![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
Normal Blood Gas Levels:
pH PCO2 HCO3 PO2 SaO2 |
pH 7.35-7.45
PCO2 35-45 mmHg HCO3 22-26 mEq/L PO2 80-100 mmHg (breathing room air) SaO2 90-100% |
|
|
The most common clinical manifestations indicative of inadequate ventilation are:
|
Tachycardia (100+)
Tachypnea (24+) Anxiety Restlessness or confusion Use of accessory breathing muscles Change in cognition or response Increased blood pressure |
|
|
Name the Respiratory Nursing Diagnosis for the following related factors:
Imbalance between oxygen supply and demand |
activity intolerance
|
|
|
Name the Respiratory Nursing Diagnosis for the following related factors:
Fatigue; excessive secretions; pain; immobility; neuromuscular disease; chronic obstructive pulmonary disease |
Inefective airway clearance
|
|
|
Name the Respiratory Nursing Diagnosis for the following related factors:
Depressed airway protective mechanisms; presence of artificial airway; enteral feedings; neuromuscular disease |
Aspriation, risk for
|
|
|
Name the Respiratory Nursing Diagnosis for the following related factors:
Immobility; fatigue; pain; nueromuscular impairment; chronic respiratory disease; pharmacological agents |
Ineffective breathing patterns
|
|
|
Name the Respiratory Nursing Diagnosis for the following related factors:
Ventilation/perfusion imbalance; hypoventilation, COPD; airway obstruction; heart failure; pulmonary edema |
Impaired gas exchange
|
|
|
Name the Respiratory Nursing Diagnosis for the following related factors:
Disturbed sleep pattern |
obstructive airway (sleep apnea)
|
|
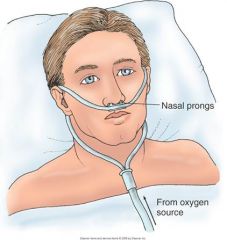
Low flow systems:
What is this? |
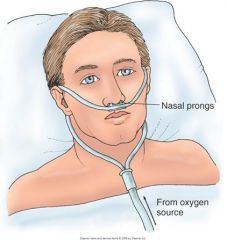
better tolerated and may be humidified but often not if run @ less than 5 L/min
The nasal cannula, or nasal prongs, is used at flow rates of 1 to 6 L/min. Approximate oxygen concentrations of 24% (at 1 L/min) to 44% (at 6 L/min) can be achieved. Flow rates greater than 6 L/min do not significantly increase oxygenation because the anatomic dead space (places where air flows but the structures are too thick for gas exchange; includes the oral and nasal cavities, pharynx, trachea, mainstem bronchi, secondary bronchi, and smaller airways down to the alveolar ducts) is full. In addition, high flow rates increase mucosal irritation. With the use of a nasal cannula, an effective oxygen concentration can be delivered to both nose breathers and mouth breathers. The nasal cannula is frequently used for chronic lung disease and for long-term maintenance of clients with other illnesses. The client who retains carbon dioxide rarely receives oxygen at a rate higher than 2 to 3 L/min because of the concern for losing the drive to breathe, increasing the risk for apnea or respiratory arrest. The nurse places the nasal prongs in the nostrils, with the openings facing the client. |
|
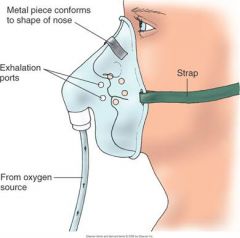
Low flow systems:
What is this? |
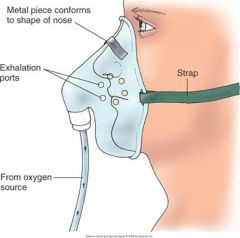
Delivers 35 to 55 % O2 at flows of 5 to 12 L/min
**Must never be used at flows less than 5 L/min to prevent rebreathing of CO2 A simple face mask is used to deliver oxygen concentrations of 40% to 60% for short-term oxygen therapy or in an emergency. A minimum flow rate of 5 L/min is needed to prevent the rebreathing of exhaled air. The nurse gives special attention to skin care and to the proper fitting of the mask so that inspired oxygen concentration is maintained. |
|
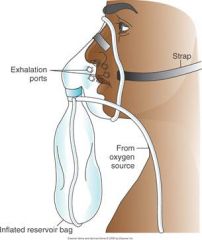
Low flow systems:
What is this? |
A partial rebreather mask provides oxygen concentrations of 60% to 75%, with flow rates of 6 to 11 L/min. It consists of a mask with a reservoir bag but no flaps. The client first rebreathes one third of the exhaled tidal volume, which is high in oxygen, thus providing a high fraction of inspired oxygen (Fio2). The nurse ensures that the bag remains slightly inflated at the end of inspiration; otherwise, the client will not be getting the desired oxygen prescription. If needed, the nurse calls the respiratory therapist for assistance.
|
|

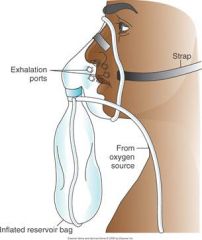
Low flow systems:
What is this? |
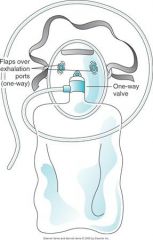
NON-REBREATHER MASK. A non-rebreather mask provides the highest concentration of the low-flow systems and can deliver an Fio2 greater than 90%, depending on the client's breathing pattern. The non-rebreather mask is used most often with deteriorating respiratory status who might soon require intubation.
The non-rebreather mask has a one-way valve between the mask and the reservoir and two flaps over the exhalation ports. The valve allows the client to draw all needed oxygen from the reservoir bag, and the flaps prevent room air from entering through the exhalation ports. During exhalation, air leaves through these exhalation ports while the one-way valve prevents exhaled air from re-entering the reservoir bag. It is crucial for the nurse to ensure that the valve and flaps are intact and functional during each breath. Some manufacturers include only one flap on the mask, or one of the exhalation flaps may be removed for safety purposes. If the oxygen source should fail or be depleted when both flaps are in place, the client would not be able to inhale room air. The flow rate is maintained at a high-enough level to keep the bag inflated during inhalation. The nurse assesses for this safety feature. |
|
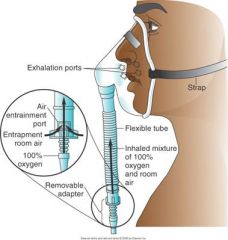
High Flow Systems:
What is this? |
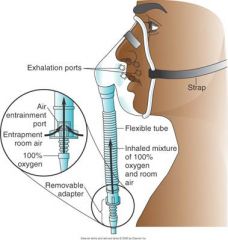
VENTURI MASK. The Venturi mask (commonly called Venti mask) delivers the most accurate oxygen concentration. Its operation is based on a mechanism that pulls in a specific proportional amount of room air for each liter flow of oxygen. An adaptor is located between the bottom of the mask and the oxygen source. Adaptors with holes of different sizes allow only specific amounts of air to mix with the oxygen. Precise delivery of oxygen results. Each adaptor also specifies the flow rate to be used; for example, to deliver 24% of oxygen, the flow rate must be 4 L/min. Another type of Venturi mask has one adaptor with a dial that the nurse uses to select the amount of oxygen desired. Humidification is not necessary with the Venturi mask. The Venturi system is best for the client with chronic lung disease because it delivers a precise oxygen concentration.
|
|

High Flow Systems:
What is this? |

A face tent fits over the chin, with the top extending halfway across the face. The oxygen concentration varies, but the face tent, instead of a tight-fitting mask, is useful for facial trauma or burns.
|
|

High Flow Systems:
What is this? |

An aerosol mask is used when high humidity is required after extubation or upper airway surgery or for thick secretions.
|
|

High Flow Systems:
What is this? |
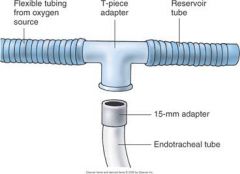
The tracheostomy collar can be used to deliver high humidity and the desired oxygen to the client with a tracheostomy.
A special adaptor, called the T-piece, can be used to deliver any desired Fio2 to the client with a tracheostomy, laryngectomy, or endotracheal tube. The flow rate is regulated so that the aerosol does not disappear on the exhalation side of the T-piece. |
|
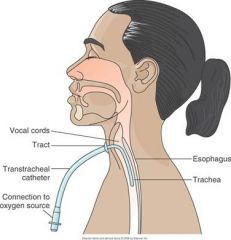
What type of oxygen therapy is this?
|
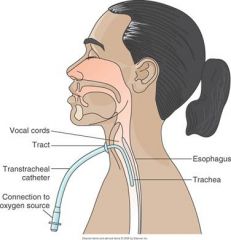
TRANSTRACHEAL OXYGEN THERAPY
Transtracheal oxygen (TTO) is a long-term method of delivering oxygen directly into the lungs. The physician passes a small, flexible catheter into the trachea via a small incision with the use of local anesthesia. TTO allows better compliance and avoids the irritation that nasal prongs cause. Clients also report it to be more cosmetically acceptable. A TTO team provides formal client education, including the purpose of TTO and care of the catheter. The physician prescribes a TTO flow rate for rest and for activity and a flow rate for the nasal cannula, to be used when the TTO catheter is being cleaned. The average client will have a 55% reduction in required oxygen flow at rest and a 30% decrease with activity. |
|
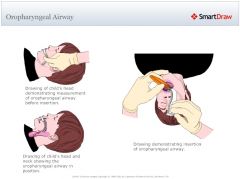
Inserting an Oropharyngeal AIrway
|
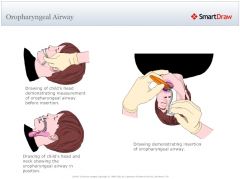
http://www.youtube.com/watch?v=SvoJfxRbpkg&playnext=1&list=PLFB148F69B3C4AF71&feature=results_main
|
|

Inserting a Nasopharyngeal Airway
|

http://www.youtube.com/watch?v=En2sXsOLzCs&list=PLFB148F69B3C4AF71
|

