![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
77 Cards in this Set
- Front
- Back

|
1
|
|

|
2
|
|

|
3
|
|

|
4
|
|

|
5
|
|

|
6
|
|

|
7
|
|

|
8
|
|

|
9
|
|

|
10
|
|

|
11
|
|
|
12
|
|

|
13
|
|

|
14
|
|

|
15
|
|

|
16
|
|

|
17
|
|

|
18
|
|

|
19
|
|

|
20
|
|

|
21
|
|
|
List three ways organisms can get into the lungs:
How does this affect the infection's appearance on imaging? |
-Microorganisms responsible for producing pneumonia enter the lung and cause infection by three potential routes: via the tracheobronchial tree, via the pulmonary vasculature, or via direct spread from infection in the mediastinum, chest wall, or upper abdomen.
-Infection via the tracheobronchial tree is generally secondary to inhalation or aspiration of infectious microorganisms and can be divided into three subtypes: lobar pneumonia, lobular or bronchopneumonia, and interstitial pneumonia. -Certain organisms will typically produce one of these three patterns, although there may be considerable overlap. -The spread of infection to the lung via the pulmonary vasculature usually occurs in the setting of systemic sepsis. -The pattern of parenchymal involvement is patchy and bilateral. -The lung bases are most severely involved, because blood flow is greatest in the dependent portions of the lungs. -Pulmonary infection from direct spread usually results in a localized parenchymal process adjacent to an extrapulmonary source of infection. -If an organism causes extensive parenchymal necrosis, abscess formation may result. |
|
|
Explain the difference between lobar pneumonia, bronchopneumonia, and interstitial pneumonia:
|
-Each is usually secondary to aspiration of microorganisms (not hematogenous)
-Lobar pneumonia is typical of pneumococcal pulmonary infection. -In this pattern of disease, the inflammatory exudate begins within the distal airspaces. -The inflammatory process spreads via the pores of Kohn and canals of Lambert to produce nonsegmental consolidation. -If untreated, the inflammation may eventually involve an entire lobe. -Because the airways are usually spared, air bronchograms are common and significant volume loss is unusual. -Bronchopneumonia is the most common pattern of disease and is most typical of staphylococcal pneumonia. -In the early stages of bronchopneumonia, the inflammation is centered primarily in and around lobular bronchi. -As the inflammation progresses, exudative fluid extends peripherally along the bronchus to involve the entire pulmonary lobule. -Radiographically, multifocal opacities that are roughly lobular in configuration produce a “patchwork quilt” appearance because of the interspersion of normal and diseased lobules. -Exudate within the bronchi accounts for the absence of air bronchograms in bronchopneumonia. -With coalescence of affected areas, the pattern may resemble lobar pneumonia. -In interstitial pneumonia, seen in viral and mycoplasma infection, there is inflammatory thickening of bronchial and bronchiolar walls and the pulmonary interstitium. -This results in a radiographic pattern of airways thickening and reticulonodular opacities. -Air bronchograms are absent because the alveolar spaces remain aerated. -Segmental and subsegmental atelectasis from small airways obstruction is common. |
|
|
Which patients develop pulmonary infections via hematogenous spread?
What does it look like on imaging? |
-The spread of infection to the lung via the pulmonary vasculature usually occurs in the setting of systemic sepsis.
-The pattern of parenchymal involvement is patchy and bilateral. -The lung bases are most severely involved, because blood flow is greatest in the dependent portions of the lungs. |
|
|
What is the typical radiographic appearance of acute pneumococcal pneumonia?
How long does it take to clear radiographically? |
-The typical radiographic appearance of acute pneumococcal pneumonia is lobar consolidation.
-Air bronchograms are usually evident. -Pneumococcal pneumonia tends to begin in the lower lobes or the posterior segments of the upper lobes. Initially there is involvement of the terminal airways, but rather than remaining localized to this site, there is rapid development of an airspace inflammatory exudate. -In children, pneumococcal pneumonia may present as a spherical opacity (“round pneumonia”) simulating a parenchymal mass. -Cavitation in pneumococcal pneumonia is rare -Uncomplicated parapneumonic effusion or empyema may be seen in up to 50% of patients -With appropriate therapy, complete clearing may be seen in 10 to 14 days. -In older patients or those with underlying disease, complete resolution may take 8 to 10 weeks. |
|
|
What is the typical radiographic appearance of acute staphylococcal pneumonia?
|
-S aureus typically produces a bronchopneumonia and appears radiographically as patchy opacities.
-In severe cases, the opacities may become confluent to produce lobar opacification. -Because the inflammatory exudate fills the airways, air bronchograms are rarely seen. -In adults, the process is often bilateral and may be complicated by abscess formation in 25% to 75% of patients. -In patients who develop pulmonary infection from hematogenous seeding, one sees multiple bilateral poorly defined nodular opacities that eventually become more sharply defined and cavitate. -Parapneumonic effusion and empyema are common. -Pneumatocele formation is common in children and may lead to pneumothorax. |
|
|
How can you tell a pneumatocele from a lung abscess?
|
Pneumatoceles may be distinguished from abscesses by their thin walls, rapid change in size, and tendency to develop during the late phase of infection
|
|
|
Describe the radiographic and CT features of pulmonary anthrax:
|
-Naturally occurring inhalational anthrax is rare; however, anthrax has been used as an agent of bioterrorism
-The primary radiographic manifestations of inhalational anthrax are related to the underlying pathology of hemorrhagic lymphadenitis and mediastinitis accompanied by hemorrhagic pleural effusions. -Conventional radiographs demonstrate mediastinal widening, hilar enlargement, and often pleural effusion. -Frank areas of consolidation are not usually present, but peribronchial opacities may be seen. -CT scans of recent bioterrorism victims demonstrated high-attenuation lymphadenopathy and pleural effusions secondary to hemorrhage. -CT scans may show extensive adenopathy in the setting of normal radiographs and should be obtained if the suspicion of anthrax is high |
|
|
What are the typical imaging features of gram negative bacterial pneumonia?
|
-Involvement is usually bilateral and multifocal, and the lower lobes are most frequently affected.
-Abscess formation and cavitation are relatively common. -Parapneumonic effusion is common and is often complicated by empyema formation. |
|
|
What are the typical imaging features of legionella pneumonia?
|
-The characteristic radiographic pattern is airspace opacification, which is initially peripheral and sublobar.
-In some patients, the airspace opacities appear as a round pneumonia. -The infection progresses to lobar or multilobar involvement despite the initiation of antibiotic therapy. -At the peak of disease, the parenchymal involvement is usually bilateral. -Pleural effusions are seen in approximately 30% of patients. -Cavitation is not seen except in the immunocompromised patient -The radiographic resolution of pneumonia is often prolonged and may lag behind symptomatic improvement. |
|
|
Which pulmonary segments are affected by aspiration in a supine position?
What about aspiration in the erect position? |
-When aspiration occurs in the supine position, it is the posterior segments of the upper lobes and superior segments of the lower lobes that are predominantly involved, whereas aspiration in the erect position leads to involvement of basal segments of the lower lobes.
|
|
|
What are the typical imaging features of thoracic actinomycosis?
|
-The radiographic pattern of actinomycosis is often indistinguishable from that of nocardiosis.
-Findings consist of nonsegmental airspace opacities in the periphery of the lower lobes. -In some cases, the infection manifests as a localized masslike opacity that mimics bronchogenic carcinoma. -If therapy is not instituted, a lung abscess may develop. -Thoracic actinomycosis is characterized by its ability to spread to contiguous tissues without regard for normal anatomic barriers. -Extension into the pleura will cause empyema, while chest wall involvement is characterized by osteomyelitis of the ribs and chest wall abscess. -Involvement of the ribs is seen as wavy periosteal reaction or lytic rib destruction. -If the pleuropulmonary disease becomes chronic, extensive fibrosis may be seen. -Rarely, the disease is disseminated and a miliary pattern is seen. |
|
|
What are the typical imaging features of pulmonary mycoplasma infection?
|
-In the early stages of infection, interstitial inflammation leads to a fine reticular pattern on the chest radiograph.
-This may progress to patchy segmental airspace opacities, which may coalesce to produce lobar consolidation. -CT of mycoplasma pneumonia usually appears as patchy airspace opacities with a tree-in-bud appearance that reflects infectious bronchiolitis. -The process is often unilateral and tends to involve the lower lobes. -Pleural effusion may be seen in the consolidative form of disease and occurs most commonly in children. -Lymph node enlargement is uncommon but may be seen in children. -Radiographic resolution may require 4 to 6 weeks. |
|
|
What are the types of pulmonary tuberculosis?
|
-Two principal forms of tuberculous pulmonary disease are recognized clinically and radiographically: primary tuberculosis (TB) and “reactivation” or postprimary disease.
-In primary infection, the parenchymal disease and adenopathy may completely resolve, or there may be a residual focus of scarring or calcification. -The disease will be contained by the granulomatous response and recur years later (reactivation or postprimary TB) in the setting of weakened host defenses from aging, alcoholism, diabetes, cancer, or HIV infection. |
|
|
What is progressive primary TB?
|
In some situations, usually in infants under the age of 1 year or immunocompromised patients, local primary parenchymal disease progresses and is termed progressive primary TB.
|
|
|
How does primary tuberculosis infection present on imaging?
|
-Most patients with primary TB are asymptomatic and have no radiographic sequelae of infection.
-If the patient is symptomatic, a nonspecific focal pneumonitis occurs and is seen as small, ill-defined areas of segmental or lobar opacification -The parenchymal consolidation may mimic a bacterial pneumonia, but the clinical and radiographic course is much more indolent. -Lower lobes are affected moreso than upper lobes. -Cavitation is uncommon -Pleural effusions can develop (10%) -Hilar and paratracheal adenopathy is common (95%) -In most patients, the bacilli are phagocytized and killed by alveolar macrophages, and the parenchymal consolidation heals without sequelae. -BUT, If the bacilli overcome the immune response of the host, an inflammatory focus is established. -The macrophages then aggregate to form granulomas with caseous necrosis -The granulomas are usually well-formed by 1 to 3 weeks after infection -When parenchymal granulomas calcify, they're called a Ghon lesion. -When Ghon lesions are associated with calcified nodes, it's called a Ranke complex. -During the primary tuberculous infection, there is hematogenous dissemination of the organism to regions with a high partial pressure of oxygen; these include the lung apices, renal medullae, and bone marrow. -This can show up as a miliary pattern on imaging -These microscopic foci are clinically silent and serve as a source of reactivation disease |
|
|
What is a Ghon lesion? What is a Ranke complex?
|
-When parenchymal granulomas of primary TB calcify, they're called a Ghon lesion.
-When Ghon lesions are associated with calcified nodes, it's called a Ranke complex. |
|
|
What are the calcified granulomas of primary TB called? What about the calcified nodes?
|
Ghon lesion
Ranke complex=Ghon lesion + calcified nodes |
|
|
Is miliary TB part of a primary or postprimary infection?
|
Either, it can occur whenever the organism undergoes hematogenous spread.
|
|
|
How do postprimary TB patients present clinically?
|
Postprimary TB patients often present with cough and constitutional symptoms, including chills, night sweats, and weight loss.
|
|
|
What are imaging features of postprimary TB?
|
-Reactivation tends to occur in the apical and posterior segments of the upper lobes and the superior segments of the lower lobes (rare in anterior segments of the upper lobes--unlike histo)
-Ill-defined patchy and nodular opacities are commonly seen. -Cavitation is an important radiographic feature of postprimary infection and usually indicates active and transmissible disease -The cavitary focus may lead to transbronchial spread of organisms and result in a multifocal bronchopneumonia. -Erosion of a cavitary focus into a branch of the pulmonary artery can produce an aneurysm (Rasmussen aneurysm) and cause hemoptysis. -With appropriate antimicrobial treatment, the disease is usually controlled by a granulomatous response. -Parenchymal healing is associated with fibrosis, bronchiectasis, and volume loss (cicatrizing atelectasis) in the upper lobes. |
|
|
What is a Rasmussen aneurysm?
|
Erosion of a cavitary focus of TB into a branch of the pulmonary artery, causing an aneurysm
-This is a cause of hemoptysis. |
|
|
What's it called when a cavitary TB focus erodes into a pulmonary artery?
|
Rasmussen aneurysm
|
|
|
What are causes of hemoptysis in TB patients?
|
Hemoptysis may be secondary to bronchiectasis, mycetoma formation in an old tuberculous cavity, erosion of a cavitary lesion into a pulmonary artery, or erosion of a calcified peribronchial lymph node (broncholith) into a bronchus.
|
|
|
What radiographic feature indicates active TB infection?
|
Cavitation is an important radiographic feature of postprimary infection and usually indicates active and transmissible disease
|
|
|
Describe the imaging appearance of nontuberculous mycobacterial infections:
|
-Disease in nonimmunocompromised patients typically affects patients with underlying COPD.
-The radiographic features are often indistinguishable from those of reactivation TB, with chronic fibrocavitary opacities involving the upper lobes. -While cavitation is common, pleural effusion, lymph node enlargement, and miliary spread are distinctly unusual. -A second pattern of disease with MAI has recently been described in middle-aged and elderly women, with small peribronchial nodules and bronchiectasis seen in a middle lobe and lingular distribution (lady Windemere syndrome) -"hot tub lung" is a hypersensitivity pneumonitis caused by inhalation of MAC |
|
|
Describe imaging findings of viral pneumonia:
|
-The diagnosis of viral pneumonia is often one of exclusion.
-Chest radiographic features are nonspecific and usually demonstrate a pattern of bronchopneumonia or interstitial opacities. -Resolution is usually complete, but permanent sequelae may be seen, including bronchiectasis, bronchiolitis obliterans (which may produce a unilateral hyperlucent lung or Swyer-James syndrome), and interstitial fibrosis. |
|
|
What is Swyer-James syndrome?
|
B-roncholitis obliterans, a complication of viral pneumonia
-Causes a small hyperlucent lung |
|
|
Describe imaging findings of influenza:
Which patients are most at risk? |
-In most patients the disease is confined to the upper respiratory tract, but in elderly persons, those with underlying cardiopulmonary disease or immunocompromise, and pregnant women, a severe hemorrhagic pneumonia may develop.
-In adults with influenzal pneumonia, there is often bilateral lower lobe patchy airspace opacification. -In children, a diffuse interstitial reticulonodular pattern is more commonly seen. -Bacterial superinfection with Streptococcus or Staphylococcus organisms contributes to a fulminating course that may result in death. -The development of lobar consolidation, pleural effusion, or cavitation suggests bacterial superinfection. |
|
|
What imaging findings suggest bacterial superinfection in an influenza patient?
|
The development of lobar consolidation, pleural effusion, or cavitation suggests bacterial superinfection.
|
|
|
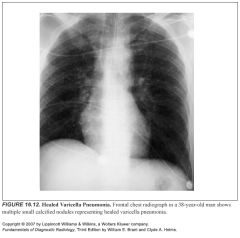
Describe imaging features of varicella pneumonia:
Which patients are most at risk? |
-Varicella-zoster, which causes chickenpox and shingles, may produce a severe pneumonia in adults.
-Patients on immunosuppressive therapy or with lymphoma are at greatest risk. -Chest radiographs characteristically show diffuse bilateral ill-defined nodular opacities 5 to 10 mm in diameter. -These opacities usually resolve completely, although in some patients they involute and calcify to produce innumerable small (2 to 3 mm) calcified nodules |
|
|
What is acute chest syndrome?
|
-It is defined as new consolidation on chest x-ray plus respiratory symptoms in a sickle cell patient
-The causes of the ACS are multiple; thus, the terminology "ACS" does not indicate a definite diagnosis but reflects the clinical difficulty of defining a distinct etiology in the majority of such episodes Possible causes: -Pulmonary infarction -Hypoventilation secondary to rib/sternal bone infarction -Hypoventilation secondary to narcotic administration -Pulmonary edema induced by narcotics or fluid overload -Infections (pneumococcal, mycoplasma, viruses) -Sarcoid -Asthma |
|
|
Describe imaging features of pulmonary histoplasmosis:
|
-The overwhelming majority (95% to 99%) of infections by H capsulatum are asymptomatic.
-A routine chest film demonstrating multiple well-defined calcified nodules less than 1 cm in size, with or without calcified hilar or mediastinal lymph nodes, may be the only indication of prior infection. -Acute histoplasma infection most often presents with the abrupt onset of flulike symptoms. -The chest radiograph in such patients may be normal or may show nonspecific changes, including subsegmental airspace opacities with or without associated hilar lymph enlargement. -If the patient inhales a large inoculum of organisms, widespread, fairly discrete nodular opacities 3 to 4 mm in diameter are seen with hilar adenopathy. -Alternatively, acute histoplasmosis may result in a solitary, sharply defined nodular opacity, <3 cm in diameter, termed a histoplasmoma. -Histoplasmomas are most common in the lower lobes and frequently calcify. -H capsulatum can also cause chronic pulmonary disease, usually in patients with underlying emphysema. -Unilateral or bilateral upper lobe cicatrizing atelectasis with marked hilar retraction may mimic the radiographic findings seen in postprimary TB. -Similarly, chronic upper lobe fibrocavitary disease may be seen. -Involvement of the mediastinum by chronic granulomatous inflammation may lead to fibrosing mediastinitis, while endobronchial disease can produce bronchostenosis. -Asymptomatic blood-borne dissemination of H capsulatum is common, as judged by the frequency of calcified splenic granulomas in residents of endemic areas. -The chest film most commonly shows widespread 2- to 3-mm nodules that are indistinguishable from those of miliary TB, though reticular opacities and patchy areas of consolidations may also be seen. |
|
|
What are the four different types of pulmonary coccidiodal infection:
|
There are four types of clinical and radiographic coccidioidal pulmonary infection: acute, persistent, chronic progressive, and disseminated coccidioidomycosis.
|
|
|
Describe imaging findings in acute coccidiodomycosis:
|
-These patients develop a self-limiting viral-type illness, which is referred to as “valley fever” when associated with erythema nodosum and arthralgias.
-The chest radiograph may be normal or show focal or multifocal segmental airspace opacities that resolve over several months. -Hilar and mediastinal adenopathy and pleural effusions may be seen in association with parenchymal disease |
|
|
Define persistent coccidiodomycosis:
What does it look like on imaging? |
-Patients whose symptoms or radiographic abnormalities persist beyond 6 to 8 weeks are considered to have persistent coccidioidomycosis.
-The radiographic features of persistent pulmonary disease include coccidioidal nodules or masses (coccidioidomas), persistent areas of consolidation, and miliary nodules. -Coccidioidal nodules are areas of round pneumonia, usually located in the subpleural regions of the upper lobes. -These nodules tend to cavitate rapidly and produce characteristic thin-walled cavities. |
|
|
Describe imaging findings in chronic progressive coccidiodomycosis:
|
In chronic progressive disease, upper lobe fibrocavitary disease similar to postprimary TB and histoplasmosis is seen.
|
|
|
List the different forms of pulmonary aspergillosis:
List the immune status of the host associated with each of the different forms: |
-Allergic (Allergic bronchopulmonary aspergillosis)--hypersensitive host
-Aspergilloma--normal immune status -Invasive--severely immunocompromised host -Semi-invasive (chronic necrotizing)--normal or mildly impaired host |
|
|
Describe imaging findings of an aspergilloma:
|
-An aspergilloma (mycetoma, fungus ball) is a ball of hyphae, mucus, and cellular debris that colonizes a preexisting bulla or a parenchymal cavity created by some other pathogen or destructive process.
-Invasion into adjacent lung parenchyma does not occur unless host defense mechanisms are compromised. -The mycetoma is usually asymptomatic, but may cause hemoptysis, which may be massive -An aspergilloma is seen as a solid round mass within an upper lobe cavity, with an “air crescent” separating the mycetoma from the cavity wall (Monod sign)--please note that technically, the air-crescent sign is used in necrotizing cavitary lesions like invasive aspergillosis -The mycetoma is usually free within the cavity and can be seen to roll dependently on decubitus radiographs or CT. -Progressive apical pleural thickening adjacent to a cavity is a common radiographic finding and should prompt a search for a complicating mycetoma. |
|
|
Describe imaging findings in invasive aspergillosis:
|
-Seen in severely immunocompromised patients (bone marrow transplant, leukemia)
-The infection starts with endobronchial fungal proliferation and then leads to vascular invasion with thrombosis and infarction -multiple pulmonary nodules -nodules have a characteristic halo of ground-glass (pulmonary hemorrhage) -within 2 weeks, nodules undergo cavitation resulting in the air-crescent sign -peribronchial opacities and focal areas of consolidation are also seen -If pleural effusion develops, it usually indicates empyema. |
|
|
What entities display the air-crescent sign?
|
-Invasive aspergillosis (after cavitation)
-actinomycosis -mucomycosis -septic emboli -tumors |
|
|
Describe imaging features of semi-invasive aspergillosis:
|
-occurs in mildly immunocompromised patients (diabetes, alcoholics, malnutrition, COPD)
-similar pathophysiology to invasive aspergillosis (vascular invasion with thrombosis and infarction) but progresses more slowly over months -appearance is similar to invasive aspergillosis (multiple pulmonary nodules with surrounding groundglass that cavitate) but cavitation occurs 6 mos or more after infection |
|
|
What's the difference between the monod sign and the air-crescent sign?
|
-Monod sign is seen in an aspergilloma and refers to the air between the fungus ball and the cavity it's housed in
-Air-crescent sign refers to a crescent shaped air collection in an actively cavitating lesion -Air-crescent sign is seen in invasive/semi-invasive aspergillosis, TB, mucormycosis, actinomycosis, septic emboli, tumors |
|
|
Describe pulmonary findings seen in amebiasis:
|
-Symptomatic infection with Entamoeba histolytica is usually confined to the GI tract and liver.
-If the infection remains confined to the subphrenic space, a right pleural effusion and basilar atelectasis may result from local diaphragmatic inflammation. -The most common method of pleuropulmonary involvement by amebiasis is by the direct intrathoracic extension of infection from a hepatic abscess. -This transdiaphragmatic spread of organisms may extend into the right pleural space to produce an empyema or may involve the right lower lobe to produce an amebic pneumonia or lung abscess. |
|
|
What organism causes hydatid disease?
What organism causes amebiasis? |
-Echinococcus granulosus is the cause of most cases of human hydatid disease.
-Entamoeba histolytica |
|
|
What are imaging features of pulmonary hydatid disease?
|
-Pulmonary echinococcal cysts characteristically present as well-circumscribed, spherical soft tissue masses.
-In distinction to hepatic cysts, lung cysts do not have calcified walls. -The cysts range in size from 1 to 20 cm, with a predilection for the lower lobes and the right side. -While most cysts remain asymptomatic, patients may present when the cyst develops a communication with the bronchial tree. -If the pericyst ruptures, a thin crescent of air will be seen around the periphery of the cyst, producing the “meniscus” or “crescent” sign. -If the cyst itself ruptures, the contents of the cyst are expelled into the airways, producing an air–fluid level. -On occasion, the cyst wall may be seen crumpled and floating within an uncollapsed pericyst, producing the pathognomonic “water lily” sign. -Rarely, a cyst will rupture into the pleural space, producing a large pleural effusion. |
|
|
What is the "water lilly" sign?
|
-From rupture of an echinococcal cyst within an intact pericyst
-The crumpled cyst wall looks like a water lilly |
|
|
Describe imaging features of pulmonary shistosomiasis:
|
-The larvae penetrate the skin or oropharyngeal mucosa and travel via the venous circulation to the pulmonary capillaries.
-As the larvae pass through the lungs, an allergic response may develop, presenting radiographically as transient airspace opacities (eosinophilic pneumonia) that resolve spontaneously -The mature flukes produce ova, which may embolize to the lungs, where they implant in and around small pulmonary arterioles. -The organism induces granulomatous inflammation and fibrosis, which leads to an obliterative arteriolitis, resulting in pulmonary hypertension and cor pulmonale. -Radiographically, a diffuse fine reticular pattern is most commonly seen in association with dilatation of the central pulmonary arteries. -Small nodular opacities resembling miliary TB may be seen as granulomata forming around ova. |
|
|
When does pneumonia become an AIDS defining infection?
|
The occurrence of two or more episodes of bacterial pneumonia within 1 year is categorized as an AIDS-defining illness for patients with HIV infection.
|
|
|
Which patients tend to get pulmonary nocardiosis?
|
It is usually an opportunistic infection in patients on immunosuppressive therapy, those with lymphoma or leukemia, and patients with alveolar proteinosis.
-nocardiosis is particularly common in patients with alveolar proteinosis |
|
|
Describe imaging features of pulmonary nocardiosis:
|
-The most frequent radiographic presentation is a homogeneous, nonsegmental airspace opacity or a mass.
-Cavitation is frequent -Infection may extend into the pleural space and chest wall to produce empyema and osteomyelitis, respectively. -Hilar lymph nodes may be enlarged. |
|
|
What do tuberculosis infections look like on imaging in HIV patients?
|
-The chest radiographic findings depend on the stage of HIV infection and the degree of immune dysfunction, which can be estimated by the CD4 count.
-In the early stages of AIDS (CD4 >200 cells/mm3), a postprimary pattern of upper lobe fibrocavitary disease indistinguishable from that seen in the immunocompetent patient is most common. -Later in the course of AIDS (CD4 50 to 200 cells/mm3), the radiographic features most often associated with primary disease are seen and include lobar consolidation, mediastinal and hilar lymphadenopathy, and pleural effusion -Rim-enhancing nodes with central necrosis on CT scans are a characteristic finding and should strongly suggest TB in a patient with AIDS. -In advanced AIDS (CD4 <50 cells/mm3), the radiographic findings are atypical and are characterized by diffuse reticular or nodular (miliary) opacities. |
|
|
Which patients tend to get CMV pneumonia?
What does it look like on imaging? |
-Cytomegalovirus is a common cause of viral pneumonia in patients with impaired cell-mediated immunity, specifically renal transplant recipients and lymphoma.
-It is an UNcommon cause of pneumonia in the AIDS population. -Chest radiographs show diffuse bilateral reticular or nodular opacities in the lower lobes. |
|
|
Describe typical imaging characteristics of PCP pneumonia in immunocompromised patients:
|
-A normal chest x-ray does not exclude PCP pneumonia (gallium scanning or HRCT of the lung may provide evidence of subradiographic disease)
-As the disease progresses, a fine reticular or ground-glass pattern develops, particularly in the parahilar regions -Progressive disease leads to confluent symmetric airspace opacification. -Pleural effusion or lymph node enlargement is distinctly uncommon (<5%) and should suggest an alternative or additional diagnosis. -Upper lobe predominance -Thin-walled cysts or pneumatoceles may develop during the course of disease and are responsible for an increased incidence of spontaneous pneumothorax, complicating PCP |
|
|
Which nucs test can be used for PCP pneumonia?
|
-Gallium scans
-Gallium is taken up in a wide variety of active inflammatory processes |
|
|
Describe imaging features of pulmonary toxoplasmosis:
Which patients are affected? |
-Pulmonary involvement is usually seen in the generalized form of the disease, which affects immunocompromised hosts, including those with AIDS, organ transplant recipients, and patients with leukemia or lymphoma.
-The radiographic findings in pulmonary toxoplasmosis include diffuse reticular opacities that resemble those of acute viral pneumonia. -Less commonly, airspace opacities with air bronchograms may be seen. -Hilar and mediastinal lymph node enlargement is common, while pleural effusion is rare. -With generalized disease, most often seen in patients with AIDS, diffuse bilateral small nodular opacities may be seen |
|
|
Describe the common pulmonary complications of bone marrow transplant and how they vary based on time:
|
Because of the predictable course of immune suppression, a timeline of expected pulmonary complications can be constructed to help narrow the differential diagnosis for radiographic abnormalities in patients following BMT:
Neutropenic phase (0–30 days) -Pulmonary edema -Alveolar hemorrhage -Fungal infection -Drug reaction Early phase (30–100 days) -Fungal infection -Drug reaction -Cytomegalovirus infection -Upper respiratory virus infection -Idiopathic pneumonia -Acute graft-versus-host disease Late phase (>100 days) -Bronchiolitis obliterans -Bronchiolitis obliterans–organizing pneumonia -Chronic graft-versus-host disease -Upper respiratory virus (to 6 months) -Idiopathic pneumonia (to 6 months) |

