![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
195 Cards in this Set
- Front
- Back
|
What is the normal volume of fluid in the pleural space?
|
2-5 ml
|
|
|
How does pleural fluid form?
|
-According to Starling’s law
-Depends upon hydrostatic and oncotic forces in both the systemic capillaries of the parietal pleura and the pleural space -Pleural fluid is formed by filtration from systemic capillaries in the parietal pleura and resorbed via the parietal pleural lymphatics |
|
|
What is the criteria for a transudative pleural effusion (Light’s criteria)?
|
-Pleural/serum protein ratio <0.5
-Pleural/serum LDH ratio <0.6 -Pleural LDH <200 IU/L |
|
|
What conditions cause an elevation in the hydrostatic pressure?
|
-Left heart failure (most common)
-Fluid overload from renal failure -Pregnancy -Constrictive pericarditis |
|
|
What conditions cause a decrease in oncotic pressure?
|
-Hypoproteinemia of liver failure (most common)
-Nephrotic syndrome -Severe malnutrition -Protein losing enteropathy |
|
|
Why do exudative pleural fluids form (physiology)?
|
Increased pleural capillary permeability
|
|
|
What conditions cause exudative pleural effusions?
|
Peripheral pulmonary or pleural processes that inflame the pleura (pneumonia, serositis)
Processes that directly invade the pleura (malignancy) |
|
|
Characterize the pleural effusion associated with CHF:
|
-Transudative
-Usually bilateral -Usually larger on the right side -An isolated right effusion is twice as common as an isolated left effusion |
|
|
Why does pneumonia cause a pleural effusion?
|
-Called parapneumonic effusion and empyema
-Peripheral infections cause visceral pleural inflammation that increases pleural capillary permeability -Inflammatory thickening of the pleural membranes with lymphatic obstruction may also occur |
|
|
Define empyema:
|
When parenchymal infection extends into the pleural space
|
|
|
Which infections tend to produce empyema?
|
-Bacterial pneumonia
-Septic emboli -Lung abscess -Fungal, viral and parasitic infections do not commonly cause empyema -Less commonly, infection may extend into the pleural space from the spine, mediastinum, and chest wall |
|
|
What percent of pneumonias have a pleural effusion?
|
40%
|
|
|
Which organisms are the most common causes of parapneumonic effusion and empyema?
|
Staph aureus
Gram-negatives |
|
|
Describe the first stage of parapneumonic effusion formation:
|
-Exudative phase
-Visceral pleural inflammation causes increased capillary permeability and pleural fluid accumulation -Most of these sterile exudative effusions resolve with appropriate antibiotic therapy |
|
|
Describe the second stage of parapneumonic effusion formation:
|
-Fibrinopurulent pleural fluid collection containing bacteria and neutrophils
-Fibrin deposition on the visceral and parietal pleura impairs fluid resorption and produces loculations |
|
|
Describe the third stage of parapneumonic effusion formation:
|
-2-3 weeks after initial pleural fluid formation
-Characterized by the ingrowth of fibroblasts over the pleura, which produces pleural fibrosis and entraps the lung -Dystrophic calcification of the pleura may develop following resolution of the pleural infection. |
|
|
Describe TB related effusions:
|
-Caused by the rupture of subpleural caseating granulomas
-May be a complication of primary infection, or the presenting feature -More common in young adults with pulmonary disease and HIV pts with severe immunodeficiency -Typically straw colored, with >70% lymphocytes and low glucose |
|
|
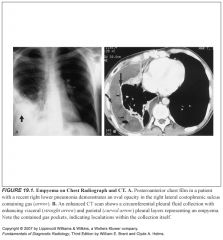
What does empyema look like on plain film and CT?
|
-Loculated pleural fluid collection
-On CT, it is elliptic in shape -Seen most often within the posterior and inferior pleural space -The collection conforms to and maintains a broad area of contact with the chest wall |
|
|
Why is it so important to tell the difference between a empyema from peripheral lung abscess?
|
Because you treat them differently—empyemas have to be drained externally. Lung abscesses respond to postural drainage and antibiotics
|
|
|
How can you tell an empyema from a peripheral lung abscess?
|
-Contrasted CT is most useful
-Most findings are not specific for empyema -"split pleura sign" with enhancement of the visceral and parietal pleural layers. -Pleural thickening can be seen in noninfected collection but thicker pleura is more suggestive of empyema -Thickening of the extrapleural fat |
|
|
How can you tell if there’s an empyema if there is extensive parenchymal consolidation?
|
-Thickening and enhancement of the parietal pleura
-Presence of loculations -Detection of discrete soft tissue lesions along the parietal pleura outlined by low attenuation pleural fluid |
|
|
What do hemorrhagic pleural effusions look like on CT?
|
-High attenuation
-Presence of fluid-fluid level caused by dependent cellular blood elements |
|
|
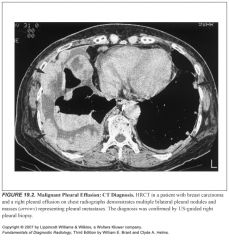
Which tumors are most commonly associated with pleural effusions?
(in order of frequency) |
-Lung ca
-Breast ca -Pelvic tumors -Gastric ca -Lymphoma |
|
|
Describe findings of hemothorax:
|
-Intrapleural blood coagulates quickly, forming septations
-Acute hemothorax will have high attenuation on CT (>80 H) -Associated rib fractures or subcutaneous emphysema should suggest this diagnosis |
|
|
Which side is the pleural effusion from Boerhaave syndrome normally in?
|
Left side
|
|
|
What is the incidence of pleural effusions in SLE?
|
Ranges from 33-74%
|
|
|
Characterize the pleural effusion associated with SLE:
|
-Exudative, from pleural inflammation
-In some cases, the nephrotic syndrome associated with SLE may produce a transudative effusion -Cardiomegaly is a common finding and may be caused by pericardial effusion, hypertension, renal failure, or lupus associated endocarditis |
|
|
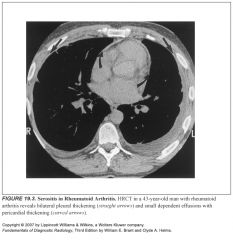
Describe the pleural effusion associated with RA:
|
-Frequently seen in males
-Form independent of pulmonary parenchymal involvement -May develop after rupture of peripheral rheumatoid nodules -Exudative, low glucose, low pH (<7.2), lymphocytosis |
|
|
Describe postpericardiotomy syndrome:
|
-Automimmune syndrome producing pleural and pericardial effusions
-Fever, pleuritis, pneumonitis, pericarditis -Develops within days to weeks of the precipitating event -X-ray findings: enlargement of the cardiac silhouette, pleural effusions, parenchymal airspace opacities -Serosanguinous effusion is seen in over 80% -Treated with NSAIDS |
|
|
Describe Dressler syndrome:
|
-Following an MI
-Automimmune syndrome producing pleural and pericardial effusions -Fever, pleuritis, pneumonitis, pericarditis -Develops within days to weeks of the precipitating event -X-ray findings: enlargement of the cardiac silhouette, pleural effusions, parenchymal airspace opacities -Serosanguinous effusion is seen in over 80% -Treated with NSAIDS |
|
|
How could peritoneal fluid enter the pleural space?
|
-Radioisotope studies demonstrate that peritoneal fluid may enter the pleural space via transdiaphragmatic lymphatic channels or through defects in the diaphragm
-The lymphatic channels are larger on the right, accounting for the higher incidence of right-sided effusions associated with ascites or liver failure (hepatic hydrothorax) |
|
|
Describe the pleural effusion associated with pancreatitis:
|
Occurs with acute or chronic
-Most often left-sided because of the proximity of the pancreatic tail to the left hemidiaphragm -Typically exudative, may be bloody -Rupture of the pancreatic duct can lead to a pancreaticopleural fistula |
|
|
Describe subphrenic abscess associated pleural effusion:
|
-Complication of abdominal surgery or perforation of a hollow viscus
-Can cause diaphragmatic paresis, basilar atelectasis, pleural effusion -Diagnosed on CT or US |
|
|
What is Meigs syndrome?
|
-Pleural effusion associated with ovarian fibroma
-Usually transudative, resolve following tumor removal -A number of pelvic and abdominal tumors (including pancreatic and ovarian malignancy, lymphoma, and uterine leiomyomas) can also cause pleural effusion |
|
|
Where does the thoracic duct empty?
|
The confluence of the left internal jugular and subclavian veins
|
|
|
What side is the thoracic duct on?
|
-The lower part is on the right side
-The higher part is on the left side -It crosses at the level of the sixth thoracic vertebra |
|
|
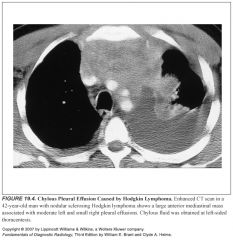
What are causes of chylothorax?
|
Malignancy, iatrogenic trauma, TB
|
|
|
What does a chylothorax look like on x-ray/CT?
|
Like any other free-flowing effusion
|
|
|
How does one make a diagnosis of chylothorax?
|
Triglycerides >110 mg/dL
|
|
|
Describe pleural effusion associated with PE:
|
-Associated with elevation of the ipsilateral diaphragm and peripheral wedge-shaped opacities (Hampton’s hump)
-Typically small, unilateral, serosanguinous |
|
|
What drugs are associated with pleural effusion?
|
-Methysergide causes pleural inflammation
-Phenytoin, isoniazid, hydralazine, procainamide produce a lupus-like syndrome -Nitrofurantoin is associated with immunologic reaction that causes eosinophilic pleuropulmonary disease |
|
|
How do you treat transudative pleural effusions?
|
Treat the underlying disorder because the pleura are essentially normal
|
|
|
How do you treat parapneumonic effusions?
|
-Depends on how likely the effusion will cause pleural fibrosis and respiratory impairment
-Larger, loculated collections with positive gram stains or cultures and pH<7.2 are associated with moderate to high risk for poor outcome. These should be drained if possible -Options for drainage include image-guided, intrapleural fibrinolytics, open pleural drainage with VATS, or thoracotomy with decortication |
|
|
How do you treat malignant pleural effusions?
|
-Closed drainage and pleural sclerosis with talc
-Some pts get VATS drainage -Some pts receive indwelling silastic catheters and pts drain their own fluid |
|
|
How do you treat chylothorax?
|
Treat underlying etiology
|
|
|
What is a bronchopleural fistula?
|
-Communication between the lung and the pleural space
-Often originates from a peripheral airway -If it originates peripherally, it can cause intractable pneumothorax -If it originates proximally, it can cause empyema |
|
|
What causes bronchopleural fistulas?
|
-Dehiscence of a bronchial stump following lobectomy or pneumonectomy
-Necrotizing pulmonary infection |
|
|
How does bronchopleural fistula present on x-ray?
|
-Loculated intrapleural air and fluid collection
-CT is useful in distinguishing bp fistula from empyema and may demonstrate the actual fistulous communication |
|
|
What does the chest look like after a pneumonectomy?
|
-The residual space gradually fills with fluid and appears as an opaque hemithorax with ipsilateral mediastinal shift
-Development of an air-fluid level or a drop in the air-fluid level associated with mediastinal shift back toward the mid-line suggests bronchopleural fistula |
|
|
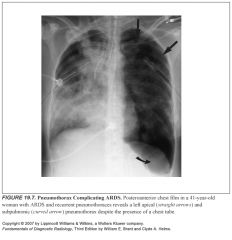
What are the two types of pneumothorax?
|
Spontaneous and traumatic
|
|
|
Two types of spontaneous pneumothorax?
|
Primary—no identifiable etiology
Secondary—associated with underlying pathology |
|
|
Usual presenting sx’s of a pneumothorax?
|
Dyspnea and chest pain
|
|
|
What is the most common cause of pneumothorax?
|
Trauma
|
|
|
How can blunt chest trauma cause pneumothorax?
|
-An acute increase in intrathoracic pressure results in extra-alveolar interstitial air because of alveolar disruption which tracks peripherally and ruptures into the pleural space
-Laceration of tracheobronchial tree can cause a bronchopleural fistula -Rib fractures can project inward to lacerate the lung |
|
|
Who gets spontaneous pneumos?
|
Young or middle-aged, usually tall men
|
|
|
Why do spontaneous pneumothoraces occur?
|
Pts have blebs or bullae within the lung apices that spontaneously rupture
|
|
|
How do you treat spontaneous pneumothorax?
|
Initial episode gets closed tube drainage
Recurrent or persistent leaks get a thorascopic bullectomy |
|
|
What is the medical condition most assoc with pneumothorax?
|
COPD
|
|
|
How can cancer cause pneumothorax?
|
Pneumothorax develops when necrotic subpleural metastases rupture into the pleural space
|
|
|
What are the most common malignancies that can cause pneumothorax?
|
Osteogenic sarcoma, lymphoma, and germ cell malignancies
|
|
|
What is the most common connective tissue disorder to cause pneumothorax?
|
Marfan’s—usually from rupture of an apical bulla
|
|
|
Causes of traumatic pneumothorax:
|
Iatrogenic
-Thoracic/abdominal surgery -Percutaneous interventional procedures (Lung/pleural biopsy, Thoracentesis) -Central line placement -Mechanical ventilation -Esophagoscopic biopsy/dilatation -Bronchoscopic biopsy Non-iatrogenic -Penetrating injury (Stab or gunshot wound) -Blunt injury (Tracheobronchial disruption, Esophageal rupture) |
|
|
Causes of secondary spontaneous pneumothorax:
|
Obstructive airways disease
-Asthma -Emphysema Infection -Cavitating pneumonia -Lung abscess -Septic emboli -Pneumotoceles Pulmonary infarction (rare) Neoplasm -Bronchogenic carcinoma -Pleural or chest wall neoplasm Cystic lung disease -Sarcoidosis -Eosinophilic granuloma -Cystic fibrosis -Tuberous sclerosis -Lymphangioleiomyomatosis Catamenial pneumothorax Connective tissue disorders -Marfan syndrome -Ehlers-Danlos syndrome -Cutis laxa |
|
|
Why would someone with ARDS be at increased risk of pneumothorax?
|
-Positive pressure ventilation
-Underlying COPD -Underlying pneumonia -Frequent line placements and other invasive procedures -ARDS pts develop small peripheral cystic airspaces, which can rupture into the pleural space. |
|
|
Define catamenial pneumothorax:
|
-Rare, recurrent pneumothorax that occurs with menstruation
-Caused by cyclical necrosis of pleural endometrial implants -Also, air may enter the peritoneal cavity during menstruation and gain access to the pleural cavity via diaphragmatic defects (Catamenial pneumothoraces tend to be on the right side because of this) -Usually women in their fourth decade -Pneumothoraces tend to be small and resolve spontaneously |
|
|
Prevention of catamenial pneumothorax?
|
Preventing menstruation with OCPs
|
|
|
What’s the most common cause of a tension pneumothorax?
|
Iatrogenic trauma in a mechanically ventilated pt
|
|
|
What’s the tension in a tension pneumothorax?
|
-The check-valve lets air in but not out
-This causes the formation of a pleural air collection that has a pressure exceeding atmospheric pressure |
|
|
Why are tension pneumothoraces deadly?
|
-The pressure causes complete collapse of the underlying lung
-More importantly, the pressure impairs venous return to the heart |
|
|
Presenting signs of pneumothorax?
|
Tachypnea, tachycardia, cyanosis, hypotension
|
|
|
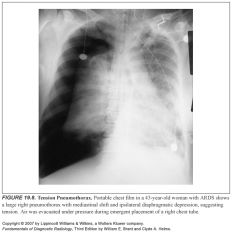
X-ray findings in tension pneumothorax?
|
-Involved hemithorax is expanded and hyperlucent
-Medially retracted lung -Ipsilateral diaphragmatic depression or inversion -Contralateral mediastinal shift |
|
|
Important thing to remember about mediastinal shift in pneumothoraces:
|
It does not mean that there’s a tension pneumo (it is a clinical diagnosis). Immediate evacuation of the pleural space should be performed with a needle, catheter, or large-bore thoracostomy tube.
|
|
|
What is the most common cause of localized pleural thickening?
|
pneumonia
|
|
|
Give a differential for localized pleural thickening:
|
Localized pleural thickening from fibrosis is usually the end result of peripheral parenchymal and pleural inflammatory disease, with pneumonia the most common cause. Additional causes include pulmonary embolism with infarction, asbestos exposure, trauma, prior chemical pleurodesis, and drug-related pleural disease.
|
|
|
Which pleura is more likely the calcify, the visceral or parietal?
|
It more often the visceral pleura that calcifies.
|
|
|
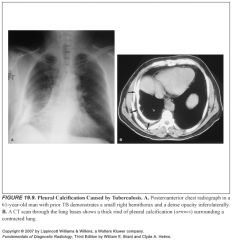
Give a differential for pleural calcifications:
|
It is usually the result of prior hemothorax or empyema (e.g., TB), although pleural thickening from any cause may calcify. Asbestos exposure can cause bilateral calcified parietal pleural plaques. Visceral pleural calcifications from pleural hemorrhage or infection are indistinguishable radiographically.
|
|
|
What should you think of if you see a fluid layer within calcified pleural layers?
|
The presence of fluid within calcified pleural layers seen on CT suggests an active empyema and is most often seen in patients with prior TB.
|
|
|
Which opacities can mimic focal pleural thickening?
|
-Apical cap
-Companion shadows of first and second ribs -Subpleural deposits of fat |
|
|
Give a differential for a pleural/extrapleural mass:
|
Neoplasm:
Benign: -Fibroma -Lipoma -Neurofibroma Malignant: -Metastases (usually multiple) -Mesothelioma (usually diffuse pleural thickening) Loculated pleural effusion/empyema Hematoma |
|
|
What can mimic a pleural mass on radiographs?
|
loculated pleural fluid can mimic a pleural mass radiographically.
|
|
|
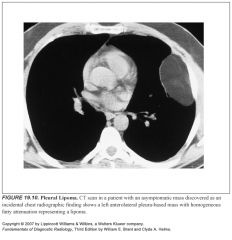
What is diagnostic of a pleural lipoma?
|
Homogeneous fat attenuation on CT scan (-30 to -100 H) is diagnostic
|
|
|
Are localized fibrous tumors of pleura (LFTP) benign or malignant?
|
80% are benign, 15% will recur after resection.
|
|
|
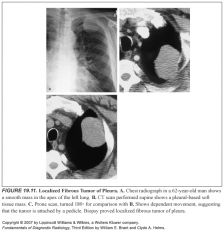
What does a localized fibrous tumor of pleural (LFTP) look like on imaging?
|
These lesions appear as well-defined, spherical or oblong masses. These tumors are occasionally attached to the pleura by a narrow pedicle, a finding that is virtually pathognomonic and accounts for changes in intrapleural location seen with changes in patient positioning in some individuals. CT usually shows a smoothly marginated, pleura-based soft tissue mass with either uniform soft tissue attenuation or inhomogeneous enhancement caused by areas of necrosis.
|
|
|
What are localized fibrous tumors of pleural associated with?
|
An association between LFTP and hypertrophic pulmonary osteoarthropathy and hypoglycemia is recognized.
|
|
|
Are localized fibrous tumors of pleural associated with asbestos exposure?
|
No.
|
|
|
What kinds of things cause diffuse, smooth pleural thickening?
|
-Pleural fibrosis
-Hemothorax -Prior empyema or exudative effusion (including asbestos exposure) -Interstitial pulmonary fibrosis -Pleural effusion (particularly on supine radiographs) |
|
|
What kinds of things cause diffuse lobulated pleural thickening?
|
Primary
-Mesothelioma Metastatic -Adenocarcinoma of lung, breast, ovary, kidney, GI tract -Invasive thymoma -Lymphoma (subpleural deposits) Multiloculated pleural effusion/empyema |
|
|
Define fibrothorax:
|
Fibrothorax (diffuse pleural fibrosis) is defined as pleural thickening extending over more than one fourth of the costal pleural surface. The fibrothorax can encompass the entire lung and produce entrapment. When this causes a restrictive ventilatory defect, pleurectomy (decortication) may be necessary to restore function to the underlying lung.
|
|
|
What kinds of things cause fibrothorax?
|
Fibrothorax most commonly results from the resolution of an exudative pleural effusion (including asbestos-related effusions), empyema, or hemothorax. It may also be seen as a subpleural extension of diffuse interstitial fibrosis.
|
|
|
What cancers tend to metastasize to the pleura?
|
The malignant tumors with a propensity to metastasize to the pleura include adenocarcinomas of the lung, breast, ovary, kidney, and GI tract.
|
|
|
What cancers can be locally invasive to the pleura?
|
Invasive thymoma or thymic carcinoma, mesothelioma, and rarely non-Hodgkin lymphoma.
|
|
|
What does malignant (versus benign) pleural disease look like on imaging?
|
Pleural malignancy presents radiographically as multiple discrete pleural masses or lobulated pleural thickening.
The pleural lesions are often obscured by an associated malignant pleural effusion. Contrast-enhanced CT can distinguish solid pleural masses from loculated pleural fluid and can show discrete pleural masses or thickening in patients with large effusions. In contrast to benign pleural thickening, malignant pleural disease is more likely when the pleural thickening on CT is circumferential and nodular, greater than 1 cm in thickness, and/or involves the mediastinal pleura. Chest wall invasion by pleural tumor, seen as rib destruction or soft tissue infiltration of the subcutaneous fat and musculature, is better appreciated on CT or MR than on plain films. |
|
|
1
|
|
|
2
|
|
|
4
|
|

|
5
|
|

|
6
|
|
|
7
|
|
|
8
|
|
|
9
|
|
|
10
|
|
|
11
|
|

|
12
|
|
|
13
|
|
|
14
|
|

|
15
|
|
|
16
|
|
|
3
|
|

|
17
|
|

|
18
|
|
|
19
|
|
|
20
|
|
|
21
|
|

|
22
|
|
|
23
|
|
|
24
|
|
|
25
|
|
|
26
|
|

|
27
|
|
|
28
|
|

|
29
|
|
|
30
|
|
|
31
|
|

|
32
|
|
|
33
|
|
|
34
|
|
|
35
|
|

|
36
|
|
|
37
|
|
|
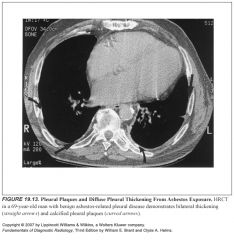
What is the most common manifestation of adbestos exposure?
|
-Benign pleural disease is the most common thoracic manifestation of asbestos inhalation and includes pleural plaques, pleural effusions, and diffuse pleural fibrosis.
-Pleural effusion is the first manifestation. -Specifically, pleural plaques are the most common benign manifestation of asbestos inhalation. |
|
|
Where are pleural plaques related to asbestos exposure located?
|
-Asbestos plaques are found on the parietal pleura, most commonly over the diaphragm and lower posterolateral chest wall.
-The mediastinal pleural surface and costophrenic sulci are characteristically spared. -Visceral pleural plaques, in contrast, are seen as discrete flat regions of pleural thickening within the major fissures on HRCT, are most commonly associated with interstitial fibrosis. |
|
|
What do pleural plaques related to asbestos exposure look like?
|
-The plaques are discrete, bilateral, slightly raised (2 to 10 mm thick) foci of pleural thickening.
-Histologically, the plaques are comprised of dense bands of collagen. -Punctate or linear calcification within the plaques is common and is more frequent as the plaques enlarge. |
|
|
Which entity causes plaques/calcifications of the parietal pleura? What about the visceral pleura?
|
-Asbestos exposure
-Pulmonary fibrosis |
|
|
What do calcified pleural plaques look like on plain film?
|
-Detection of pleural plaques on conventional radiographs is best performed with 45° oblique views that profile the anterolateral and posterolateral plaques.
-When viewed en face, the calcified plaques appear as geographic areas of opacity that have been likened to a holly leaf -Although plaques are invariably bilateral on gross examination of the pleural space in affected individuals, it is not unusual to see unilateral plaques (most often left-sided) on conventional radiographs or HRCT. |
|
|
How long after asbestos exposre do patients develop pleural effusions? What about pleural plaques? What about mesothelioma?
|
-Pleural effusion occurs 10 to 20 years after the initial exposure and is the earliest manifestation of asbestos-related pleural disease.
-The development of asbestos-related effusions appears to be dose related. -While most asbestos-related pleural effusions resolve spontaneously, up to one third recur and some patients develop diffuse pleural fibrosis. -Pleural plaques develop 20 to 30 years after the initial asbestos exposure and are more frequent with increasing length and severity of exposure. -Mesothelioma most often occurs 30 to 40 years after the initial exposure. -It is not dose dependent. |
|
|
What does diffuse pleural thickening from asbestos exposure look like? How does it differ from asbestos related pleural plaques?
|
-Diffuse asbestos pleural thickening is defined as smooth, flat pleural thickening extending over one fourth of the costal pleural surface.
-In distinction to pleural plaques, which affect the parietal pleura alone, diffuse pleural fibrosis involves both the parietal and visceral pleura. -Radiographically, diffuse pleural thickening is seen as a smooth thickening of the pleura involving the lower thorax with blunting of the costophrenic sulci. |
|
|
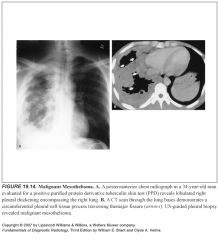
What does malignant mesothelioma look like?
|
-Mesothelioma typically grows by contiguous spread from the pleural space into the lung, chest wall, mediastinum, and diaphragm; distant metastases are not uncommon.
-It most often appears radiographically as thick (>1 cm) and lobulated diffuse pleural thickening. -Calcification or, rarely, ossification is seen in 20% of tumors, although calcified pleural plaques may be seen in uninvolved areas of the pleura. -A pleural effusion is often present, which, if large, may obscure the pleural tumor. -Malignant involvement of the mediastinal pleural surface may prevent contralateral mediastinal shift despite extensive pleural tumor volume and effusion, a finding that may help distinguish mesothelioma from metastatic disease. -Adenopathy is seen in the ipsilateral hilum and mediastinum in approximately 50% of patients. -While the radiologic findings may be highly suggestive of mesothelioma, metastatic pleural malignancy can have a similar appearance, so histologic confirmation is necessary. |
|
|
What do you always have to include in your differential if you're suggesting mesothelioma?
|
While the radiologic findings may be highly suggestive of mesothelioma, metastatic pleural malignancy can have a similar appearance, so histologic confirmation is necessary.
|
|
|
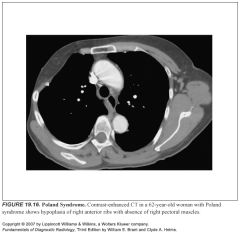
Describe Poland syndrome:
|
-Poland syndrome is an autosomal recessive disorder characterized by unilateral absence of the sternocostal head of the pectoralis major, ipsilateral syndactyly, and rib anomalies.
-There may be associated aplasia of the ipsilateral breast |
|
|
What's the syndrome where there's a missing pectoralis muscle on one side?
|
Poland syndrome
|
|
|
What do chest x-rays look like if a patient has had a mastectomy?
|
-Patients who have had a mastectomy will show unilateral hyperlucency.
-In those who have undergone a modified radical mastectomy, the horizontally oriented inferior edge of the hypertrophied pectoralis minor muscle may be identified on frontal radiographs. |
|
|
What is a dumbbell lipoma?
|
Lipomas may be intrathoracic or extrathoracic, or they may project partially within and outside the thorax (dumbbell lipoma).
|
|
|
What are the most common primary malignant tumors of the chest wall? Who's at increased risk? What do they look like?
|
-Fibrosarcomas and liposarcomas are the most common malignant soft tissue neoplasms of the chest wall in adults.
-Malignant tumors often present with symptoms of localized chest wall pain and a visible, palpable mass. -Patients who have received chest wall radiation are at particular risk for developing sarcomas. -Radiographically, these soft tissue masses are often associated with bony destruction. -CT best depicts the bone destruction and intrathoracic component of tumor, while MR shows the extent of tumor and delineates tumor from surrounding muscle and subcutaneous fat |
|
|
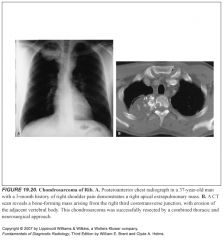
What is an Askin tumor?
|
-A rare malignant neoplasm arising from the chest wall of children and young adults is an Askin tumor, which arises from primitive neuroectodermal rests in the chest wall
-These lesions are very aggressive and associated with a high mortality rate. |
|
|
What is the aggressive chest wall tumor in kids that comes from neuroectodermal tissue?
|
Askin tumor
|
|
|
What are intrathoracic ribs?
What side do they normally arise from? |
Intrathoracic ribs are extremely rare congenital anomalies where an accessory rib arises from a vertebral body or the posterior surface of a rib and extends inferolaterally into the thorax, usually on the right side.
|
|
|
What are ribbon ribs?
What conditions are they associated with? |
Osteogenesis imperfecta and neurofibromatosis may be associated with thin, wavy, “ribbon” ribs.
|
|
|
What are cervical ribs?
What complications are associated with cervical ribs? |
-A relatively common congenital anomaly is the cervical rib, which arises from the seventh cervical vertebral body.
-Cervical ribs are usually asymptomatic, although in a minority of individuals with the thoracic outlet syndrome, the rib or associated fibrous bands can compress the subclavian artery, producing secondary ischemic symptoms, or compress the subclavian vein and brachial plexus, producing pain, weakness, and swelling of the upper extremity. -Surgical resection of the cervical rib can relieve the symptoms in selected patients. |
|
|
What is rib notching?
What is the most common cause of rib notching? Can you think of other causes of rib notching? |
-Inferior rib notching is much more common than superior rib notching and is caused by enlargement of one or more of the structures that lie in the subcostal grooves (intercostal nerve, artery, or vein).
-The notching predominantly affects the posterior aspects of the ribs bilaterally and may be narrow, wide, deep, or shallow. -The most common cause of bilateral inferior rib notching is coarctation of the aorta distal to the origin of the left subclavian artery. -Other causes of aortic obstruction that can lead to inferior rib notching include aortic thrombosis and Takayasu aortitis. -Congenital heart diseases associated with decreased pulmonary blood flow may be associated with rib notching as the intercostal arteries enlarge in an attempt to supply collateral blood flow to the oligemic lungs. -Superior vena cava obstruction can cause increased flow through intercostal veins and produce rib notching. -Multiple intercostal neurofibromas in neurofibromatosis type 1 are the most common nonvascular cause of inferior rib notching. |
|
|
When does rib notching develop in patients with aortic coarctation?
|
-Patients with aortic coarctation develop rib notching gradually; it is most common in adolescents and is rare in children under age 7.
|
|
|
Which ribs are notched with coarctation of the aorta (proximal to the origin of the left subclavian)?
|
-The notching predominantly affects the posterior aspects of the ribs bilaterally and may be narrow, wide, deep, or shallow.
-The first two ribs are uninvolved because the first and second intercostal arteries arise from the superior intercostal branch of the costocervical trunk of the subclavian artery and therefore do not communicate with the descending thoracic aorta. |
|
|
What conditions cause unilateral inferior rib notching?
|
-Coarctation may produce unilateral left rib notching when the aortic narrowing occurs proximal to an aberrant right subclavian artery.
-Unilateral right-sided notching occurs when the coarctation is proximal to the left subclavian artery. -Additional causes of unilateral inferior rib notching include subclavian artery obstruction and surgical anastomosis of the proximal subclavian artery to the ipsilateral pulmonary artery (Blalock-Taussig procedure) -Multiple intercostal neurofibromas in neurofibromatosis type 1 are the most common nonvascular cause of inferior rib notching and may be unilateral |
|
|
Describe bony thoracic manifestations of neurofibromatosis type 1:
|
-Multiple intercostal neurofibromas in neurofibromatosis type 1 are the most common nonvascular cause of inferior rib notching.
-The neurofibromas appear as multiple extrapleural soft tissue masses, most often seen in the upper paravertebral regions. -Other thoracic bony manifestations of neurofibromatosis include ribbon ribs, thoracic kyphoscoliosis, and scalloping of the posterior aspect of the vertebral bodies caused by dural ectasia. |
|
|
What sorts of things cause superior rib notching?
Why does it occur? |
-Superior rib notching is much less common than inferior rib notching.
-The pathogenesis of superior rib notching is unknown, although a disturbance of osteoblastic and osteoclastic activity and the stress effect of the intercostal muscles are proposed mechanisms. -Paralysis is the most common condition associated with superior rib notching. -Other etiologies include rheumatoid arthritis, systemic lupus erythematosus, and rarely, marked tortuosity of the intercostal arteries from severe, long-standing aortic obstruction. |
|
|
Why are fractures of the first three ribs significant?
|
Since the first three ribs are well protected by the clavicles, scapulae, and shoulder girdles, fracture of these ribs indicates severe trauma and should prompt a careful evaluation for associated great vessel and visceral injuries.
|
|
|
Define flail chest:
Why is it significant? |
-Severe blunt trauma to the ribcage, in which multiple contiguous ribs are fractured in more than one place, is termed a “flail chest.”
-This results in a free segment of the chest wall that moves paradoxically inward on inspiration and outward on expiration. |
|
|
When fibrous dysplasia affects the ribs, what does it look like on imaging?
|
-The ribs are the most common site of involvement by monostotic fibrous dysplasia.
-The typical appearance is an expansile lesion in the posterior aspect of the rib with a lucent or ground-glass density; rarely, the lesion is sclerotic. -Multiple rib involvement from polyostotic fibrous dysplasia can result in severe restrictive pulmonary disease. |
|
|
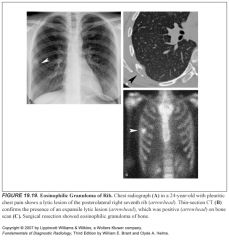
What do eosinophilic granulomas of the ribs look like on imaging?
How can you distinguish it from fibrous dysplasia? |
-Eosinophilic granuloma can cause lytic lesions in patients under age 30.
-These are usually solitary lytic lesions, which can be expansile but do not have sclerotic margins; this latter feature helps distinguish these lesions from fibrous dysplasia |
|
|
Which infections are notorious for transpleural spread to the chest wall?
|
Pleuropulmonary infections that may traverse the pleural space and produce a chest wall infection include TB, actinomycosis, and nocardiosis.
|
|
|
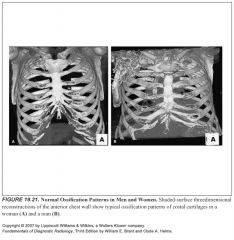
How can you tell the difference between male and female patients by their costal cartilage ossification?
|
-Female costal cartilage ossification involves the central portion of the cartilage, extending from the rib toward the sternum in the shape of a solitary finger, while male costal cartilage ossification involves the peripheral portion of the cartilage and has the appearance of two fingers (“peace” sign).
-These typical patterns of male and female costal cartilage ossification are seen in 70% of patients and do not apply to the first rib. |
|
|
What is a Sprengel deformity?
What is Klippel-Feil syndrome? |
-Sprengel deformity is a congenital anomaly in which the scapula is hypoplastic and elevated.
-The association of Sprengel deformity with an omovertebral bone, fused cervical vertebrae, hemivertebrae, kyphoscoliosis, and rib anomalies is termed the Klippel-Feil syndrome. |
|
|
What is the term for a congenitally hypoplastic and elevated scapula?
|
Sprengel deformity
(The association of Sprengel deformity with an omovertebral bone, fused cervical vertebrae, hemivertebrae, kyphoscoliosis, and rib anomalies is termed the Klippel-Feil syndrome) |
|
|
What causes a winged scapula?
|
-A winged scapula is identified when the scapula is superiorly displaced from its normal position and the inferior portion is posteriorly displaced from the chest wall, thereby foreshortening its appearance on the frontal radiograph.
-This deformity results from disruption in the innervation of the serratus anterior muscle that maintains the scapula against the chest wall. |
|
|
What is cleidocranial dysostosis?
|
-The clavicles are completely missing or reduced to small vestiges, this allows hypermobility of the shoulders including ability to touch the shoulders together in front of the chest.
-Failure of fontanelles to close |
|
|
What diseases are associated with erosion of the distal clavicles?
|
-Rheumatoid arthritis and hyperparathyroidism are associated with erosion of the distal clavicles.
-The distal clavicle is sharply defined in rheumatoid arthritis and tapers to a point, whereas in hyperparathyroidism it is often widened and irregular. |
|
|
What syndromes are usually associated with extramedullary hematopoiesis?
Why is extramedullary hematopoiesis often paraspinal in location? |
Chronic anemia in patients with thalassemia major or sickle cell disease may result in prevertebral or paravertebral masses of extramedullary hematopoiesis, which represent herniated hyperplastic bone marrow.
|
|
|
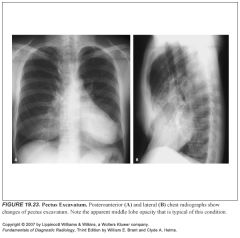
What does pectus excavatum look like on chest x-ray?
|
-Pectus excavatum has a characteristic appearance on frontal chest radiograph.
-The heart is displaced to the left, and the combination of the depressed soft tissues of the anterior chest wall and the vertically oriented anterior ribs results in loss of the right heart border. -The findings on frontal radiographs may be mistakenly attributed to middle lobe opacification from pneumonia or atelectasis. -The typical inward depression of the midsternum and lower sternum is seen on lateral chest radiographs |
|
|
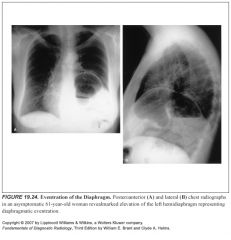
What is eventration of the diaphragm?
|
-Eventration of the diaphragm is a result of congenital absence or underdevelopment of diaphragmatic musculature.
-This produces a localized elevation of the anteromedial portion of the hemidiaphragm on frontal radiographs in older individuals, which is indistinguishable on the right from the rare foramen of Morgagni hernia. |
|
|
How do you diagnose diaphragmatic paralysis?
|
A positive fluoroscopic or ultrasonographic sniff test (paradoxical superior movement of the diaphragm with sniffing, a result of the effects of negative intrathoracic pressure on a flaccid diaphragm during inspiration) is diagnostic.
|
|
|
What is thoguht to be the cause of idiopathic phrenic nerve dysfunction?
What side is it usually on? |
Idiopathic phrenic nerve dysfunction resulting from a viral neuritis is a common cause of diaphragmatic paralysis in male patients and is usually right sided.
|
|
|
What is your differential diagnosis for an elevated diaphragm?
|
-Eventration
-Diminished lung volume (Hypoplastic lung, Lobar/lung atelectasis, Pulmonary resection) -Paralysis (Idiopathic, Iatrogenic phrenic nerve injury, Phrenic nerve crush for tuberculosis, malignant invasion of phrenic nerve, Inflammation of diaphragmatic muscle from pleuritis, lower lobe pneumonia, subphrenic abscess) -Upper abdominal mass (Hepatomegaly or liver mass, splenomegaly, Gastric/colonic distention, Ascites (usually bilateral) -Diaphragmatic hernia* -Subpulmonic pleural effusion* *apparent diaphragmatic elevation |
|
|
What are the three types of nontraumatic diaphragmatic hernias?
Where are the diaphragmatic defects associated with these hernias? |
-Hiatal hernia (through esophageal hiatus)
-Bochdalek (defect in the hemidiaphragm at the site of the embryonic pleuroperitoneal canal) -Morgagni (a defect in the parasternal portion of the diaphragm) |
|
|
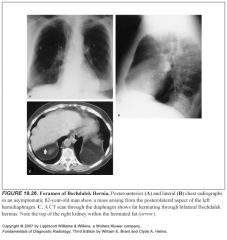
What side are Bochdalek hernias usually on?
What do they look like on imaging? |
-Small hernias through this foramen are common and are predominantly seen on the left side, presumably because of the protective effect of the liver, which prevents herniation of right infradiaphragmatic fat through the right foramen of Bochdalek
-The hernia typically appears as a posterolateral mass above the left hemidiaphragm, although it can occur anywhere along the posterior diaphragmatic surface. -CT shows the diaphragmatic defect with herniation of retroperitoneal fat, omentum, spleen, or kidney. |
|
|
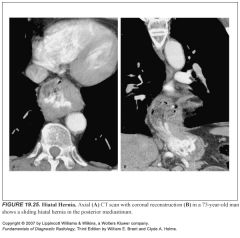
What side are Morgagni hernias usually on?
What do they look like on imaging? |
-A Morgagni hernia is invariably right sided and appears as an asymptomatic cardiophrenic angle mass.
-The diagnosis is made by noting herniation of omental fat, liver, or transverse colon through the paracardiac portion of the right hemidiaphragm on CT scans through the lung bases. -The presence of omental vessels within a fatty paracardiac mass is diagnostic -Coronal MR or US can demonstrate the diaphragmatic defect, distinguishing this entity from partial eventration of the hemidiaphragm. |
|
|
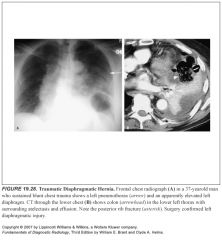
Aside from the presence of abdominal contents in the chest, what are some CT findings in traumatic diaphragmatic rupture?
|
-In addition to the detection of intrathoracic herniation of abdominal contents, MDCT can directly depict the diaphragmatic defect, even in the absence of visceral herniation.
-Other CT findings suggestive of traumatic diaphragmatic injury include thickening or retraction of the diaphragm away from the traumatic injury, a narrowing or waist of the diaphragm on the herniated viscus (“collar” or “waist” sign) and contact between the posterior ribs and the liver (right-sided injury) or stomach (left-sided injury), termed the “dependent viscera” sign. |
|
|
What is the "dependent viscera" sign?
|
-The dependent viscera sign is seen with diaphragmatic rupture.
-The absence of posterior support by the diaphragm allows viscera to “fall” against the posterior ribs to a dependent position. -The dependent viscera sign is said to be present on the right side if the upper one-third of the liver abuts the posterior ribs and on the left side if the stomach or bowel abuts the posterior ribs or lies posterior to the spleen |
|
|
What does bronchial atresia look like on chest x-ray?
|
-A rounded, oval, or branching central lung opacity representing the obstructed, mucus-filled, dilated bronchus (mucocele) with hyperlucency in that portion of lung supplied by the atretic bronchus.
-The overinflated lobe or segment results from air trapping in the obstructed lung as air enters by collateral air drift on inspiration but cannot empty through the proximal tracheobronchial tree on expiration. -The most common site of involvement is the apicoposterior segment of the left upper lobe, followed by the segmental bronchi of the right upper and middle lobes. -The combination of a central mucocele with peripheral hyperlucency in a young, asymptomatic patient is virtually diagnostic of this disorder |
|
|
What is congenital lobar emphysema?
|
-Neonatal lobar hyperinflation (congenital lobar emphysema) may develop from a variety of disorders that produce a check-valve bronchial obstruction.
-These include extrinsic compression by mediastinal bronchogenic cysts, anomalous left pulmonary artery, congenital deficiency of bronchial cartilage, and congenital or acquired bronchial stenosis. -The bronchial obstruction leads to air trapping on expiration, with resultant overinflation of the distal lung. -In order of decreasing frequency, the left upper lobe, right middle lobe, and right upper lobe are the most common sites of involvement. -Radiographically, hyperlucency of the affected lobe is seen with compression of adjacent lung, diaphragmatic depression, and contralateral mediastinal shift -These findings are accentuated on expiratory films or on decubitus films obtained with the affected side down. -CT, particularly when performed in expiration or with the affected side down, shows a hyperlucent, overexpanded lobe with attenuated blood vessels. |
|
|
What is pulmonary sequestration?
How do these patients present clinically? |
-Bronchopulmonary sequestration is a congenital abnormality resulting from the independent development of a portion of the tracheobronchial tree that is isolated from the normal lung and maintains its fetal systemic arterial supply.
-Grossly, the sequestered lung is cystic and bronchiectatic. -These patients most often present with recurrent pneumonia from recurrent infection in the sequestered lung, although some (mostly extralobar sequestrations) are discovered as asymptomatic posterior mediastinal masses on routine radiographs. |
|
|
What are the two types of pulmonary sequestration?
How can you tell them apart? |
-Intralobar sequestration is contained within the visceral pleura of the normal lung.
-Extralobar sequestration is enclosed by its own visceral pleural envelope and may be found adjacent to the normal lung or within or below the diaphragm. -Intralobar sequestration is more common than the extralobar type -Extralobar sequestration is predominantly left sided (90%), whereas one third of intralobar sequestrations are right sided [Extralobar is almost alway on the lEft, Intralobar is sometimes on the rIght]. -A major differentiating feature between the two types is the arterial supply to and venous drainage from the sequestered lung. -An intralobar sequestration is supplied by a single large artery that arises from the infradiaphragmatic aorta and enters the sequestered lung via the pulmonary ligament. -The venous drainage is via the pulmonary veins [this makes sense since it's already inside the visceral pleura] -In contrast, an extralobar sequestration receives several small branches from systemic and occasionally pulmonary arteries, with venous drainage into the systemic venous system (inferior vena cava, azygos, or hemiazygos veins). [It makes sense that extralobar would have both systemic arterial and venous supply since it's outside the visceral pleura] -Additional congenital abnormalities are more common in extralobar sequestration |
|
|
What causes a hypoplastic lung?
|
-Hypoplastic lung is a developmental anomaly resulting in a small lung.
-It occurs secondary to congenital pulmonary arterial deficiency or following compression of the developing lung in utero from a variety of causes. -Grossly, the lung is small, with a decrease in the number and size of airways, alveoli, and pulmonary arteries. -Radiographically, the small lung and hemithorax are associated with ipsilateral diaphragmatic elevation and mediastinal shift, with herniation of the hyperinflated contralateral lung anteriorly toward the affected side. -Hypoplastic lung can simulate total lung collapse radiographically but can usually be distinguished on clinical grounds and review of prior radiographic studies that show a small lung without evidence of pleural or parenchymal scarring. |
|
|
Describe scimitar syndrome:
What are the associated abnormalities? |
-Hypogenetic lung-scimitar syndrome, a variant of the hypoplastic lung, is characterized by an underdeveloped right lung with abnormal venous drainage of the lung to the inferior vena cava just above or below the right hemidiaphragm.
-The systemic venous drainage of the lung produces an extracardiac left-to-right shunt. -The anomalous vein, which drains all or most of the right lung, may be seen as a vertically oriented curvilinear density shaped like a scimitar in the medial right lower lung, thereby giving this syndrome its common name of scimitar syndrome. -The right pulmonary artery is invariably hypoplastic, with supply to all or part of the lung (usually the lower lobe) from the systemic circulation. -Associated anomalies include eventration of the right hemidiaphragm, horseshoe lung (congenital fusion of the right and left lungs posteroinferiorly), and cardiac anomalies such as atrial septal defect (most common), coarctation of the aorta, patent ductus arteriosus, and tetralogy of Fallot. |
|
|
Describe plain film findings of scimitar syndrome:
|
-The frontal chest radiographic findings are diagnostic and include a small right hemithorax with diaphragmatic elevation or eventration, dextroposition of the heart, and herniation of left lung anteriorly into the right hemithorax
-The classic appearance of a solitary scimitar vein is seen in only one third of cases, with the remainder having multiple small draining veins. |
|
|
What syndrome is associated with multiple pulmonary AVMs?
How do patients with pulmonary AVMs present clinically? |
Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome)
-The most common pulmonary symptoms are hemoptysis and dyspnea, the latter attributable to hypoxia caused by the intrapulmonary right-to-left shunt. -Nonpulmonary symptoms most often relate to CNS disease. -Stroke may occur from paradoxical right-to-left cerebral emboli or from thrombosis resulting from secondary polycythemia caused by chronic hypoxemia. -Brain abscess may develop from paradoxical septic emboli. |
|
|
How long does it take for pulmonary contusions to resolve?
What should you think about if they don't resolve? |
-The typical radiographic course is stabilization of opacities by 24 hours and improvement within 2 to 7 days.
-Progressive opacities seen more than 48 hours after trauma should raise the suspicion of aspiration pneumonia or developing ARDS. |
|
|
What's the difference between aspiration pneumonia and aspiration pneumonitis?
|
-Aspiration pneumonia describes a mixed anaerobic infection resulting from the aspiration of infected oropharyngeal contents.
-The aspiration of oropharyngeal or gastric secretions may also occur in a “pure” form uncomplicated by anaerobic infection, producing aspiration pneumonitis. |
|
|
What does chronic aspiration pneumonitis look like on imaging?
|
-With repeated episodes of aspiration over months to years, irregular reticular interstitial opacities may persist, probably representing peribronchial scarring.
-A reticulonodular pattern may be seen, caused by granulomas forming around food particles. -These chronic interstitial abnormalities can be observed in between episodes of acute aspiration pneumonitis. |
|
|
What does lipoid pneumonia look like on CT?
|
-When solitary, lesions can mimic lung cancer.
-CT findings of fat attenuation with a compatible clinical history are diagnostic of this entity |
|
|
What does an acute hypersensitivity reaction to drugs look like on imaging?
What drugs are most commonly responsible? |
-In the lung, this produces bronchospasm or eosinophilic pneumonia, usually associated with fever, skin rash, and blood eosinophilia.
-Radiographically, fleeting peripheral patchy airspace opacities develop hours to days after the initiation of drug therapy. -The opacities often respond to corticosteroid therapy. -The penicillin and sulfonamide antibiotics are the drugs most often associated with hypersensitivity reactions. |
|
|
What do chronic drug hypersensitivity reactions look like on imaging?
What drugs are most commonly involved? |
-The most common form of chronic lung toxicity from drugs is that of a chronic interstitial pneumonitis, with subsequent development of pulmonary fibrosis in the healing phase of this disorder.
-The drugs most commonly implicated in this form of lung disease are amiodarone, nitrofurantoin, and the chemotherapeutic agents Cytoxan (cyclophosphamide), bleomycin, and methotrexate. -Radiographically, there are bilateral predominantly lower lobe coarse reticular and linear opacities with diminished lung volumes. -In patients undergoing chemotherapy for malignancy, the findings are difficult to distinguish from those of lymphangitic carcinomatosis, pulmonary hemorrhage, or opportunistic pneumonia, while pulmonary edema is the major differential diagnosis in patients on amiodarone therapy. -The diagnosis is usually made by excluding one of these other processes. -Pulmonary nodules are an uncommon manifestation of chronic lung injury from bleomycin or Cytoxan, and in this situation, they are radiographically indistinguishable from pulmonary metastases. |
|
|
How might illegal drugs cause pulmonary disease?
Describe the imaging findings: |
-A diffuse alveolar damage that is histologically identical to the early changes of ARDS.
-Opiates, including heroin and crack cocaine, and chemotherapeutic agents, particularly busulfan, cytosine arabinoside, and chlorambucil, are most commonly associated with this reaction. -Radiographically, the lungs show acute interstitial or airspace opacities that are indistinguishable from those of pulmonary edema, although the heart size is usually normal -Characteristically, the edema clears as rapidly as it appeared. -A chronic granulomatous vasculitis may develop as a response to particulate substances such as talc or starch mixed with illicit intravenous drugs. -This can lead to obliteration of the pulmonary vasculature, producing pulmonary hypertension and RV failure. -Radiographically, the lungs may show an interstitial pattern of disease, with enlargement of the central pulmonary arteries and right heart. -The radiographs may rarely show central conglomerate masses that are indistinguishable from progressive massive fibrosis of silicosis or end-stage sarcoidosis. |
|
|
Describe pulmonary toxicity related to bleomycin:
|
-Bleomycin is a cytotoxic antibiotic used in the treatment of lymphoma, squamous cell carcinoma, and testicular cancer.
-Bleomycin-induced lung disease is related to the cumulative dosage of the drug. -Free oxygen radicals within the lung are felt to play a major role in the lung injury and account for the deleterious effects of supplemental oxygen administration in patients with bleomycin toxicity. -The typical radiographic pattern is that of bilateral lower lobe reticular opacities. -A minority of patients will demonstrate acute patchy or confluent airspace opacities as a result of a hypersensitivity reaction to the drug or diffuse alveolar damage. -The reticular or airspace opacities tend to have a basal predominance. -Solitary or multiple pulmonary nodules constitute an unusual radiographic appearance of bleomycin lung toxicity that is indistinguishable radiographically from pulmonary metastases; the lesions generally disappear following cessation of the drug. |
|
|
Describe pulmonary toxicity related to amiodarone:
What does it look like on imaging? |
-Pulmonary toxicity begins months to years after the initiation of therapy.
-CT findings show significant overlap with findings of pulmonary edema—which is common in these patients—with reticulation and ground-glass and airspace opacities, but findings of fibrosis and high attenuation within parenchymal abnormalities should strongly suggest amiodarone toxicity -Amiodarone should be withdrawn or the dose diminished at the earliest sign of toxicity because the drug has an extraordinarily long half life (approximately 90 days). -The cessation of amiodarone at an early stage of toxicity, with occasional use of corticosteroids, usually provides relief. |
|
|
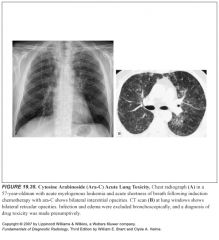
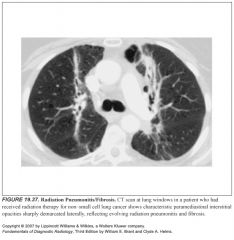
When does radiation pneumonitis occur?
What does the acute phase look like on imaging? |
-Acute radiation fibrosis usually appears 3 weeks after treatment.
-Fibrosis usually occurs after 6-12 months -The parenchymal changes are usually stable by 1 year following radiation therapy. -Acute reactions look like airspace consolidation that conforms to the radiation port -Adhesive atelectasis of the involved portion of lung is common because the radiation produces a loss of surfactant by damaging type 2 pneumocytes -Chronically, fibrosis appears as coarse linear opacities or occasionally as a homogeneous parenchymal opacity with severe cicatrizing atelectasis of the involved portion of the lung. -Pleural thickening caused by fibrosis is a common finding. -Small pleural and pericardial effusions are also common. |
|
|
How can MR be used to tell the difference between radiation pneumonitis and recurrent tumor?
|
Fibrotic tissue is characteristically low signal on T2W MR sequences, a finding that is helpful in distinguishing fibrosis from recurrent tumor, which typically produces high signal on T2WIs.
|

