![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
73 Cards in this Set
- Front
- Back
|
XS EDTA can cause ? |
LOW PCV & MCV
|
|
|
SCID Hyperadrenocorticism, stress, steroid treatment, have what effect on lymphocyte level?
|
Absolute Lymphopenia
|
|
|
Aged samples may have low OR high MCV?
|
Aged samples may have raised MCV (cell swelling)
|
|
|
Inadequate centrif. has what affect on MCHC and PCV and MCV?
|
Raised PCV & MCV,
lower MCHC (MCHC = Hb / PCV) |
|
|
Life span of platelets?
|
Life span a few days
|
|
|
Is it okay to refrigerate platelets before counting?
|
NO
|
|
|
Younger platelets have higher OR lower MPV?
|
Big platelets occur --> high MPV in thrombopoiesis or platelet neoplasm
|
|
|
6. A blood sample was drawn and placed into a green-top tube containing Li-heparin. Which blood assay would be run?
a. CBC b. Glucose c. Coagulation profile d. Chemistry |
d. Chemistry
|
|
|
8. Na-citrate (light blue) is used for which blood assay?
a. CBC b. Glucose c. Coagulation profile d. Chemistry |
c. Coagulation profile
CBC |
|
|
Qualitative Buffy Coat (QBC ) analyser used for measuring?
|
small machine gives accurate cell & platelet counts, & part differential WBC count
|
|
|
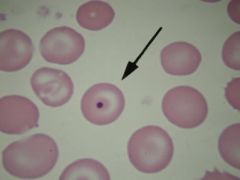
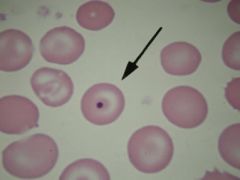
These are examples of what type of stains?
Wright’s, Diff-quik (most common), Leishman’s, May-Grunwald-Giemsa |
Romanowsky stains
|
|

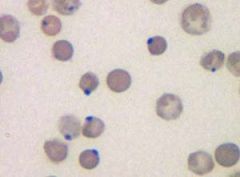
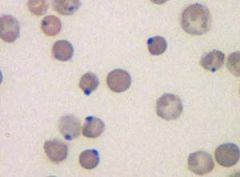
name these sites on blood smear
|

see pic
|
|
|
Where best place to do differential WBC count on blood smear?
|
monolayer
|
|
|
Where on blood smear might u find microfilariae In heartworm areas of the world?
|
feathered edge of smear
check with 10X at feathered edge of smear for microfilaria |
|
|
CSF, pleural/peritoneal/pericardial, & joint fluids should be split and part placed into ____________________ (to preserve cell morphology) & part into sterilin tubes (for culture).
|
EDTA
|
|
|
33. Polychromasia & anisocytosis (RBCs unequal size) may be seen in animals which have been poisoned with:
a. Copper b. Iron c. Lead d. Cobalt e. Magnesium |
C. Lead poisoning, b/c associated with Polychromasia & anisocytosis due to inappr. RBC regen.
(actually pretty sure copper can also cause this, but only an in large animals i guess) |
|
37. H-J bodies = DNA remnants of nucleus. Low numbers may be present in healthy ___ b/c spleen is not very effective in removing them.
|
CATS
|
|
|
intracellular protozoan causes IV hemolysis in cattle therefore causing “redwater” or reddish urine
|
babesia
|
|
|
45. T/F? Both intra-- & extravascular hemolysis cause hyperbilirubinemia
|
False; extravascular
IV hemolysis more likely to cause hemogloburia and hemoglobinemia |
|
60. Which is not a listed cause of Heinz Body anemia?
a. Copper toxicity in sheep b. Inorganic phosphate deficiency c. Tylenol (acetaminophen) d. Brassica e. A sh*t ton of plants f. T. cruzi g. onion |
f. T. cruzi
|
|
|
Splenomegaly & hepatomegaly are the result of ?
|
EV hemolysis?
|
|
|
Dyserythropoiesis means?
Dyshemopoiesis? |
1. difficulty producing RBC;s
2. difficulty producing all blood cells |
|
|
62. Bacillary Hemoglobinuria is the result of:
a. Deficiency of inorganic phosphate b. EIAV c. Liver infarct & the release of hemolytic beta toxin d. Isoimmune hemolytic anemia e. Babesia |
c. Liver infarct & the release of hemolytic beta toxin (Clostridium)
|
|
|
Postparturient hemoglobinuria is due to ? (5)
|
dietary deficiency in: Inorganic phosphate; also cold weather, copper def., too much water, certain plants
|
|
|
Aplastic anemia?
hypoplastic anemia? |
3. aplastic anemia is no production
4. regeneration poor (hypoplastic anemia) |
|
|
Most common type of anemia?
Is it acute or chronic? Source of problem? |
Secondary Dyshemopoiesis anemia, beginning outside bone marrow, chronic condtition
|
|
|
6 causes of Dyshemopoiesis anemia
|
1. Immune destruction of RBC precursors (rare)
2. Toxins like Estrogen 3. Neoplasms 4. Iron-deficiency 5. Iron sequestration from chronic disorder 6. infection |
|
|
Name 3 things that can damage RBC, WBC or Plt precursors anemia or all. Dyshemopoietic anemia.
|
Estrogen or Bracken fern (and Ehrlichea) affect on blood cell levels
|
|
|
Cows have eaten Bracken fern. Which symptoms will you see last: for anemia? leukopenia? or thrombocytopenia?
|
All are not being produced, but will see symptoms of anemia last b/c RBC life span longest (80-160 days), but WBC have lifespan of few hours.
|
|
|
Causes of intravascular hemolysis? (3)
|
Babesiosis, Clostridium hemolyticum (Bacillary Hb.uria), Post parturient Hb.uria (also get some extravascular)
|
|
|
Animals with Bracken fern poisoning show what symptoms?
(skip until know else) |
high temp., septicemia (low WBC so bacteria come in)
bleeding from nose, mouth (thrombocytopenia) |
|
|
Why does body sequester iron in BM (macrophages) during inflam. dz?
|
Body acts as if it has bacterial infection
|
|
|
Aside from anemia, offer symptoms of inflam.dz?
|
Leukocytosis, Neutrophilia , left shift, high globulin (protein level),
|
|
|
What is a left shift?
|
appearance of immature neutrophils (band cells) in blood
|
|
|
granulocytes?
|
eosinophils neutrophils & basophils
|
|
|
Mononuclear cells ?
|
lymphocytes & monocytes
|
|
|
Neutrophil granules are more prominent in ? ALSO called????????????
|
rabbit, guinea pig, birds & reptiles aka “heterophils”.
|
|
|
Neutrophil granules more prominent in large animals OR cats/dogs?
|
Neutrophil granules more prominent in large animals
|
|
|
circulating WBC’s vary with species, which has highest?
|
pigs highest circulating WBC conc.; also very excited
|
|
|
Neutrophils higher OR lower in young animal?
|
higher in young
|
|
|
Dogs, cats, horses which WBC dominant?
|
Neutrophils
|
|
|
In Ruminants & Pigs, which WBC predominate?
|
– Lymphocytes predominate
|
|
|
Which WBC pool lie dormant on walls of small blood vessels; release if excited ? What is this called when released due to adrenaline incr.?
|
MARGINATED pool
“physiological leukocytosis”. |
|
|
maturing pool called ?
|
PROLIFERATING pool
|
|
|
T or F: ALL WBC’s enter tissues & remain there
|
~False: EXCEPTION lymphocytes which may recirculate back to blood directly, or through lymphatics.
|
|
|
Pathological leukocytosis caused?
|
* infection trauma/ burn autoimmune disease;
*Stress/Cortisone (effect moderate) *Bone marrow Neoplasia (eg MPD or LPD) effect variable – can be marked *RBC regeneration- effect usually mild/moderate |
|
|
A higher proportion of marginated cells are lymphocytes in what species?
|
CATS
(therefore with epinephrine release / excitment -> greater increase of lymphocytes in cats) |
|
|
What are 3 things that happen to WBC levels when animal is given corticosteroids? (in sequential order)
|
1. lymphopenia (esp. in cow - b/c major cell type in cattle)
2. mature neutrophilia 3. sometimes eosinopenia/ monocytosis (incr.) in dogs only |
|
|
Myelodysplasia and myeloproliferative disorders?
|
difficulty in producing 1 or more cell types
|
|
|
Viral infections can decimate WBC’s e.g. ? (3)
|
parvovirus & canine adenoviral hepatitis
|
|
|
Viral infections can slowly damage precursor cells for example...(name 3 or 4)
|
Viruses which FeLV, FIV, BoLV, BVD/MD;
|
|
|
In what species is leukocytosis uncommon w/o severe inflam., but when occurs is grim prognosis?
|
HORSE, leukocytosis uncommon but serious
|
|
|
T or F: Inflammation causes leukocytosis in cattle; why or why not.
|
False: Inflam. often causes LEUKOPENIA in cattle, b/c have small neutrophil pool which low/migrate quickly to site of inflammation
|
|
|
T or F: Don’t rely on total WBC count in cow.
|
True
|
|
|
Inflam. leukogram:
|
1. leukocytosis
2. neutrophilia (increased neutrophil release) 3. left shift |
|
|
Regenerative left shift
|
left shift + leukocytosis
(increase in circulating pool in severe inflammation) |
|
|
Nonregen. left shift?
Characteristic of? Prognosis? |
*left shift + NO leukocytosis (no incr. in WBC); immature outnumber mature
*systemic toxemia, BM unable *prognosis bad |
|
|
Inflammatory leukogram + monocytosis indicates?
|
‘chronic/granulomatous’ inflammatory leukogram
|
|
|
Neutropenia (decr. release) from bone marrow caused by ? (4)
|
decrease in progenitor cells from some drugs, viral infections, neoplasias, Chediak-Higashi syndrome.
|
|
|
4 causes of neutrophil decr.:
|
1. Decreased release
2. Increased exit 3. Increased destruction 4. Shift from circulating to marginated pool; maybe in shock..why? |
|
|
Congenital anomaly in man dog & other spp; granulocytes look immature but function normally. May cause healthy animals to have marked “left shift”
|
PELGER-HUËT ANOMALY: granulocytes look immature but function normally
|
|
|
Chediak-Higashi syndrome occurs in ? (3)
|
in man cow cat;
|
|
|
Chediak-Higashi syndrome characterized by? (4 symptoms)
|
neutropenia & neutrophils have big granules; animals are infection-susceptible, ? albino, & bleed easily
|
|
|
Neutrophil adhesion defect in what animals ? (2)
|
Irish setter, Holstein cow
|
|
|
Neutrophil adhesion defect char. by? (4)
|
poor chemotaxis & recurrent bacterial & fungal infections; ? neutrophilia, left shift, hard to diagnose
|
|
|
Neutrophil adhesion defect diagnosed how?
(skip until end) |
Neutrophil function test (difficult for small practice)
|
|
|
autosomal recessive trait in S/Gr collies; 10-14 day cyclical fluctuation in neutrophils & WBC count --> inf.-susc.; also ? microphthalmia, GI probs
|
Canine cyclic hematopoiesis
|
|
|
Inclusions in neutrophils may include ?
(give 3 examples) |
Inclusions in neutrophils may include Bacteria, Ehrlichia Distemper inclusions &Hepatozoon americanum
|
|
|
What is this called? If many neutrophils have >4/5 lobes
|
NEUTROPHIL HYPERSEGMENTATION
|
|
|
NEUTROPHIL HYPERSEGMENTATION indicates?
prognosis? |
it indicates presence of older cells & that production of young neutrophils is impaired
*guarded prognosis |
|
|
Eosinophilia caused by (4)
|
Hypersensitivity
Parasitism Addison’s ? Eosinophilic myositis ? Eosinophilic MPD |
|
|
Basophilia caused by (2)?
|
IgE mediated disorders
Mast cell tumor ? |
|
|
Monocytosis caused by (3)?
(how do monocytes change?) |
Chronic inflammation
esp. if granulomatous Stress (in dog) Monocytic sarcoma *monocytes get bigger |

