![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
list three indications for performing semen analysis
|
evaluation of male infertility
select donors fro therapeutic insemination monitor the sucess of surgical procedures such as varicocelectomy and vasectomy |
|
|
a patient collecting semen should remain abstinent for a fairly strict period of ??days; he should transport the semen sample to the laboratoty within ??hours
|
3 days but not more than 5 days
1 hour of collection |
|
|
what is the normal pH of semen?
|
7.2 to 7.8;
acute prostatitis or epididymitis may raise the pH above 8.0 and urine can lower it to below 7.0 |
|
|
normal sperm motility is considered to be greater than ??
|
50%
there is a grading scale from 0-4 for assessing motility; a score of 2 is normal |
|
|
what are the two methods to detect sperm antibodies, and what type of antibody is clinically most significant?
|
sperm antibodies can be detected by a direct or indirect mixed aggutination reaction or by immunobead assay;
the agglutination reaction can pick up IgG or IgA and the immunobead assay can pick up IgG, IgA or IgM; IgA is the most clinically significant |
|
|
which common subunit is found in FSH, LH and TSH, and which subunit confersfunctional specificity?
|
the alpha subunit is common
the beta subunit confers specificity |
|
|
what is the typical laboratory profile in an infertile male with a 47XXY karyotype?
|
Klinefelter's syndrome
testosterone is decreased and the normal pituitary gland secretes excess FSH and LH because it receives no negative feedback in the form of inhibin from the testes |
|
|
what subunits do most immunometric assays for HCG measure, and when does HCG reach a maximum in a normal pregnancy
|
the sandwich assays usually measure both the free beta-subunit, which is specific for HCG and intact HCG which contains both the alpha and beta subunits;
the maximum HCG level is usually reached at 10 weeks gestation |
|
|
a blighted ovum is indicated by what levels of estradiol and progesterone?
|
estradiol of <200ng/mL and a progesterone of <15ng/mL indicate a blighted ovum
|
|
|
what anticonvulsant is associated with an increased risk of neural tube defects?
|
valproate
|
|
|
assisted reproductive technology (ART), hormones to stimulate specific physiologic processes; state the function of the following medications
GnRH analog: human menopausal gonadotropin (HMG): HCG bolus: |
GnRH analog supresses normal FSH and LH synthesis and secretion;
HMG has predominantly FSH activity, so it will stimulate follicular growth of several follicles simultaneously HCG bolus acts as the LH surge of the midcycle and simulates ovulation |
|
|
AFP concentrations peak at 12-14 weeks gestation yet maternal screening is performed in the second trimester; why is this
|
fetal AFP diffuses across the amniotic membrane into the amniotic fluid and then from the amniotic fluid into the maternal serum (MS);
AFAFP levels peak at 13-14 weeks gestation, but due to changes in the transfer to MS and internal maternal clearance of AFP, the MSAFP levels increase by approximately 15% per gestation week in second trimester |
|
|
5 clinical factors in determining MSAFP multiples of the medium (MoM) and how each affects the MSAFP?
|
maternal weight: MSAFP decreases with increasing weight
Race: blacks have 10-15% higher than whites IDDM: levels are 20% lower than in the general population Multiple gestation: MSAFP is proportional to the number of fetuses Gestational age: MSAFP increases 15% per week in the second trimester |
|
|
what is the profile of maternal serum markers in fetal Down syndrome?
MSAFP: Unconjugated estriol(uE3): HCG: |
MSAFP: low by about 25%
Unconjugated estriol(uE3):low HCG:high, usually 2.0MoM |
|
|
A 23 year old woman who has taken no prenatal vitamins has a MSAFP of her singleton fetus that is 6.8 multiple of the mean(MoM). The ultrasound is abnormal. What is the most likely diagnosis?
|
with a MoM of 6.8, it is likely to be anencephaly
|
|
|
What lecithin/ spingomyelin (L/S) ration indicates fetal lung maturity?
|
an L/S ratio of 2.0 is indicative of fetal lung maturity
|
|
|
True or false. The primary risk to the fetus in the hemolytic disease of the newborn is the accumulation of unconjugated bilirubin in the central nervous system (kernicterus).
|
False, the placenta normally removes unconjugated bilirubin and it thus appears in th amniotic fluid; anemia is the primary risk to the fetus; after delivery both anemia and kenicterus threaten the neonate
|
|
|
Briefly outlined are commonly use status or diagnosis in premature rupture of membranes.
|
To detect amniotic fluid (AF) and the posterior vaginal pole, a sample of fluid is aspirated and placed on nitrazine-impregnated paper. An alkaline pH of 7.0-7.5 (recall that AF is an alkaline fluid, while vaginal secretions or acidic) will turn the paper tape blue color and indicate rupture of amnionic membranes.
|
|
|
Although the lecithin/ spingomyelin (L/S) is frequently measured by thin-layer chromatography to assess fetal lung maturity, this method has several disadvantages. List them?
|
The L/S ratio method is slow,labor intense, and only 25% sensitive in predicting respiratory distress syndrome at the level of 2.0 . Vaginal secretions and meconium both interfere with measurement.
|
|
|
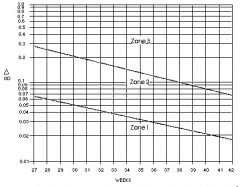
The Liley Curve
A result in Zone I indicates mild or no disease. Fetuses in zone I are usually followed with amniocentesis every 3 weeks. A result in zone II indicates intermediate disease. Fetuses in low Zone II are usually followed by amniocentesis every 1-2 weeks. A result above the middle of Zone II may require transfusion or delivery. |

