![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
265 Cards in this Set
- Front
- Back
|
Major 4 components of haematopoietic system?
|
Bone Marrow
Liver Lymph nodes Spleen |
|
|
3 things produced by lymph nodes?
|
B & T lymphocytes, plasma cells
|
|
|
What is the main source of erythrocytes, neutrophils, eosinophils, monocytes and platelets?
|
Bone marrow
|
|
|
4 things produced by spleen
|
B & T lymphocytes, plasma cells AND retains haematopoietic potential
|
|
|
How long does it take to produce rbcs
a) normal circumatances b) high demand |
a) 7 days
b) 2-4 days |
|
|
Which cytokine regulates rbc production?
|
Erythropoietin (renal tissue produces in response to hypoxia. Stim stem cell differentiation and increases maturation rate)
|
|
|
How is CO2 carried away from the tissues?
|
Mostly transported as HCO3 dissolved in plasma, some transported via haemoglobin
|
|
|
Which blood cell is the longest living?
|
RBCs
|
|
|
Why do RBCs require blood glucose?
|
Can't synthesize proteins or lipids
|
|
|
How long do WBCs live?
|
1-3 days
|
|
|
Name the two classifications of haemolysis and their prevalence
|
Extravascular (90%) old or damaged rbcs removed by macrophages in spleen, liver, bone marrow
Intravascular haemolysis (10%) e.g. IMHA |
|
|
How do we get haemoglobinuria?
|
Intravascular haemolysis - haptoglobin binds haemoglobin in blood but once haptoglobin is saturated, excess haemoglobin is free in blood, small enough to filter through glomerulus
|
|
|
Why do we need dietary iron?
|
Forms part of the heme group. Usually recycled well from catabolised rbcs ao not much needed in diet to replace losses
|
|
|
Name two conditions that could increase serum iron
|
Haemolytic anaemia, hyperadrenocorticism
|
|
|
Name two conditions that could cause decreased serum iron
|
Iron deficiency
Acute or chronic inflammatory disease |
|
|
What is MCV?
|
Mean corpuscular volume
|
|
|
Three conditions that would cause increased MCV?
|
=macrocytosis.
Reticulocytosis IMHA Poodles FeLV |
|
|
Three conditions that would cause decreased MCV?
|
=microcytosis
Iron deficiency anaemia Liver disease (e.g. portosystemic shunt) Japanese Akita |
|
|
What is MCHC?
What would cause it to -increase -decrease (2) |
Mean corpuscular haemoglobin concentration.
Increase = atrefact Decrease = reticulocytosis, iron deficiency |
|
|
What is MCH?
|
Mean corpuscular haemoglobin
|
|
|
Reticulocytes are a good measure of the bone marrow response in all species except what? Why?
|
Horses - rarely see retics in circulation in horses.
|
|
|
Why is absolute retic count more accurate than retic %?
|
Anaemia will increase the percentage.
|
|
|
What causes acanthocytes
a)in general b) in cats c) in dogs |
a) increased cholesterol in membrane
b) hepatic lipidosis c) haemangiosarcoma |
|
|
Name two types of keratocytes (morph. names)
and three things that can cause them |
Blister cells, helmet cells. Damage to cell membranes, caused by
DIC (fibrin strands) Iron deficiency Vascular neoplasms |
|
|
What are schistocytes and name three things that can cause them
|
Fragmented rbcs,
DIC Iron deficiency Vascular neoplasms |
|
|
What causes spherocytes?
|
Partial phagocytosis of rbcs - IMHA
|
|
|
What causes eccentrocytes and what else do we commonly see with them?
|
Oxidative damage, Heinz bodies
|
|
|
When would you see basophilic stippling in
a)smallies b)largies |
Smallies - lead toxicity
Largies - regenerative response |
|
|
What causes Heinz bodies?
|
Oxidative damage. <10% is normal in cats bc their spleen is less effective at removing them
|
|
|
What are Howell-Jolly bodies and give three causes
|
Retained nuclear material
Regenerative response Chronic steroid therapy Reduced splenic function |
|
|
How can we differentiate between rouleaux and agglutination of rbcs?
|
Add saline - agglutination persists
|
|
|
3 broad categories that result in anaemia
|
Increased loss (haemorrhage)
Increased destruction Reduced production |
|
|
How many days does it take for a regenerative response to occur?
|
3-5 days
|
|
|
How can plasma protein help us classify anaemia?
|
TP normal = haemolysis
TP low = external loss (haemorrhage) |
|
|
Microcytic anaemia in a dog - what two tests would you do?
|
Serum Fe level
Faecal blood (this is common reason for Fe deficiency) |
|
|
What do metarubricytes in circulation indicate?
|
Regenerative response to anaemia
|
|
|
What effect does chronic external haemorrhage have on the regenerative response?
|
Depletion of iron stores - regenerative response ceases
Blood sucking parasites, GI ulcers |
|
|
Internal blood loss - what would you expect TP to do? What grade anaemia would you expect and why?
|
TP normal because reabsorbed. RBC components reabsorbed and recycled so anaemia milder than external blood loss.
Bleeding tumours, bleeding disorders, GI ulcers |
|
|
Why can the body have such a massive regen response to IMHA?
|
Because iron is released and used directly.
NB TP stays normal, like with internal blood loss. |
|
|
What would be elevated in the wbcs in IMHA?
Urine? Serum biochem? |
Neutrophils and leucocytes due to tissue damage
Urine - Haemoglobin Bilirubin (icterus) |
|
|
4 causes of intravascular haemolysis?
|
Blood parasites
Osmotic injury IMHA Oxidative damage |
|
|
What are the two forms of haemolytic anaemia in smallies and which is most common?
|
Extravascular and intravasculr. Extravascular is most common (spleen)
|
|
|
Four causes of non-regenerative anaemia due to reduced rbc production
|
Anaemia of chronic disease/inflammation (iron sequestration)
Anaemia of chronic renal disease (decreased EPO) Myelophthistic anaemia - BM replaced by something els Hypoplastic or aplastic anaemia - usually reversible. |
|
|
Two causes of non-regen anaemia due to reduced Hb synthesis
|
Chronic iron deficiency
Copper deficiency |
|
|
Microcytic, hypochromic anaemia with schistocytes and keratocytes, regenerative progressing to non regenerative - likely diagnosis?
|
Iron deficiency anaemia
|
|
|
Four cell types of the innate immune system
|
Neut, Eosin, Mono, Baso
|
|
|
Cell type of the humoral immune system
|
B lymphocytes
|
|
|
Describe how the innate and humoral immune systems work together
|
Monocytes present antigen (bacteria) to B cells. B cells produce antibody which coats those bacteria, neutrophils destroy all Ab coated bacteria
|
|
|
Describe the neutrophil:lymphocyte ratio in:
-dogs -cats -horses -cows |
Dogs N>L
Cats are the same Horses N=L Cows L>N |
|
|
Three main causes of Neutrophilia
|
Physiological (fear/excitement)
Stress (corticosteroid) Inflammatory |
|

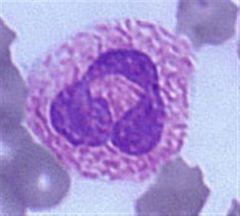
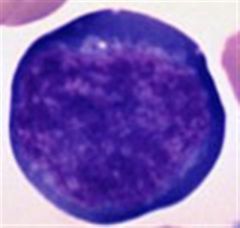
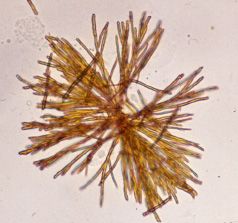
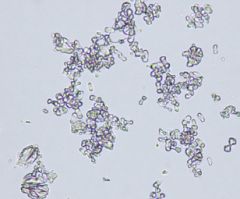
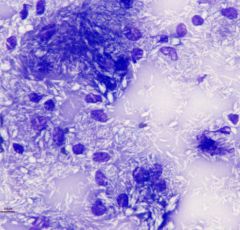
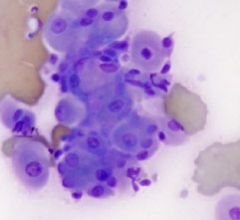
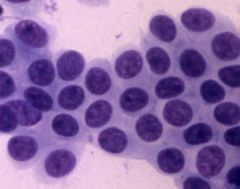
Name that cell
|
Band
|
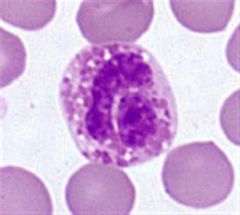
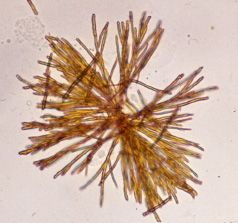
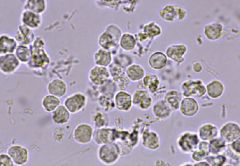
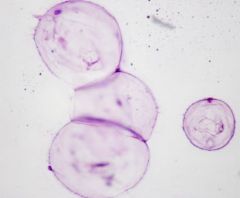
|
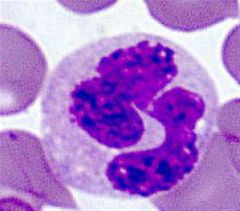
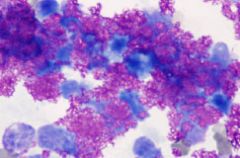
Name that cell
|
Cat eosinophil
|
|
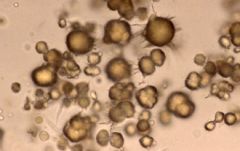
|
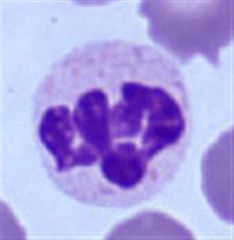
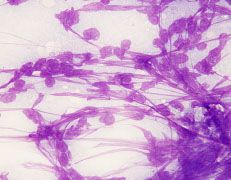
Name that cell
|
Dog eosinophil
|
|
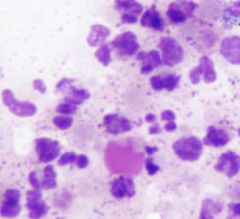
Name that cell
|
Dog eosinophil
|
|
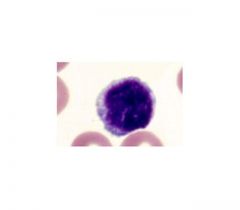
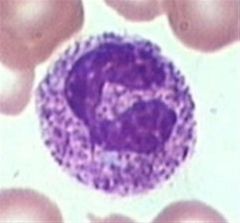
Name that cell
|
Lymphocyte
|
|
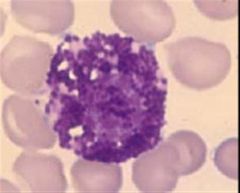
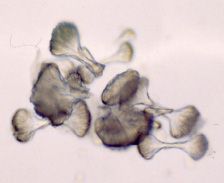
Name that cell
|
Mast cell
|
|
Name that cell
|
Metamyelocyte
|
|
Name that cell
|
Monocyte
|
|
Name that cell
|
Neutrophil
|
|
|
Name that cell
|
Neutrophil
|
|

Name that cell
|
Neutrophil
|
|
Name that cell
|
Neutrophil with toxic granulation
|
|
Name that cell
|
Reactive lymphocyte
|
|
|
Four reasons for monocytosis
|
Tissue necrosis (remove tissue)
Chronic inflammation Coticosteroid excess (stress leukogram) Neutropenia (compensatory) |
|
|
Five causes of lymphocytosis
|
Physiologic response (adrenaline)
Chronic inflammation Lymphoid leukaemia BLV infection Addisons disease (due to absence of glucocorticoids) |
|
|
Four reasons for lymphopenia
|
1. Stress leukogram (corticosteroid)
2. Lymph loss, sequestration or drainage (lymphangiestasia, protein losing enteropathy, chylothorax) 3. Reduced lymphopoiesis (e.g. removal of thymus) 4. Acute viral infection |
|
|
What is BLAD and CLAD?
|
Bovine/Canine Leukocyte adhesion deficiency
Lack glycoprotein required for adhesion - limited ability to get into tissues from bloodstream Stunted growth, neutropenia and recurrent infections seen |
|
|
Define leukaemia
|
Neoplastic proliferation of haematopoietic cells in the bone marrow (hence end up in the circulation too).
The leukaemia is classified by the type of neoplastic cell present - rbcs, neuts, eos, monos, lymphos, platelets... |
|
|
How do we definitively diagnose a leukaemia?
|
BM biopsy - detect lots of blast cells for the neoplastic cell type
|
|
|
How can leukaemia of e.g. lymphocytes cause neutropenia?
|
Displacement of other cell lines. Can cause low levels of any of the other cell lines
|
|
|
Myeloproliferative disorders:
Where do they arise? What are the three common types? |
Bone marrow stem cell system
Granulocytic (granulocyte precursor) Monocytic (Monocyte precursor) Erythroid (Rubricytes rbc precursor) |
|
|
Lymphoproliferative disorder = neoplastic process with lymphoid cell differentiation.
What are they called when they're in: a) solid tissue b) bone marrow/blood c) Plasma cells? |
Solid tissue = lymphoma
BM/blood = lymphoid leukaemia Plasma cells = myeloma |
|
|
What do you call a lymphoproliferative disorder of Plasma cells?
|
Myeloma
|
|
|
What do you call a lymphoproliferative disorder of the BM/blood?
|
Lymphoid leukaemia
|
|
|
What do you call a lymphoproliferative disorder of solid tissue? What species is this most common in?
|
Lymphoma. Cats.
|
|
|
What is the difference cytologically between acute leukaemia and chronic leukaemia? Clinical course?
|
Acute = immature blast forms. Short clinical course if not treated.
Chronic= more mautre forms, longer clinical course (months - years) |
|
|
Where does lymphoma originate?
|
Lymph nodes. Disseminates to other nodes then to tissues and the bone marrow.
|
|
|
Clinical characteristics of acute lymphocytic leukaemia:
a) circulating lymphocyte count b) neoplastic circulating cell type c) BM aspirate shows what? d) Prognosis |
a) normal to high
b) immature blast cells c) >30% of BM cells are immature blast forms d) poor Commonly also see neutropenia, anaemia and thrombocytopenia. |
|
|
Chronic lymphocytic leukaemia:
a) circulating cell type b) clinical significance |
a) mature lymphocytes
b) may be picked up incidentally, long clinical course (months to years) |
|
|
Do we see leukaemia with lymphoma?
|
Only in 10-25% of cases
|
|
|
What is the most common malignant tumour of cats?
|
Lymphoma
|
|
|
What proportion of FeLV cats develop neoplasia?
|
1/3rd
|
|
|
When do we see leukaemia with feline lymphoma?
|
In approx 50% of cases. Once BM has been invaded (LN - tissues -BM)
|
|
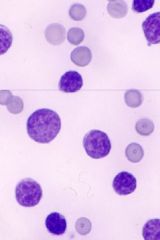
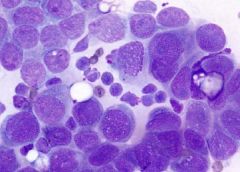
Blood smear from cat with nonregen anaemia and lethargy. Likely diagnosis?
|
Immature lymphocyte blast cells seen, feline lymphoma likely. Anaemia due to myelophthisis. NB BM only involved in 50% of feline leukaemias.
|
|
|
Likely type of lymphoma in a cow:
a) < 6mths old b) 1-3 years old c) >6yrs old |
< 6mths: Sporadic Juvenile (calf) lymphoma
1-3yrs: Sporadic Thymic or cutaneous lymphoma >6yrs Enzootic Bovine Leukosis |
|
|
What causes Enzootic Bovine Leukosis?
What distribution in the body? How many cows develop clinical disease? |
Bovine Leukaemia Virus (BLV)
Multicentric (eg abomasum, LNs, heart, kidneys...) Many asymptomatic carriers 30% develop persistent leukocytosis <5% become clinical Rare in NZ - eradication scheme |
|

2 year old cow. Two differentials? How would you differentiate?
|
Sporadic cutaneous lymphoma
Papillomatosis Cytology or histology |
|

6 month old calf, massively enlarged LNs
Likely diagnosis? |
Sporadic juvenile lymphoma
|
|

2 year old cow, massive swelling at thoracic inlet - likely diagnosis?
|
Sporadic thymic lymphoma (occurs 1-3yrs old)
|
|

7 yo cow, exophthalmos and poor condition score. Diagnosis? What is the cause?
|
Enzootic bovine leukosis. Cause by Bovine Leukaemia Virus. Only 5% become clinical. Tumour cells have infiltrated periocular tissues.
|
|
|
Four things that albumin transports in the blood?
|
40% of serum calcium
Hormones Drugs Bilirubin |
|
|
What produces
a) alpha globulins b) beta globulins c) gamma globulins |
alpha and beta - liver
gamma - B Lo and plasma cells |
|
|
Four causes of hypoalbuminaemia
|
Liver disease (see increase globulins)
Malnutrition Malabsorption Exocrine pancreas insufficiency Also get compensatory if have hyperglobulinaemia |
|
|
Three causes of hyperglobulinaemia
|
Dehydration
Inflammation (acute or chronic) Plasma cell myeloma |
|
|
Polyclonal gammopathy - what do we suspect?
|
Chronic inflammation
|
|
|
Monoclonal gammopathy - what do we suspect?
|
Plasma cell myeloma
|
|
|
Name the main acute phase protein used in clin path
|
Fibrinogen
|
|
|
6 causes of lipaemia in smallies
|
Same as hypercholesterolaemia
Post prandial (nonpathogenic) Hypothyroidism Diabetes mellitus Cholestatic liver disease Pancreatitis Nephrotic syndrome |
|
|
6 causes of lipaemia in smallies
|
Same as lipaemia
Post prandial (nonpathogenic) Hypothyroidism Diabetes mellitus Cholestatic liver disease Pancreatitis Nephrotic syndrome |
|
|
Cause of hyperlipaemia in horses
|
Negative energy balance - mobilisation of FFAs - can lead to fatty liver
|
|
|
Define primary haemostasis
|
Formation of platelet plug
|
|
|
Define secondary haemostasis
|
Stabilisation of platelet plug with fibrin
|
|
|
Haemostasis consists of four steps:
1. Platelet plug 2. Fibrin stabilisation of platelet plug What are steps 3 and 4? |
3 - Removal of fibrin plug
4. Tissue repair |
|
|
What steps are involved in primary haemostasis?
|
Vascular injury - vasoconstriction - adhesion of platelets - aggregation of platelets - platelet contraction
|
|
|
Why is normal liver function essential for haemostasis?
|
Most clotting factors and clotting inhibitors are produced in the liver.
|
|
|
Which clotting factors make up the intrinsic pathway? What stimulates it?
|
8,9,11,12 (in reverse order)
Contact with collagen (negatively charged surface) |
|
|
Which clotting factors make up the extrinsic pathway? What stimulates it?
Why is it called extrinsic? |
7. Tissue factor. TF is found in many cells but not free in the plasma hence extrinsic. Activated when tissues are damaged (cells release tissue factor)
|
|
|
Which factors make up the common clotting pathway?
|
10, 5, 2 (in that order).
What is the result? Factor 10 converts prothrombin to thrombin. Then thrombin os converted to fibrin. |
|
|
Describe fibrinolysis
|
Plasminogen is converted to Plasmin.
Plasmin dissolves fibrinogen and fibrin - cleaves them into smaller "fibrin degradation products". Some FDPs inhibit clotting. |
|
|
What three things can set off DIC?
|
Endothelial damage
Platelet activation Tissue factor activation |
|
|
Describe the pathogenesis of DIC
|
Something causes mutliple fibrin clots to form in terminal vasculature
Results in widespread activation of fibrinolysis - lots of FDPs produced FDPs inhibit coagulation, at the same time all the clotting factors and platelets are being used up. Uncontrollable haemorrhage |
|
|
3 categories of primary haemostasis defects
|
Platelet defects (number or function)
von Willebrands factor defects vessel wall defects |
|
|
4 reasons for thrombocytopenia
|
increased consumption
increeased destruction decreased production sequestration |
|
|
Epistaxis, haematochezia, petechiae, ecchymoses, haematuria, melaena - disorder of primary or secondary haemostasis?
|
Primary.
|
|
|
haematomas, ecchymoses, bleeding into body cavities, prolonged post surgical bleeds - disorder of primary or secondary haemostasis?
|
Secondary - unable to form insoluble fibrin. Platelet plug forms but not stabilised. aka coagulopathies
|
|
|
What tubes are appropriate for coagulation profiles?
|
EDTA or citrate
|
|
|
Describe the Thrombin Time test
|
Add calcium and thrombin to plasma. Assesses time taken to convert fibrinogen to fibrin.
Prolonged if: Low fibrinogen (DIC, liver failure) Increased FDPs (DIC) |
|
|
Describe the Activated Clotting Time test
|
Measures intrinsic and common pathways (12,11,9,8,10,5,2)
Quick and can be done in clinic. |
|
|
Haemophilia A, B and C are disorders of primary or secondary haemostasis?
|
Secondary (8,9,11 respectively)
|
|
|
Give 3 examples of acquired secondary haemostasis disorders
|
DIC
Severe chronic liver disease Vitamin K antagonism |
|
|
If a dog is suspected to have ingested coumarins (rat bait) but his PT time is normal - what would you do?
|
It takes 36-72 hours for PT to become pprolonged, so retest in 48-72 hours, treat with Vit K in the meantime.
|
|
|
Differences between primary and secondary bleeding disorders wrt:
a) petechiae b)haematomas c) site of bleeding d) Onset of bleeding e) BMBT test f) Coagulation times |
a) Primary - get petechiae, secondary they are rare
b) Primary don't get haematomas c) Primary - mucous membranes, generalised. Secondary - often localised, joints, muscles, cavities d) Primary immediate, secondary delayed e) BMBT prolonged in primary, normal in secondary e) Coagulation times normal for primary, increased for secondary |
|
|
Which species has naturally occuring isoantibodies against red blood cell antigens?
|
Cats
|
|
|
70% of cats have Type ? blood
30% of cats have type ? blood |
A 70%
B 30% |
|
|
Why can dogs have reactions to blood transfusions on the second but not the first transfusion?
|
First - haven't formed any Abs yet. Second - have preformed Abs against rbc Ags
|
|
|
What does blood crossmatching tell us?
|
Whether the recipient has Abs to the donors rbc Ags
|
|
|
Why is a major crossmatch more important than a minor crossmatch?
|
If a reaction occurs with a minor crossmatch there is only a small qty of Abs in the donor blood, insifficient to cause too mcuh lysis. But major crossmatch reaction - host has Abs to donor Ags - all of the donated blood will be lysed and there will be a major allergic rxn
|
|
|
What is ADH, where does it come from and what does it do?
|
Antidiuretic hormone, from the posterior pituitary gland, causes collecting ducts to be more permeable to water hence more is reabsorbed.
|
|
|
Which is more significant on a urinalysis - 2+ protein in concentrated urine, or 2+ protein in dilute urine?
|
Dilute!
|
|
|
How can bacteria increase the pH of urine?
|
Urease-producing bacteria
|
|
|
3 categories of proteinuria
|
Prerenal, renal, postrenal
|
|
|
Causes of prerenal proteinuria (3)
|
= protein exceeds absorptive ability of tubules
Hburia, myoglobunuria, bence jones protein (plasma cell myeloma) |
|
|
Cause of renal proteinuria and two things that lead to it?
|
Glomerular disease
Renal amyloidosis, immune-mediated glomerulonephritis |
|
|
Most likely cause of post renal proteinuria?
|
Urinary tract inflammation/infection
|
|
|
What protein do urine dipsticks detect in urine?
|
Albumin. Insensitive to globulins and bence jones.
|
|
|
How do we quantify proteinuria?
|
Urinary protein:creatinine ratio. In a quiet sediment (no blood etc), elevated ratio strongly suggests glomerular disease.
|
|
|
Is trace protein significant in concentrated urine?
|
No
|
|
|
Can microscopic (nonvisible) blood contamination increase urine protein on dipstick?
|
No
|
|
|
Does chronic renal failure cause proteinuria?
|
Not usually
|
|
|
What is the most likely cause of marked proteinuria?
|
Glomerular disease (but not only differential)
|
|
|
What is the renal threshold for blood glucose to appear in the urine?
|
10mmol/L
|
|
|
Four reasons for glucosuria to occur?
|
Diabetes mellitus
Stress Cushings Impaired tubular resorption |
|
|
What does ketonuria represent? (2)
|
Defective carbohydrate metabolism or excessive fat breakdown
|
|
|
Four causes of ketonuria? (Two apply only to largies)
|
Diabetes mellitus
Starvation Bovine ketosis Preg tox in sheep |
|
|
Why does only conjugated bilirubin appear in urine?
|
Unconjugated bilirubin is bound to albumin - so it is too big to get through glomerulus
|
|
|
What is the significance of trace bilirubin in the urine of a
a) cat b) dog |
a) Likely cholestatic liver disease
b) Insignificant |
|
|
Two main causes of bilirubinuria?
|
Hepatobiliary disease
Heamolysis |
|
|
How would you differentiate between Hburia, Haematuria, Mburia?
|
Hburia - doesn't spin down
Haematuria - spins down Myoglobinuria - doesn't spin down, increase serum CK and AST. |
|
|
What is urobilinogen and what is it used for?
|
Product of gut bacterial action on bilirubin. Is recycled thru liver, and some is excreted in urine. Limited use in animals.
|
|
|
Urine sediment exam - how many rbcs is significant?
|
> 5 per hpf. Means haematuria, inflammation
|
|
|
Urine sediment exam - how many wbcs is significant?
|
>5-8 per hpf. More = inflammation
|
|
|
Urine sediment exam - if lots of epithelial cells, what is your next action?
|
Stain to differentiate between squamous or transitional
|
|
|
What are urinary casts?
|
Mucoprotein secreted by epithelial cells lining renal tubules and loops of Henle.
Can reflect renal damage. Many different types. |
|
|
What is the significance of hyaline urinary casts?
|
Glomerular damage. Small numbers normal.
|
|
|
What is the significance of granular urinary casts?
|
Tubular damage
|
|
|
What is the significance of cellular urinary casts?
|
Tubular damage.May progress to granular casts as the cells degenerate.
|
|
|
What is the significance of fatty urinary casts?
|
Mainly seen in cats, due to degeneration of tubular epithelial cells.
Dogs - diabetes mellitus. |
|
|
What is the significance of bilirubin crystals in dog urine?
|
Usually insignificant.
|
|
|
What is the significance of struvite crystals in dog urine?
|
Often insignificant
|
|
|
What is the significance of calcium carbonate crystals in horse urine?
|
Usually insignificant.
|
|
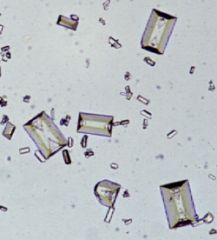
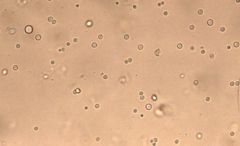
Name that urinary crystal (horse urine)
|
Calcium carbonate. Insignificant because Ca excreted in urine
|
|
Name that urinary crystal (dog)
|
Struvite - often insignificant
|
|
Name that urinary crystal (dog)
|
Bilirubin (often insignificant)
|
|
Name that urinary crystal (cat) Significance?
|
Bilirubin. Cholestatic liver disease
|
|
Name that urinary crystal (dog). Significance?
|
Ammonium biurate. Portosystemic shunt
|
|
Name that urinary crystal (cat). Significance?
|
Ammonium biurate. Portosystemic shunt
|
|
Name that urinary crystal (cat)
Significance? |
Calcium oxalate crystals, ethylene glycol poisoning
|
|
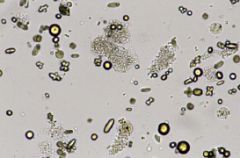
Dog urine sample - what can you see?
|
Leukocytes and bacteria
|
|
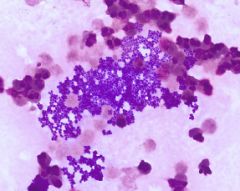
Urine sample - what can you see?
|
Degenerate neuts, cocci
|
|
Cat urine - what can you see?
|
Fat droplets
|
|
|
Define azotaemia
|
Increased urea and creatinine in blood
|
|
|
Define uraemia
|
Azotaemia and isosthenuria due to renal failure
|
|
|
Urea:
Where/how is it formed? Where is it excreted What causes level to vary? |
Formed in Liver - conversion from ammonia
Excreted by Kidney Dietary protein causes variation |
|
|
Creatinine:
Where does it come from? Where is it excreted? What does it reflect? |
Muscle creatine
Kidney Reflects total body muscle mass. Fairly constant production and excretion |
|
|
Four categories of azotaemia?
|
Prerenal
Renal Postrenal Nonrenal |
|
|
How does nonrenal azotaemia occur? What does creatinine do?
|
Increased urea production due to increased protein catabolism.
Creatinine stays normal. Increased dietary protein Increased catabolism of body tissues GIT haemorrhage Drugs Post prandial |
|
|
What causes prerenal azotaemia?
|
Decreased GFR.
Dehydration, CV disease, hypovolaemia, severe hypoalbuminaemia. Usually mild. |
|
|
What causes renal azotaemia?
|
Loss of >75% of renal nephrons.
Can be mild to marked. Usually accompanied by isosthenuria because can't maintain medullary hypertonicity. May also get increased or decreased urine production |
|
|
What causes postrenal azotaemia?
|
Obstruction or rupture of bladder or urethra.
Feline urologic syndrome Traumatic (HBC) Bladder rupture in foals parturition Urolithiasis in male ruminants |
|
|
What will happen to urine production with
a) prerenal b)renal c) postrenal azotaemia? |
Prerenal - decreased or normal
Renal - can be increased or decreased Postrenal - usually decreased |
|

Dog kidney, dipped in Lugols iodine. WHat are the black bits?
|
Glomeruli containing amyloid - renal amyloidosis
|
|
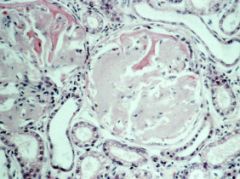
What is wrong with this glomerulus?
|
Distended with amyloid (pale pink material).
Dark pink in bowmans capsule = protein leaked from glomerular capillaries |
|
|
How can we diagnose diabetes insipidus?
|
Give ADH. DI = unresponsive to ADH so won't concentrate urine in response to ADH. Called ADH stim test
|
|
|
What is the tolerable number of casts to see in a low power field? (10x)
|
1-2. Higher indicates renal disease
|
|
|
Contrast leakage enzymes with induction enzymes (liver)
|
Leakage -ALT, AST, GLDH - cellular damage allows them to leak out hence their levels are increased in the blood. Peak early and decline over 1+ weeks. Often not increased with chronic liver damage.
Induction - ALP, GGT -drugs or cholestasis causes an increase in activity. Occurs in a day, peaks within 3-4 weeks, declines over months. |
|
|
What kind of indicator enzyme is ALT? Where does it indicate damage?
|
Leakage. Hepatocytes of dogs and cats. Usually normal in chronic liver damage, increased with acute injury.
Can get mild elevations with LOTs of different conditions e.g. glucocorticoids, GIT dz, DM... |
|
|
What kind of indicator enzyme is AST? Where does it indicate damage?
|
Leakage. Hepatocytes, red blood cells or muscle. Check CK to rule out muscle damage.
Used in largies and smallies |
|
|
What kind of indicator enzyme is GLDH? Where does it indicate damage?
|
Leakage. Liver of smallies and largies but ALT better for smallies so use that instead.
Indicates acute liver damage in largies. |
|
|
Which liver enzymes are the best indicators of cholestatic liver disease?
|
Induction enzymes - ALP and GGT
|
|
|
What kind of indicator enzyme is ALP? Where does it indicate damage?
|
Induction. Contained in
Liver Osteoblasts Intestinal epithelium Renal epithelium Placenta But intestinal and renal and placental isoenzymes have very short half lives so don't usually interfere with blood tests. |
|
|
What are the two main ALP isoenzymes and what causes increases in them?
|
B-ALP (in osteoblasts)
Young rapidly growing animals, active bone resorption, lytic or proliferative bone lesions. L-ALP (liver) Increased in cholestasis - both intrahepatic or extrahepatic. Only used in smallies. Can also get increased ALP from corticosteroids (endogenous or exogenous) |
|
|
What kind of indicator enzyme is GGT? Where does it indicate damage?
|
Induction. Contained in cell membranes of
biliary epithelium hepatocytes renal tubular cells mammary cells Get increases with -Cholestasis -Corticosteroids in dogs -Biliary duct inflammation and hyperplasia Also good indicator of colostrum absorption |
|

What is this?
What GGT level would you expect and why? What is the main problem caused by this organism |
Fasciola hepatica
Normal to mildly increased - although it is acute damage, fasciola does not primarily attack biliary epithelium. Ingest blood - anaemia. |
|
|
What serum GGT level would you expect with
a) acute sporidesmin toxicity b) boxing glove liver |
a) increased (for several months)
b) normal |
|
|
Name 5 tests of hepatic function
|
Bilirubin
Bile acids Cholesterol Ammonia Plasma proteins |
|
|
Describe the bilirubin metabolism pathway
|
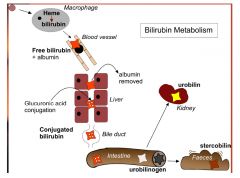
Macrophages break down rbcs, removing bilirubin from heme.
Bilirubin binds to albumin in the blood, travels to liver. Liver removes albumin and conjugates bilirubin with glucuronic acid, puts it into bile. Bile enters intestine. Some becomes urobilin - excreted in kidney. Some becomes stercobilin - excreted in faeces. |
|
|
How do we get
a) Fasting hyperbilirubinaemia? b) Haemolytic hyperbilirubinaemia? c) Hepatic hyperbilirubinaemia? d) Cholestatic hyperbilirubinaemia? e) Inflammatory hyperbilirubinaemia? |
a) Fasting - esp in horses, decreased uptake of bilirubin by hepatocytes
b) Haemolytic - haemolysis of rbcs - lots of bilirubin released, usually see anaemia too c) Hepatic - Impaired processing and cholestasis. Also see bilirubin in urine. Both free and conjugated bilirubin in blood. Can be acute or chronic liver dz. 4) Cholestatic - obstruction of bile flow, can be intra or extrahepatic. Also see in urine. 5) Inflammatory - don;t know, just get it with severe inflammation eg pneumonia, peritonitis, endocarditis w Ecoli or Staph intermedius |
|
|
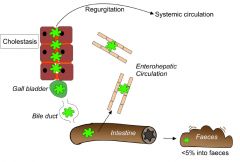
Describe bile acid metabolism
|
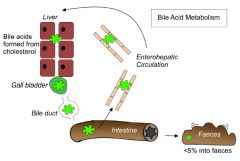
Bile acids formed in liver from cholesterol.
Put into gall bladder, excreted via bile duct into intestine. From intestine, 95% reabsorbed into enterohepatic circulation, go back to liver. Remaining 5% excreted in faeces. |
|
|
Four functions of bile acids
|
Eliminate cholesterol from the body
Driving bile flow to eliminate hepatic catabolites Emulsifying lipids in the intestine Reducing bacteria in the intestine and bile duct |
|
|
What are three things that could cause increased serum bile acids?
|
Portosystemic shunt
Reduced functional hepatic shunt Cholestasis |
|
|
How does reduced hepatic mass result in increased serum bile acids?
|
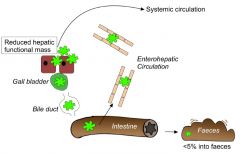
When the bile acids are reabsorbed from the intestine to go back to the liver, the liver cannot keep up and so bile acids build up in the systemic circulation
|
|
|
How does cholestasis result in increased serum bile acid concentration?
|
Cholestasis causes a buildup and back flow of serum bile acids (and cholesterol as liver can't make more bile acids either) into the systemic circulation
|
|
|
Cholesterol increases in cholestasis, hypothyroidsim, diabetes mellitus and nephrotic syndrome? When does it decrease?
Where is most cholesterol synthesized and excreted in the body? |
Chronic liver disease, because the liver synthesizes most cholesterol. Excreted in bile acids.
|
|
|
Describe the pathway of ammonia in the body
|
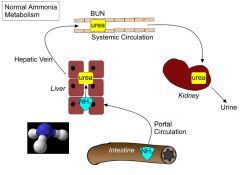
Absorbed from intestines from protein breakdown. Enters liver - liver converts it to urea (BUN = blood urea nitrogen). Urea is excreted via the kidney.
|
|
|
When do we see increased levels of ammonia in the blood? (2)
What might we see a decrease in? |
Portosystemic shunt
Loss of 60-70% liver mass BUN (urea) Can cause hepatic encephalopathy |
|
|
What effect on plasma proteins will loss of 70-80% of liver function have?
|
Hypoalbuminaemia
Globulins either normal or increased (compensatory) Coagulation factors may also be decreased |
|
|
What regulates basal metabolism?
|
Thyroid gland
|
|
|
Describe the thyroid hormone production pathway
|
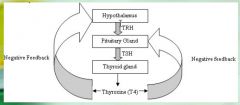
Hypothalamus produces TRH (thyroid releasing hormone) - pituitary produces TSH (thyroid stimulating hormne) - thyroid gland produces T4 - negative feedback on both Hypothalamus and Pituitary gland
|
|
What are the two main causes of primary hypothyroidism in dogs? Which one is this?
|
Idiopathic thyroid atrophy
Lymphocytic thyroiditis |
|
|
What are the two causes of secondary hypothyroidism?
|
Cystic Rathke's pouch (german shepherds)
Pituitary tumour |
|
|
What is Euthyroid sick syndrome?
|
Sickness or medications cause low T4, but dog is not hypothyroid.
e.g. DM, renal failure, liver disease, cushings, infxns, anaesthetics, phenobarb, diazepam, corticosteroids, Trim-sulf |
|
|
What can cause hypothyroidism in largies? (2)
|
Brassicas
Trim-sulf |
|
|
What causes hyperthyroidism in cats?
|
Thyroid adenomatous hyperplasia
|
|
|
What abnormalities would you see on a haemogram of a cat with hyperT?
Biochem? |
Normal to mild erythrocytosis
Stress leukogram (Nophilia, Eopenia, Lymphopenia) Mild to moderate increase in ALP, AST, ALT, sometimes bilirubin - reasons for biochem changes unknown. |
|
|
WHat concurrent disease can be masked by Hyperthyroidism and how?
|
Renal insufficiency - because it increases GFR. Tx for HyperT can worsen the renal problem
|
|
|
Describe the pathway that leads to the release of cortisol
|
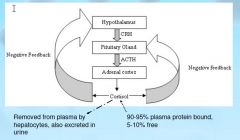
Hypothalamus releases CRH (corticotropin-releasing hormone) - Pituitary releases ACTH (adrenocorticotropic hormone). ACTH acts on the adrenal cortex - causes release of cortisol. Cortisol have negative feedback effect on hypothalamus and pituitary.
|
|
|
What are the three types of cushings and their prevalence?
|
Pituitary dependent - 85%, both adrenals enlarged
Adrenal - 15% - one adrenal enlarged Iatrogenic 5% - both adrenals tiny |
|
|
What is the treatment for
a) pituitary cushings b) adrenal cushings? |
Pit- medical (Mitotane or Trilostane)
Adr - sx |
|
|
What would you see in a wbc haemogram for a dog with cushings?
|
Leukocytosis and stress leukogram
Nophilia (impaired emigration from capillaries) Mocytosis (impaired emigration from capillaries) Eopenia (BM sequestration) Lymphopenia (steroid induced lympholysis) |
|
|
4 tests for cushings?
|
Urinary cortisol:creatinine (normal = not cushings. Increased = stress or cushings)
ACTH stim test (only test that detects iatrogenic cushings, and only test that can be used for monitoring therapy) LDDST Ultrasound is the shizzle. |
|
|
What causes equine cushings-like disease?
What are two major consequences of the disease? What leukogram would you expect? |
Hyperplasia/adenoma/hypertrophyof the pituitary oars intermedia.
Diabetes mellitus, laminitis Stress leukogram |
|
|
What is primary hypoadrenocorticism?
|
= Addisons dz.
Likely immune mediated but unknown. Destruction of adrenal cortex - decreased production of glucocorticoids and mineralocorticoids. |
|
|
What causes secondary hyperadrenocorticism?
|
Decreased secretion of ACTH to stimulate adrenal gland. Caused by pituitary tumour or abrupt removal of treatment for cushings.
|
|
|
What are the three most common clinical signs of hypoadrenocorticism (Addisons)?
|
Lethargy, anorexia, vomiting
|
|
|
Addisons disease - what would you see on a haemogram?
|
Mild non-regen anaemia - possibly masked by dehydration
Anti-stress leukogram (opposite) |
|
|
What screening test would you use for Addisons disease?
|
ACTH stim (get no increase in cortisol)
|
|
|
Differentiate type 1 from type 2 diabetes mellitus. Which is most common in dogs? Cats?
|
Type 1 - specific destruction of pancreatic beta cells - deficiency in insulin production. Dogs.
Type 2 - defect in insulin secretion or receptors. Cats |
|
|
How do we diagnose Diabetes mellitus?
|
1. Persistent hyperglycaemia despite fasting
2. Glucosuria (but stressed cats may have small amt in urine anyway) 3. Fructosamine |
|
|
What is fructosamine?
|
A protein that has glucose attached to it. It's concentration in plasma indicates the average glucose concentration in plasma over the lifetime of the protein.
Use it to distinguish hyperglycaemia due to stress from hyperg due to diabetes mellitus. Also use to test treatment efficacy. |
|
|
What is an insulinoma? What does it do?
|
Pancreatic beta cell neoplasm. Secretes lots of insulin - hypoglycaemia, weakness, collapse, seizures. Confirm by testing blood glucose and insulin - high insulin with low glucose = insulinoma
|
|
|
Differentials for high serum Ca and high serum P04?
|
Vit D toxicity
Bone lysis - osteosarcoma or osteomyelitis Rapid bone growth in young animals |
|
|
Differentials for high serum Ca and low/normal serum P04?
|
Primary hyperparathyroidism
Hypercalcaemia of malignancy |
|
|
Describe the pathway for bovine ketosis
|
High energy demand with insufficient energy intake - negative energy balance - mobilisation of fat - gluconeogenesis and fatty acid oxidation - both of these processes require OAA, not enough available - result is fatty acids only partially oxidised - ketone bodies produced (acidic) - metabolic acidosis
|
|
|
What is creatinine kinase?
|
CK = muscle leakage enzyme. Indicator of acute muscle damage. Short half life - does not last as long as AST so more indicative of acute damage.
|
|
|
Myoglobinuria in largies - what does it mean?
|
Severe active muscle necrosis
|
|
|
Hyperkalaemia in largies - how does this indicate muscle damage?
|
Leaked out of damaged cells
|
|
|
How can downer cows develop muscle damage and renal failure?
What are two good prognositc indicators (lab tests) |
Pressure - ischaemic necrosis of muscles
Dehydration - decreased renal perfusion Serum urea and AST |
|
|
Exercise, excitement and difficult venipuncture cause mild increases in CK - why?
|
Cause muscle damage
|
|
|
Quantify polyuria
|
>50ml/kg/day
|
|
|
Quantify polydipsia
|
>100ml/kg/day
|
|
|
Where is ADH produced?
In response to what two things? What does it do? |
Pituitary gland.
Decreased blood volume, increased osmolality Increases tubule permeability to water so increases reabsorption |
|
|
What is primary polydipsia? How would you confirm it?
|
Psychogenic polydipsia. PU is secondary.
Confirm by demonstrating adequate renal concentrating ability and ruling out other causes of PU/PD |
|
|
How does renal failure cause PU/PD
|
Loss of medullary concentration gradient - can't concentrate urine
|
|
|
How does liver failure cause PU/PD
|
Mechanism uncertain! Possibly hepatic encephalopathy
|
|
|
How does DM cause PU/PD?
|
Osmotic diuresis from glucose in urine
|
|
|
How does Central Diabetes Insipidus cause PU/PD?
|
Lack of ADH production or secretion - no stimulus to increase permeability of renal tubles to water so kidneys can't concentrate urine
|
|
|
How does Nephrogenic Diabetes Insipidus cause PU/PD?
|
Lack of response to ADH - no stimulus to increase permeability of renal tubles to water so kidneys can't concentrate urine
|
|
|
How does cushings disease cause PU/PD?
|
Inhibits both secretion and action of ADH - no stimulus to increase permeability of renal tubles to water so kidneys can't concentrate urine
|
|
|
How does Addison's disease cause PU/PD?
|
Decreased aldosterone - decreased Na - no medullary conc gradient (medullary washout)
|
|
|
How does Hyperthyroidism cause PU/PD
|
We don't know.
|
|
|
How does pyelonephritis cause PU/PD?
|
Renal pelvic infection or
inflammation can disrupt the medullary counter current mechanism - renal tubules become unresponsive to ADH - infection/inflammation can lead to renal failure if prolonged |
|
Whats this stuff?
|
Ultrasound gel
|
|
Whats this stuff?
|
Smeared nuclear debris amongst neutrophils - NOT fungal hyphae!
|
|
What kind of inflammation?
|
Acute septic - lots of degen neuts, can see bacteria inside nauts
|
|
Cutology from a cutaneous lump on a cat - diagnosis?
|
Feline leprosy.
Lots of large epithelioid macrophages, and negatively staining mycobacteria |
|
Cutaneous mass FNA - diagnosis?
|
Lipoma (chicken wire)
|
|
FNA skin mass - diagnosis?
|
Follicular cyst (epidermal inclusion cyst)
Can see cholesterol crystals from crystallisation of cholesterol from cell membranes. Stratified squamous epithelium, keratinised squames |
|
Classify the cells
|
Epithelial
|
|
FNA from lump near dog anus - diagnosis?
|
Perianal gland adenoma
|
|
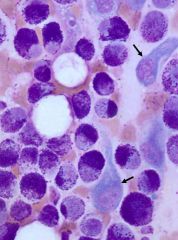
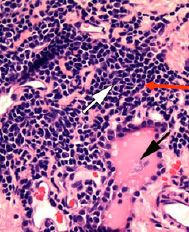
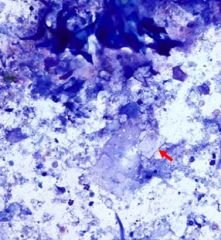
FNA skin lump on dog - diagnosis? What cells are the arrows pointing to?
|
Mast cell tumour
Mesenchymal cells - not neoplastic |
|
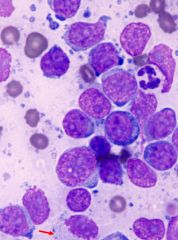
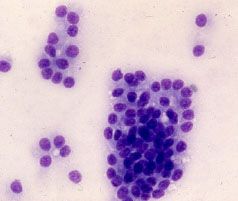
Aspirate from enlarged LN of a dog - diagnosis?
|
Lymphosarcoma - many immature blasts and mitotic figures
|
|
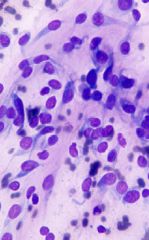
Classify the cell type
|
Mesenchymal (these ones are neoplastic)
|
|
|
How can we differentiate between active fibroblasts and neoplastic mesenchymal cells?
|
Difficult to diff on cyto - take histo and submit to lab
|
|
Mammary tumour - benign or malignant?
|
Benign
|
|
Mammary tumour - benign or malignant?
|
Malignant
|

