the past 4 weeks - 1.5 5. Previous PE/DVT - 1.5 6. Hemoptysis - 1.0 7. Malignancy (current therapy, or in previous 6 months, or palliative) - 1.0 Calculators will tell the % chance of having a PE based on these factors/total score > 4 then PE is likely |
|
|
PE Treatment based on modified wells criteria
1. Score of <4 2. Score > 4 |
1. Score <4 then do D-dimer-- if negative then no treatment, if positive then do CT if possible
2. Score > 4 then do CT with contrast. If positive then treat. If negative then do not treat. If inconclusive or cannot be performed then do LE US. If this is positive then treat. If negative then do V/Q scan or pulmonary angio and treat if positive |
|

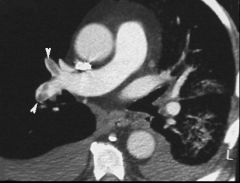
What is this ?
|
Saddle Embolism-- PE
|
|
|
Treatment of PE
|
1. Supplemental Oxygen to correct hypoxemia. Severe hypoxemia or respiratory failure requires intubation and mechanical ventilation.
2. Acute anticoagulation therapy with either unfractionated of LMWH to prevent another PE. Anticoagulation prevents further clot formation. It does NOT lyse the existing emboli or diminish the thrombus size. Start immediately on basis of clinical suspicion. DO NOT WAIT FOR STUDIES TO CONFIRM PE IF CLINICAL SUSPICION IS HIGH. Give one bolus of heparin, followed by continuous infusion for 5-10 days. The goal is get an aPTT of 1.5-2.5 times control. 3. Oral warfarin for long term treatment- start with heparin on day 1. Therapeutic INR is 2-3. Continue for 3-6 months of more, depending on risk factors. Some patients at significant risk for recurrent PE (malignancy, hypercoaguable state) may be considered for lifelong anticoagulation 4. Thrombolytic therapy- e.g. streptokinase, tPA- speeds up lysis of clots. There is no evidence that thrombolysis improves mortality rates in patients with PE. However, its use should be considered in patients with massive PE who are hemodynamically unstable (persistent hypotension), patients with evidence of Right heart failure 5. IVC filter placement- use has become more common but reduction in mortality has not been conclusively demonstrated. Patients who have IVC filter placed are at a higher risk of recurrent DVT (but lower risk of recurrent PE). Complications of placement are rare but include- filter migration or misplacement, filter erosion, and perforation of IVC wall, and IVC obstruction due to filter thrombosis. Indications include- C/I to anticoagulation in a patient with DVT or PE, complication of current anticoagulation, failure of adequate anticoagulation as reflected by recurrent PE or DVT, a patient with low pulmonary reserve who is at high risk for death from PE |
|
|
Mechanism of action of heparin
|
promotes the action of antithrombin III
|
|
|
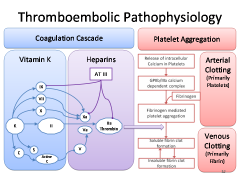
Mech of action of anticoagulants
|
|
|
Contraindications to heparin
|
1. active bleeding
2. uncontrolled HTN 3. recent stroke 4. Heparin-induced thrombocytopenia (HIT) |
|
|
low molecular weight heparin (LMWH) vs unfractionated heparin (UFH)
|
LMWH- better bioavailability and lower complication rates than UFH.
At least as effective if not more than UFH - longer half-life - given at weight adjusted doses-- do not need routine aPTT measurement |
|
|
Pretest probability and PE
|
If pre-test probability of PE is low then D-Dimer is a good non-invasive test to rule out PE. so if D-Dimer is negative then you can rule out clot. But if positive it does NOT help you because many things can cause an elevated D-Dimer
|
|
|
INR
|
- way of reporting PT in standardized fashion
- warfarin increases INR values - therapeutic INR is usually between 2-3. Notable exceptions are prosthetic mechanical heart valves, prophylaxis of recurrent MI, and treatment of antiphospholipid antibody syndrome, for which 2.5-3.5 is recommended |
|
|
What can you do if anticoagulation is contraindicated in a patient with a PE or DVT?
|
Vena cava filter
|
|
|
3 different types of pulmonary aspiration
|
1. acidic gastric content, which are especially damaging to the lungs
2. aspiration of oropharyngeal flora, which can lead to infection 3. foreign body fluids (e.g. chemicals) |
|
|
Which lung is usually affected if someone aspirates?
|
The right lung is most often involved due to anatomy- - the right main bronchus follows a more straight path down-- particularly the lower segments of the right upper lobe and upper segments of the right lower lobe
|
|
|
Predisposing factors to pulmonary aspiration
|
1. reduced level of consciousness (e.g. seizures, stroke, sedating drugs)
2. alcoholism 3. Extubation- impaired pharyngeal or laryngeal function 4. excessive vomitting, ileus 5. tube feeding, tracheostomy tubes 6. anesthesia, surgery 7. neuromuscular diseases 8. esophageal disorders (e.g. achalasia, GERD, cancer) |
|
|
Clinical features of pulmonary aspiration
|
1. Presentation is variable- some patients develop acute onset of respiratory distress. However, most often, the patient appears well, but later develops respiratory dysfunction (cough, SOB, fever, tachypnea, hypoxemia, or frothy sputum)
2. it may be initially silent, with development of acute respiratory failure with no obvious cause 3. fever may or may not be present 4, may lead to obstruction of the airways with localized wheezing |
|
|
Diagnosis of pulmonary aspiration
|
Findings on CXR are variable and resemble infiltrates that mimic bacterial pneumonia. Atelectasis and local areas of collapse may also be present
|
|
|
Treatment of pulmonary aspiration
1. if witnessed 2. if suspected 3. if obstruction 4. prevention 5. complications if untreated? |
1. If aspiration is witnesses- Airway, Breathing and circulation, supplemental oxygen and supportive measures
2. If aspiration pneumonia if suspected, give antibiotics (penicillin G or clindamycin). Although many patients who aspirate will go on to develop aspiration pneumonia-- antibiotic treatment is controversial as it may select for resistant organisms 3. if obstruction is present- early bronchoscopy is indicated 4. prevention is critical in patients at high risk for aspiration- keep the head of the bed elevated and place an NG tube to decompress the stomach 5. abscess formation |
|
|
How likely is aspiration pneumonia in the event of aspiration?
- which organisms are implicated? |
40% of patients who aspirate will develop pneumonia--usually 2-4 days after aspiration
- organisms are often mixed (aerobic and anaerobic) - foul smelling breath often indicates anaerobic infection - poor oral hygiene increases risk of infection |
|
|
Dyspnea- general characteristics
1. what should you assess on history? 2. most common causes of acute dyspnea 3. what elements of a history make lung disease more likely? |
1. distinguish acute from chronic
2. patients with chronic dyspnea usually have either heart or lung disease or both. It may be difficult to distinguish between the two 3. the most common causes of acute dyspnea include- 1. CHF exacerbation, pneumonia, bronchospasm, PE and anxiety 4. assess the patient's baseline level of activity, whether the dyspnea is new in onset and its association with exertion 5. If the patient has a history of smoking, cough, sputum, repeated infections or occupational exposure--> lung disease is likely the reason for the chronic dyspnea |
|
|
4 most common causes of acute dyspnea
|
1. CHF exacerbation
2. pneumonia 3. bronchospasm - as in asthma 4. anxiety |
|
|
What tests may be helpful in distinguishing lung and heart disease? (6)
|
1. CXR
2. Sputum gram stain and culture 3. PFTs 4. ABGs 5. ECG 6. echocardiogram |
|
|
Causes of dyspnea (ddx)
|
1. cardiovascular
a. CHF b. ischemic heart disease, acute MI c. pericarditis, cardiac tamponade d. arrhythmias e. valvular disease f. congenital heart disease 2. Pulmonary causes a. obstructive lung diseases- COPD, asthma, bronchiectasis b. PE c. ARDS d. Pneumonia, TB, bronchitis e. pleural effusion, pulmonary edema f. pneumothorax g. upper airway obstruction, foreign body aspiration (FBA) h. ILD i. chest wall abnormalities (kyphoscoliosis, rib fracture) 3. psychiatric disease- generalized anxiety disorder (GAD), panic attacks, hyperventilation, 4. systemic causes- severe chronic anemia, sepsis, DKA, GERD, medication (narcotic overdose) 5. chest wall abnormalities- kyphoscoliosis, rib fracture, ankylosing spondylitis 6. neuromuscular disease-- weaken respiratory muscles (myasthenia gravis, muscular dystrophy |
|
|
Diagnosis of dyspnea
|
1. thorough history and physical exam, vitals
2. pulse ox- normal is 96-100% on room air. Be aware that the baseline oxygen sat is chronically low in many cOPD patients 3. ABG- may be indicated if oxygen saturation is low on pulse ox-- if hypercarbia is suspected or to evaluate for acid-base abnormalities 4. CXR- can reveal pneumothorax, pleural effusion, pulmonary vascular congestion secondary to CHF, infiltrates due to pneumonia, ILD and so on 5. CBC- evaluate for anemia, infection 6. ECG- may show ventricular hypertrophy or evidence of ischemic heart disease 7. Echo- - for further evaluation of CHF, valvular heart disease 8. PFTs- perform if all of the above are normal or if an obstructive lung disease is suspected 9. V/Q Scan or spiral CT- perform if PE is suspected 10. bronchoscopy- indicated if foreign body aspiration is suspected |
|
|
treatment of dyspnea- general characteristics- when to use mech vent etc
|
1. treat the underlying causes
2. use mechanical ventilation in the following situations - impending respiratory failure is suspected - patient is unable to protect airway (e.g. decreased mental status, stroke, drug overdose) - severe hypoxia despite supplemental oxygen (PO2 < 50 to 60) - severe hypercarbia (PCO2 > 50) - exercise and conditioning may improve perception of dyspnea |
|
|
Hemoptysis- general characteristics
1. definition 2. amount and what it indicates |
1. expectoration of blood, hemoptysis varies widely in severity and medical significance. The amount of blood does not necessarily correspond with the gravity of the underlying cause
|
|
|
Differential diagnosis for hemoptysis
1. most common causes 2. other causes |
1. bronchitis (50% of cases), lung cancer (bronchogenic carcinoma), TB, bronchiectasis, pneumonia, many times the etiology is unclear after thorough eval (up to 30%)
2. goodpastures syndrome, PE with pulmonary infarction, aspergilloma within cavities, mitral stenosis-- elevated pulmonary venous pressure- vessels rupture, hemophilia |
|
|
Diagnostic evaluation of hemoptysis
|
1. verify that the hemoptysis has truly occurred. For example- superficial mouth lacerations and hematemesis may be confused with hemoptysis
2. history and physical - fever, night sweats, weight loss suggest TB or cancer. Fever and chills or history of HIV- suggest pneumonia or TB, look for risk factors for PE, in the presence of acute renal failure or hematuria, goodpastures syndrome should be considered 3. diagnostic studies a. CXR- may be a clear indicator of a pathogenic process or even diagnostic -- e.g. if fungus ball, irregular mass, granuloma, opacity consistent with pulmonary infarction is present. A normal CXR does not exclude a serious condition, especially PE or lung cancer b. fiberoptic bronchoscopy- should be performed even if CXR is normal if there is a significant clinical suspicion for lung carcinoma. look for small tumor that may not be evident on radiograph. May localize the site of bleeding. 4. CT of chest- performed as a complement to bronchoscopy or as a substitute if there are contraindications to bronchoscopy |
|
|
treatment of hemoptysis
|
1. treat the underlying cause
2. suppress the cough if it is aggravating the hemoptysis 3. correct bleeding diathesis (although anticoagulation is the treatment for PE) |
|
|
Why do patients with COPD sometimes have PND?
|
Their excessive airway secretions accumulate at night causing airway obstruction, resulting in dyspnea that awakens the patient and forces him or her to clear the airway. Therefore PND is not specific to heart disease
|
|
|
chronic CO2 retainers vs acute
|
common in COPD patients-- usually have a normal pH and increased HCO3 levels-- compensatory.
- If CO2 retention is acute, pH will be decreased and HCO3 will be near normal levels |
|
|
massive hemoptysis
|
- defined as more than 600 mL of blood in 24 hours
- the most common causes are bronchiectasis and bleeding diathesis - airway protection is key- intubate if necessary - bronchoscopy can help identify the source of the bleeding - use bronchial artery embolization or balloon tamponade of the airway if indicated. |
|
|
What is the oxygen saturation cutoff for receiving home oxygen?
|
</= 88%
|
|
|
ABG
1. what does it measure? 2. What is the normal range of blood pH? 3. How does PaO2 change with age? 4. What is the normal PaCO2 range? |

1. the partial pressures of oxygen and carbon dioxide along with the pH of arterial blood
2. Normal pH is 7.35 - 7.45 3. Normal PaO2 decreases with age 4. Normal PaCO2 is 35-45 mmHg |
|
|
For every 10 mmHg increase or decrease in PaCO2 what should the corresponding increase or decrease e?
- How do you determine whether the pH change is metabolic or respiratory? |
0.08. In general if the change in pH is in the same direction as the change in PaCO2 then the primary disorder is metabolic.
- when there is an inverse relationship then the primary relationship is respiratory (as when CO2 is retained--goes up then the pH should go down) |
|
|
Spirometry
1. What is it? 2. What is it used for? |
1. From maximum inspiration the patient exhales as forcibly as possible to maximum expiration-- PFTs. Spirometer plots the change in lung volume against time
2. Helps to distinguish obstructive from restrictive lung disease. - useful in assessing degree of functional impairment as well as monitoring effectiveness of treatment (during asthma exacerbation). May detect respiratory impairment in asymptomatic patients (e.g. smokers) Volumes are measured as percentages of predicted values based on age, height, and sex. - incorrect measurement of technique may lead to false positives. |
|
|
What are complications of obtaining an ABG?
|
It is painful and can cause radial artery spasm which may lead to ischemic in patient with a radial dominant circulation
|
|
|
DLco
1. explanation of test 2. what is it used for? |
1. The patient breathes in a small specific amount of CO, and the amount transferred from alveolar air to pulmonary capillary blood is measured. CO is a diffusion limited gas, so other variables are eliminated. Essentially measures the surface area of the alveolar capillary membrane.
2. Can often distinguish between asthma, emphysema and COPD. Useful in monitoring various conditions, such as sarcoidosis and emphysema |
|
|
Causes for low DLco (diffusing capacity for CO)
|
1. Emphysema
2. sarcoidosis 3. Interstitial fibrosis 4. pulmonary vascular disease 5. also lower with anemia due to reduced binding of CO |
|
|
Causes for high DLco
|
1. asthma-- increased pulmonary capillary blood volume
2. obesity 3. intracardiac shunt-- left to right shunt- inc pulm blood flow 4. Exercise 5. pulmonary hemorrhage (alveolar RBCs bind with CO) |
|
|
What does a high V/Q ratio indicate?
What is a normal V/Q ratio? |
Inadequate perfusion (more ventilation than perfusion)
Normal is 0.8 (so there is normally more ventilation than perfusion) |
|
|
What is a methacholine challenge and what is it used for?
|
Methacholine induces bronchospasm, which can thus determine the degree of airway hypersensitivity.
- Useful in patients in whom asthma or COPD is suspected - Sensitive in detecting airway hyperresponsiveness in mild asthma |

