![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
What are the causes of global hypoxic injury?
|
-Ischemia secondary to athersclerosis of the carotid artery
-Chronic carbon monoxide poisoning -Chronic hypoxemia (eg, chronic lung disease) -Cardiac arrest, shock -Repeated episodes of hypoglycemia in a type I diabetic (type I DM). |
|
|
What are the complications associated with global hypoxic injury?
|
a. Cerebral Atrophy due to apoptosis of neurons in layers 3, 5, and 6 of the cerebral cortex. This produces laminar necrosis & apoptotic neurons that stain bright red with eosin(called red neurons or eosinophilic).
b. Watershed infarcts that occur at junctions of arterial territories. Areas in-between do not have overlapping blood suppy; therefore the tissue is not well supplied with oxygen. Example junction between the anterior and middle cerbral arteries. c. Cerebrovascular accident (stroke) |
|

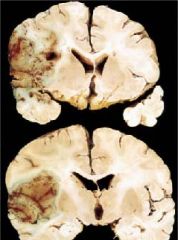
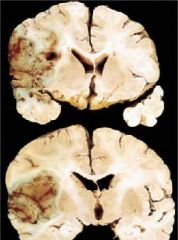
What is this?
|
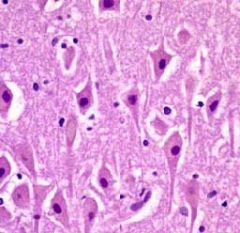
Cerebral Atrophy
|
|
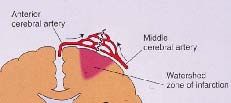
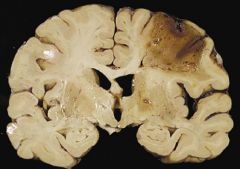
What is this?
|

Watershed infarct
|
|
|
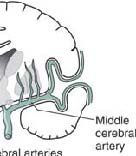
What are the key associated vessels with the circle of willis.
|
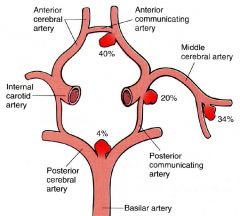
-Internal carotid artery
-Anterior Cerebral Artery -communicating branch of Anterior Cerebral Artery -Anterior Communicating Artery -Middle Cerebral Artery -lenticostriate branches of the middle Cerebral Artery -Posterior Cerebral Artery -Posterior Communicating Artery -Basilar Artery |
|
|
What locatations are most susceptible to watershed infarct?
|
-Junction between anterior and middle cerebral artery.
|
|
|
Definition of a watershed infarct.
|
-Occurs at the junctions of arterial territories. The blood supply does not overlap. Therefore this area is not well supplied with oxygen.
|
|
|
List the five type of cerebrovascular accidents.
|
1. Atherosclerotic stroke
2. Embolic stroke 3. Intracerebral hemorrhage 4. Subarachnoid hemorrhage 5. Lacunar infarcts |
|
|
Definition of atherosclerotic strokes.
|
Thrombotic(disrupted plaque) that causes a pale infarct (liquefactive necrosis) resulting in ischemia. Reperfusion usually does not occur. If reperfusion occurs there is a hemorrhagic infarction.
|
|
|
Pathogenesis of atherosclerotic strokes
|
-Result of a disrupted plaques resulting in pale infarct (liquefactive necrosis). Platelet thrombus develops over a disrupted plaque
-Occurs in the Middle Cerebral Artery and the internal carotid artery near the bifurcation. -Most occur in the distribution of the middle cerebral artery (MCA). -Reperfusion usually does not occur. -If reperfusion occurs it results in hemorrhagic infarction. |
|
|
What are the gross and microscopic findings in an atherosclerotic stroke?
|

1. Wedge-shaped area of pale infarction. Develops at the periphery of the cerebral cortex.
2.Swelling of the brain occurs with loss of demarcation between grey and white matter. Myelin begins to break down. 3. Gliosis is the reaction to injury. Astrocytes proliferate at the margins of the infarct. Microglial cells (macrophages) remove lipid debris. 4. Cystic area develops after 10 days to 3 weeks. |
|
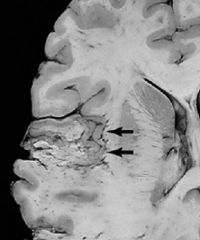
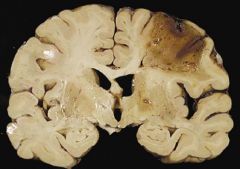
What is this?
|

Wedge-shaped area of pale infarction due to an atherosclerotic (thrombotic) stroke.
|
|
|
Transient ischemic attacks (TIA)
Something you should know & the definition, which has recently changed. |
Precede most strokes.
Definition - Deficits lasting 1-2 hours without CT or MRI evidence of damage. |
|
|
Amaurosis fugax-Definition, clinical findings, etc.
|
A type of TIA."Fleeting vision"
a. Retinal vessel embolization of a cholesterol plaque. It can visualized with an ophthalmoscope & is called a Hollenhurst plaque. b. It produces a sudden loss in vision. c. It is described as a curtain coming down over the eye and then going up when vision is restored. |
|
|
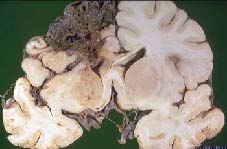
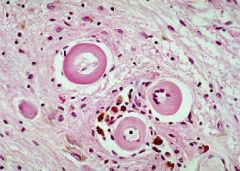
Red neurons
|
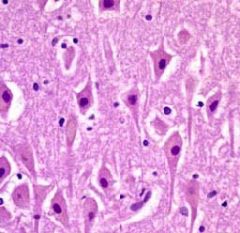
What should you be recognizing in this image?
|
|
|
Patient presents with following symptoms:
1. Contralateral hemiparesis and sensory loss in face and upper extremity 2. Expressive aphasia if Broca's area in dominant (left 85%) hemisphere involved. 3. Visual field is involved 4. Head & eyes deviate toward side of lesion Which artery is involved in this stroke? |
Middle Cerebral Artery (MCA)
|
|
|
Patient has:
1. Vertigo & Ataxia 2. Ipsilateral sensory loss in face 3. Contralateral hemiparesis and sensory loss in the trunk & limbs Which artery is involved in this stroke? |
Vertebrobasilar arterial system
|
|
|
Patient has
1) Paresis/paralysis in the contralateral leg and foot 2) Parethesia or anethesia in the contralateral leg and foot Which artery is involved in this stroke? |
Anterior Cerebral Artery
|
|
|
Definition of embolus
|
Detached mass
|
|
|
Source of emboli in an embolic stroke.
|
1) Most often originate from the left heart
2) Atherosclerotic debris from the Middle Cerebral Artery (MCA) and Carotid artery |
|
Definition of embolic stroke.
|
Hemorrhagic infaction that extends to periphery of cerebral cortex
|
|
Where do most embolic strokes occur?
|
Most occur in the distribution of the middle cerebral artery (MCA)
|
|
|
What produces hemorrhage in an embolic stroke?
|
Reperfusion after lysis of embolic material produces hemorrhage
|
|
|
How do you treat non-hemorrhagic infarcts
|
Thrombolytic therapy
|
|
|
Is thrombolytic therapy indicated in a embolic stroke?
|
No, it is hemorrhagic infarction, where thrombolytic therapy is contraindicated.
|
|
|
Intracerebral hemorrhage definition
|
Intracerebral hemorrhage is a complication of hypertension that is due to stress imposed the vessels by the high pressure.
(1) Branches of lenticulostriate vessels from MCA develop Charcot-Bouchard macroaneurysms (2) Ruputure of aneurysms produces intracerebral hemorhage (hematoma) |
|

Where are the common sites of intracerebral hemorrhage
|
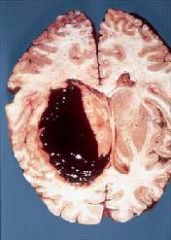
1. Basal ganglia (35-50% occur in the putamen)
2. Thalamus (10%) 3. Pons and Cerebellar hemispheres (10%) |
|
|
What is the result of treating hypertension?
|
Treatment of hypertension reduces the incidence of stroke by more than 40%
|
|
|
Definition of a Subarachnoid hemorrhage
|
-A hemorrhage that is below the arachnoid mater.
|
|
|
Pathogenesis of a subarchnoid hemorrhage
|
A subarachnoid hemorrhage is caused by the rupture of congenital berry aneurysm in most cases and bleeding from an arteriovenous malformation in others.
|
|
|
What is the patient presentation who has a subarachnoid hemorrhage?
|
Patient presents grabbing the back of their head (occiput) that has sudden occurred and is the "worst headache ever" with nuchal rigidity.
|
|
|
How many patients die after a subarachnoid hemorrhage?
|
50%
|
|
|
What are the complications of a subarachnoid hemorrhage?
|
-More hemorrhage (buhwahaha, evil laugh)
-Hydrocephalus -Permanent neurologic deficits |
|
|
What are the clinical findings of a subarachnoid hemorrhage?
|
1) Sudden onset of a severe occipital headache
2) About 50% die soon after hemorrhage 3) Complications include- a) Further hemorrhage b) Hydrocephalus c) Permanent neurologic deficits. |
|
|
Where do most congenital berry aneurysms develop?
|
They develop at junctions of the communicating branches of main cerebral artery because the junction lacks internal elastic lamina and smooth muscle. The most common site for berry aneurysm is the junction of the communicating branch with the ACA.
|
|
|
Where does the blood from the rupture go?
|

Blood goes into the subarachnoid space and covers the surface of the brain.
|
|
|
What are the CSF color changes in pathologic bleeds?
|
1) Pink, yellow, or orange-tinged CSF after centrifugation
2) Pink color is due to oxyhemoglobin from ruptured RBCs -color first occurs 2-4 hours post bleed; peaks 24-36 hours; subsides 4-8 days 3) Yellow to orange color (xanthochromia) is due to oxyHb breakdown to bilirubin. |
|
|
Xanthochromia
|
A yellow to orange color due to breakdown oxyHb to bilirubin is a sign of pathologic bleed. It firsts appears 12 hours post bleed; peaks 2-4 days; subsides 2-4 weeks.
|
|
|
Subarachnoid hemorrhage
|
rupture of congenital berry aneurysm
|
|
|
List the three types of strokes associated with hypertension
|
1. Intercerebral hemorrhage
2. Subarachnoid hemorrhage due to ruptured berry aneurysm 3. Lacunar Stroke |
|

Definition of lacunar infarct
|
-Cystic areas of microinfarction < 1 cm in diameter caused by hyaline arteriolosclerosis that are secondary to hypertension (most common) or diabetes mellitus
|
|
|
Lacunar
|
Lake
|
|
|
Where is the lesion & type of stroke if patient has motor deficits with or without dysarthria?
|
A lacunar infarct of the posterior limb of the internal capsule
|
|
|
Where is the lesion & What is the type of stroke if the patient has only sensory deficits?
|
A lacunar infarct of the thalamus.
|

