![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
183 Cards in this Set
- Front
- Back
|
Describe how pyogenic abscess/cerebritis arise:
|
Pyogenic infections of the brain may develop by direct extension following trauma, surgery, sinusitis, dental infections, or otomastoiditis. Hematogenous infections occur even more frequently, especially in patients with lung infections, endocarditis, or congenital heart disease.
|
|
|
Overall, what's the most common organism in pyogenic CNS abscess/cerebritis?
|
Anaerobic bacteria are the most common organisms overall. Infection with Staphylococcus aureus is common after surgery or trauma.
|
|
|
What locations are usually involved with hematogenously spread abscesses?
|
With infections resulting from hematogenous spread, the frontal and parietal lobes (middle cerebral artery distribution) are most commonly involved, with the abscess centered at the gray–white junction.
|
|
|
When a CNS infection is related to sinusitis, what location is typically involved?
|
The frontal lobes are most commonly affected with spread of sinus infections.
|
|
|
What location is typically involved in CNS spread from otomastoiditis?
|
The temporal lobe or cerebellum is involved in patients with spread from otomastoiditis.
|
|
|
List the four stages of CNS abscess formation. When do they occur?
|
Pathologically, there are four stages of evolution of a brain abscess, which correlate with the imaging findings:
1. Early Cerebritis (within the first few days of infection) 2. Late Cerebritis (within 1 or 2 weeks of infection) 3. Early Capsule (within 2 weeks) 4. Late Capsule (2 weeks+). |
|
|
Explain what's going on at the cellular level in early cerebritis:
|
Within the first few days of infection, the infected portion of brain is swollen and edematous. Areas of necrosis are filled with polymorphonuclear leukocytes, lymphocytes, and plasma cells. Organisms are present in both the center and the periphery of the lesion, which has ill-defined margins.
|
|
|
What does early cerebritis look like?
|
-CT scans may be normal or show an area of low density.
-There may be mild mass effect and patchy areas of enhancement within the lesion. -On MR the lesion shows increased signal on proton density images, fluid-attenuated inversion recovery (FLAIR) images, and T2WIs, with low intensity or isointensity on T1WIs. -Enhancement with gadolinium is inconstant at this stage. -Use of high-dose (0.3-mmoL/kg) gadolinium and/or magnetization transfer will increase the likelihood of detecting enhancement. -A ring of enhancement is not present at this stage, distinguishing it from the later three stages. -Unfortunately, these imaging features are nonspecific and can be seen with tumors or infarcts. |
|
|
What's going on at the cellular level in late cerebritis?
|
Central necrosis is increased, with fewer organisms detected pathologically. There is vascular proliferation at the periphery of the lesion, with more inflammatory cells, which represents the brain's effort to contain the infection.
|
|
|
What does late cerebritis look like?
|
-Thick, irregular contrast enhancement at the edges of the lesion on imaging studies.
-Centrally, there is increased signal on FLAIR images and T2WIs. -Diffusion-weighted imaging (DWI) may show some increased signal within the center of the lesion. -Vasogenic edema is seen outside the enhancing rim at this stage as well. -Delayed scans may show central filling in with contrast. -No discrete, low-signal capsule is evident on T2WIs, in distinction to some mature abscesses. |
|
|
How is early cerebritis managed?
|
Antibiotics alone. All the other stages of abscess formation tend to be treated with surgery.
|
|
|
What's going on at the cellular level in early abscess capsule formation?
|
-The infection is walled off as a capsule of collagen and reticulin forms in the inflammatory, vascular margin of the infection.
-Macrophages, phagocytes, and neutrophils are also present in the capsule. -The necrotic center contains very few organisms. |
|
|
What does an early capsule formation of a CNS abscess look like?
|
-Contrast-enhanced CT and MR scans show a well defined rim of enhancement.
-The rim tends to be low in signal on T2WIs. -Centrally there is necrosis (low density on CT, low signal on T1WIs, and high signal on intermediate images, FLAIR images, and T2WIs). -Prominent surrounding vasogenic edema is usually present. -There is increased signal centrally on DWI, which is very helpful in distinguishing abscesses from necrotic tumors, which are not usually bright on diffusion. |
|
|
What does late capsule formation of a CNS abscess look like?
|
-In the late capsule stage, the rim of enhancement becomes even better defined and thin
-Multiloculation is common. -The capsule often exhibits characteristic MR features that are helpful diagnostically at this stage. On T1WIs, the capsule is usually isointense or hyperintense to white matter, and on T2WIs it is usually hypointense to white matter. -There is marked increased signal centrally on DWI, which is a very helpful imaging feature. -The inner aspect of the enhancing capsule is often (about 50% of the time) thinner than the peripheral aspect. -This thin medial rim predisposes to intraventricular rupture, with resulting ependymitis/ventriculitis. -CT or MR scans reveal enhancement of the ependymal lining of the ventricle and sometimes abnormal density/signal intensity of the intraventricular CSF. |
|
|
Complications of a CNS abscess?
|
-Ventriculitis
-Infarction -Hydrocephalus |
|
|
Differential for a CNS abscess? What tells you that it's an abscess?
|
-The differential diagnosis of pyogenic abscess includes tumor and resolving hematoma.
-The clinical features, combined with the appearance of central high signal on DWI, thin enhancing rim (thinnest medially), much edema, and paramagnetic effects in the capsule (with no blood products centrally), should strongly suggest a brain abscess. |
|
|
What do septic emboli look like?
|
-Infections that begin with a septic embolus may not have the typical appearance of an abscess.
-The embolus frequently causes an infarct that dominates the imaging findings. -Depending on the size of the embolus, there may be a small rounded area of enhancement or a larger, wedge-shaped cortical infarct. -As with other embolic infarcts, hemorrhage may occur. -Because the nonviable, infarcted tissue has a poor blood supply, a typical capsule may not form. -A thicker, more irregular ring of enhancement that persists within an area of infarction should suggest the diagnosis. |
|
|
Name a complication that is specific to septic emboli:
|
Septic emboli may lead to mycotic aneurysm formation, which can result in intraparenchymal or subarachnoid hemorrhage.
|
|
|
What is listerial rhombencephalitis?
|
Listerial rhombencephalitis involves the brainstem and cerebellum.
|
|
|
What kind of pts get CNS listerial infections? What are its manifestations?
|
Listeria monocytogenes is an anaerobic gram-positive bacillus that primarily infects immunocompromised patients. It's a TORCH infection as well. The organism can cause meningitis, meningoencephalitis, and abscesses. Listerial rhomboencephalitis is another manifestation.
|
|
|
What does listerial rhombencephalitis look like?
|
MR scans reveal areas of abnormal signal and enhancement in the brainstem and cerebellar white matter tracts. The appearance is similar to that of acute disseminated encephalomyelitis
|
|
|
What are the different CNS manifestations of tuberculosis?
|
The most common form of CNS mycobacterial infection is tuberculous meningitis. Focal mycobacterial infection of the brain occurs in two forms: tuberculoma and abscess.
|
|
|
What's the difference between a tuberculoma and a tuberculosis abscess?
|
-A tuberculoma is a granuloma with central caseous necrosis.
-A tuberculous abscess is a rare complication that has characteristics similar to those of a pyogenic abscess, but it develops in patients with impaired T-cell immunity. -Most tuberculomas are not associated with tuberculous meningitis. -Symptoms develop more rapidly in tuberculosis abscesses than with tuberculomas. |
|
|
What do CNS tuberculomas look like?
|
-Most lesions in adults are supratentorial, involving the frontal or parietal lobes.
-Sixty percent of tuberculomas in children are in the posterior fossa, usually the cerebellum. -Multiple lesions are common. -An abnormal chest radiograph is present in up to 50% of patients. -Noncontrast CT scans show one or more isodense or slightly hyperdense nodules or small mass lesions. -Multiple lesions are present about 50% of the time. -The center of the tuberculoma is usually denser than the fluidlike center of a pyogenic abscess because of caseous necrosis. -A “target” appearance, with a central calcification surrounded by rim enhancement, is an uncommon but helpful finding, strongly suggesting the diagnosis. -Calcification is present in fewer than 5% of cases at the initial diagnosis but is commonly seen with treatment as the lesions resolve. -With MR, tuberculomas may be high or low in signal intensity with T2WIs, depending upon the size of the lesion and the water content of the caseous necrosis. -The wall of the tuberculoma is often low in signal on T2WIs. -There is significant enhancement after gadolinium administration, with a solid nodular or thick ring-shaped appearance. -There may or may not be increased signal on DWI, unlike bacterial infections, which usually show restricted diffusion. -Surrounding edema is often mild. |
|
|
Differential for an apparent CNS tuberculoma?
|
The differential diagnosis includes tumor, pyogenic abscess, fungal and parasitic infections, and sarcoidosis.
|
|
|
Why do immunocompromised patients form TB abscesses rather than tuberculomas?
|
Abnormal T-cell function prevents the normal host response of tuberculoma formation with caseous necrosis.
|
|
|
What does a tuberculosis abscess look like?
|
-The imaging features are similar to that seen with pyogenic abscesses.
-The lesions are often large and multiloculated, in distinction to tuberculomas. -Prominent edema and mass effect also distinguish tuberculous abscess from tuberculoma. |
|
|
What fungal infections can occur in both immunocompetent and immunocompromised hosts?
|
Coccidioidomycosis, North American blastomycosis, and histoplasmosis.
|
|
|
Where are the geographic areas associated with coccidioidomycosis, North American blastomycosis, and histoplasmosis?
|
-Coccidioidomycosis occurs in the southwestern United States.
-Blastomycosis occurs in the Ohio and Mississippi River valleys. -Histoplasmosis is usually a benign, asymptomatic infection, occurring in the Midwest and southern United States. |
|
|
Describe CNS manifestations of blastomycosis:
|
-Meningitis is the most frequent presentation, but parenchymal abscesses and granulomas occur more frequently than with coccidioidomycosis or histoplasmosis.
-Epidural granulomas and abscesses also occur in the head and spine, usually from direct extension from bone infection. -Up to 40% of focal brain lesions are multiple. |
|
|
Describe CNS manifestations of histoplasmosis:
|
-Dissemination is unusual, and only a small percent of disseminated cases involve the CNS.
-Meningitis is most common, but multiple or solitary granulomas may occur. -Abscesses are unusual. |
|
|
Describe the appearance of CNS fungal infections:
|
-As seen with CT or MR, most fungal granulomas are small and show solid or thick rim enhancement.
-Fungal abscesses (as sometimes seen with blastomycosis) have an appearance similar to that of the pyogenic abscesses. - Meningeal enhancement from meningitis is a common accompanying feature. -Hydrocephalus is also common, especially with coccidioidomycosis. |
|
|
Which fungal agents are seen in immunocompromised hosts?
|
Cryptococcosis, aspergillosis, mucormycosis, and candidiasis.
|
|
|
Describe CNS lesions of aspergillus:
|
-The infection may arise from hematogenous spread or by direct extension from an infected paranasal sinus, leading to meningitis or meningoencephalitis.
-Parenchymal disease usually takes the form of an abscess. -Granulomas are unusual. -The abscesses are often multiple and show irregular ring enhancement. -Subcortical or cortical infarcts and hemorrhage from blood vessel invasion may occur. |
|
|
What patients get mucormycosis? How does it arise?
|
Mucor invades the brain usually by direct extension from the sinuses, nose, or oral cavity, but hematogenous spread also occurs. Almost all patients are diabetic or otherwise immunocompromised.
|
|
|
What does mucormycosis look like?
|
-Like aspergillosis, mucormycosis tends to invade blood vessels. Imaging studies in patients with CNS mucormycosis will reveal single or multiple mass lesions with varying degrees of peripheral enhancement.
-The amount of enhancement depends upon the compromised host's ability to fight the infection. -Surrounding edema is variable in amount. -Smaller lesions will show a solid enhancement pattern. -The lesions are often in the base of the brain, adjacent to diseased sinuses. -Infarcts, intra-axial or extra-axial hemorrhage, and meningeal enhancement can be seen with CT or MR. |
|
|
Describe CNS candidal infections:
|
-Candidiasis usually causes meningitis, but granulomas and small abscesses may occur.
-In cases of CNS candidiasis, meningeal enhancement or multiple small enhancing granulomas or microabscesses are usually seen. -Infarcts, hydrocephalus, and large abscesses may also be identified. |
|
|
What's the most common CNS fungal infection?
|
Cryptococcosis is the most frequently reported CNS fungal infection.
|
|
|
What do CNS cryptococcal infections look like?
|
-The usual manifestation is meningitis.
-Granulomas can occur and are usually multiple. -Abscesses are less common. -CT scans in patients with cryptococcosis are usually normal, reflecting relatively mild meningeal involvement in most cases. -Mass lesions are seen in about 10% of cases. -Cryptococcomas are shown as small, usually multiple, solid-enhancing, peripheral parenchymal nodules. -Calcifications within a granuloma are occasionally seen. -Leptomeningeal nodules are often only seen on T1W, contrast-enhanced MR as multiple tiny enhancing lesions near the basal cisternae and sulci. -Diffuse meningeal enhancement is unusual. -Granulomas may show either solid or ring enhancement. -Another characteristic cryptococcal lesion is the gelatinous pseudocyst. -This is a cystic lesion, usually in the basal ganglia, representing enlarged Virchow-Robin spaces filled with the organism. -These lesions are usually found only in immunocompromised patients. -Viewed on CT, gelatinous pseudocysts are smooth, round, low-density masses in the basal ganglia which show no contrast enhancement. -They are usually better seen with MR than with CT, as lesions are nearly isointense with CSF on all sequences that do not enhance. |
|
|
What types of parasitic infections are encountered in the US?
|
The most common infections likely to be encountered in the United States are cysticercosis, echinococcosis, toxoplasmosis, and rarely amebiasis.
|
|
|
What's the organism that causes cysticercosis?
|
Cysticercosis is caused by the larvae of the pork tapeworm Taenia solium.
|
|
|
Four different types of cysticercosis:
|
-Parenchymal (most common)
-Intraventricular -Meningeal (racemose) -Spinal |
|
|
Describe the different stages of parenchymal cysticercosis and their imaging characteristics:
|
-Early in the infestation, during the tissue invasion stage, CT or MR scans show edema and/or nodular enhancement.
-Later, the viable cysts appear as small (usually 1 cm or less), solitary or multiple rounded lesions that are low density on CT and isointense to CSF on MR. -The lesions are usually peripherally distributed near the gray–white junction or in the gray matter. -A small marginal nodule representing the scolex is sometimes seen. -There is usually no enhancement or edema at this vesicular stage. -When the cyst dies, the fluid within it leaks into the surrounding brain, causing inflammation. -This produces clinical symptoms of an acute encephalitis, which may be severe, depending on the number of lesions. -Imaging studies now reveal ring-enhancing lesions with surrounding edema. -The cyst fluid is of increased density on CT and increased signal compared with CSF on T1W and T2W MR. -As the dead cyst degenerates, it becomes smaller, showing nodular enhancement, and then calcifies. -CT scans at this late stage show small, peripheral calcifications, with no edema or enhancement. -With MR, the calcifications are best seen on T2W or T2*W GRE images, but they are better demonstrated by CT. |
|
|
What does intraventricular cysticercosis look like?
|
-The cysts are usually isodense and isointense to CSF, making them difficult to visualize.
-MR is superior to CT for imaging, as subtle signal changes and lack of CSF pulsations within the cyst makes them more visible. -Enhancement may or may not be present, depending on the stage of disease, similar to the parenchymal form. -The cysts may obstruct the foramen of Monro, the third ventricle, or the cerebral aqueduct, resulting in hydrocephalus. -If acute hydrocephalus occurs, death may rapidly ensue. -Ventriculitis occurs if the cyst ruptures. |
|
|
What does meningeal/meningobasal/racemose cysticercosis look like?
|
-Meningeal infestation is known as meningobasal (because the basal cisterns are most frequently involved) or racemose (Latin for “clusters”) cysticercosis.
-The cysts lack a scolex but may grow by proliferation of the cyst wall. -The cysts may grow in grapelike clusters or conform to the shape of the cistern. -No mural nodules or calcifications are seen. -CT scans show CSF-density cysts in the basal cisterns. -MR reveals cysts that are isointense with CSF, often with mural enhancement or diffuse meningeal enhancement. -Hydrocephalus is commonly observed. |
|
|
What does spinal cysticercosis look like?
|
-Spinal cysticercosis is usually intradural, but can be either intramedullary or extramedullary.
-Intramedullary lesions are best seen with MR as solid or ring-enhancing cord lesions, similar to that seen in the brain parenchyma. -Extramedullary cysts are analogous to the racemose form |
|
|
What is the etiologic agent of echinococcosis
|
The etiologic agent is the dog tapeworm
|
|
|
What is echinococcosis also known as?
|
It's also known as hydatid disease
|
|
|
Where are hydatid cysts typically found?
|
Hydatid cysts are most frequently present in the lung and liver, but the brain is involved in 1% to 4% of cases.
|
|
|
What do CNS hydatid cysts look like?
|
The cysts are usually solitary, unilocular, large, round, and smoothly marginated. They are most often supratentorial, in the middle cerebral artery territory. There may rarely be mural calcification. With CT, the fluid within the cyst is usually isodense with CSF. There is usually no surrounding edema or abnormal contrast enhancement, unless the cyst has ruptured, leading to an inflammatory reaction. With MR, the lesions are usually nearly isointense with CSF.
|
|
|
What patients get toxoplasmosis?
|
The disease may be either congenital or acquired. The acquired form is seen primarily in immunocompromised patients and is very common in AIDS patients, as will be discussed later. The congenital form results when a pregnant woman eats poorly cooked meat or is infected by a cat.
|
|
|
What does congenital toxoplasmosis look like? How does the fetus get infected?
|
The congenital form results when a pregnant woman eats poorly cooked meat or is infected by a cat. A diffuse encephalitis of the fetal brain ensues, usually causing severe destruction. The infant is usually born with microcephaly (Fig. 6.14), chorioretinitis, and mental retardation. Imaging studies reveal atrophy, dilated ventricles, and calcifications. The calcifications occur in the periventricular white matter, basal ganglia and cerebral hemispheres. This is in distinction to congenital cytomegalovirus (CMV), in which the calcifications are usually periventricular only.
|
|
|
What's the name of the infection people get when they're swimming in brackish water?
|
Amebic meningoencephalitis
|
|
|
What does CNS amebic meningoencephalitis look like?
|
Amebic meningoencephalitis is sometimes seen in the southern United States. The amebae enter the nasal cavity of patients swimming in infested freshwater ponds or pools. There is direct extension through the cribriform plate to the brain. Severe meningoencephalitis results and is usually fatal. Imaging studies often underestimate the severity of the disease. Early in the infection, there may be meningeal and/or gray matter enhancement. Later, there is diffuse cerebral edema. There are a few reports of single or multiple, ring-enhancing or solid-enhancing lesions with surrounding edema in patients with amebic brain abscesses.
|
|
|
Who gets neurosyphilis?
|
-Neurosyphilis develops in about 5% of patients who are not treated for the primary infection.
-Because of effective antibiotic therapy, the disease is rare. However, there has been a significant increase in incidence since the AIDS epidemic. -Neurosyphilis is more likely to develop in HIV-infected patients, and the neurologic symptoms occur after a shorter latency period than in uninfected patients. |
|
|
Symptoms of neurosyphilis?
|
Patients with neurosyphilis are usually asymptomatic. Symptomatic patients may have an aseptic meningitis, tabes dorsalis (posterior column neuropathy), general paresis, or meningovascular disease.
|
|
|
What do gummas from neurosyphilis look like?
|
These usually appear as small enhancing nodules at the surface of the brain, with adjacent meningeal enhancement.
|
|
|
What does meningovascular neurosyphilis look like?
|
-Meningovascular syphilis presents as an acute stroke syndrome or a subacute illness with a variety of symptoms.
-Pathologically, there is thickening of the meninges and a medium to large vessel arteritis. -Imaging studies reveal small infarcts of the basal ganglia, white matter, cerebral cortex, or cerebellum. -The infarcts may exhibit patchy or gyriform enhancement, which is best seen with MR. -Meningeal enhancement is unusual, but cranial nerve enhancement in patients with syphilitic cranial neuritis has been described. -Angiography in patients with meningovascular neurosyphilis reveals multiple segmental constrictions and/or occlusions of large and medium arteries, including the distal internal carotid, anterior cerebral, middle cerebral, posterior cerebral, and distal basilar arteries |
|
|
What do lyme disease look like?
|
-In patients with cranial neuritis, MR scans may show thick, enhancing cranial nerves.
-Cranial nerves III to VIII can be involved, with the facial nerve most commonly affected. -In patients with parenchymal CNS Lyme disease, MR scans show multiple small white matter lesions, similar to that seen with multiple sclerosis. -The lesions can be found in the supratentorial and infratentorial white matter tracts. -The lesions often enhance with contrast in a nodular or ring pattern, depending on the size. -There may be meningeal enhancement. |
|
|
Differential for lyme disease?
|
The differential diagnosis includes multiple sclerosis and other demyelinating processes.
|
|
|
What are the most common CNS viral infections?
|
The most common viral infections of the CNS include CMV, herpes simplex, varicella zoster, and HIV
|
|
|
How is CMV transmitted?
|
-It causes symptomatic CNS disease primarily through congenital transmission.
-Maternal CMV infection results in transplacental transmission to the fetus in 30% to 50% of cases and symptomatic disease in 5%. -CMV infection in adults is unusual, except in immunosuppressed patients. |
|
|
Imaging findings of congenital CMV?
|
-The intracranial manifestations of congenital CMV infection largely depend upon the time of infection during gestation.
-Infection in the first trimester results in necrosis in the germinal matrix, resulting in migrational anomalies. -MR scans may show a spectrum of abnormalities, including agyria, polymicrogyria, and focal cortical dysplasia. -Delayed myelination and cerebellar hypoplasia are also common findings. -Patients infected later during gestation may have a normal gyral pattern, but delayed myelination and periventricular white matter lesions are often seen. -The most common finding with CT scanning is periventricular calcification. -These are detected better with CT than MR. -There are usually no calcifications of the basal ganglia or cortices, as is seen in congenital toxoplasmosis. -Parenchymal atrophy and ventriculomegaly are common. |
|
|
Prenatal ultrasound findings in CMV?
|
-The disease has been diagnosed in utero with obstetric US.
-Periventricular hyperechoic calcifications, preceded by hypoechoic periventricular ringlike zones, are characteristic findings. |
|
|
How is congenital herpes infection spread?
|
-The infant is usually infected during descent through the birth canal when the mother has genital (type 2) herpes.
-Occasionally there is transplacental transmission before delivery, but this usually results in spontaneous abortion. |
|
|
Which patient population gets herpes encephalitis most commonly?
|
Herpes simplex encephalitis occurs most frequently in neonates.
|
|
|
Signs/symptoms of neonatal herpes encephalitis?
|
-The infection causes a severe encephalitis, which is either fatal or has severe neurologic consequences.
-The patient usually presents with seizures in the second to fourth week of life. -If the patient survives, varying degrees of microcephaly, mental retardation, microphthalmia, enlarged ventricles, intracranial calcifications, and multicystic encephalomalacia may occur. |
|
|
What does neonatal herpes encephalitis look like?
|
-Early in the course of the encephalitis, CT scans may reveal diffuse brain swelling or bilateral patchy areas of decreased density in the cerebral white matter and cortex, with relative sparing of the basal ganglia, thalami, and posterior fossa structures
-Cranial sonography will show areas of increased echogenicity corresponding to these low-density zones. -The low-density lesions progress to areas of necrosis, which are sometimes hemorrhagic and may eventually calcify. -Multicystic ephalomalacia is the end result. -Increased density in the cortical gray matter is characteristic during this late stage. -With MR there is decreased gray–white matter contrast early in the infection, reflecting gray matter edema. -Later, there is decreased signal on T2WIs within the thinned cortical gray matter. |
|
|
Is adult herpes encephalitis a primary infection or reactivation of latent infection?
|
The infection usually is secondary to reactivation of latent herpes simplex type 1.
|
|
|
Signs/symptoms of adult herpes encephalitis?
|
-Patients with herpes encephalitis present with the gradual onset of personality changes, dysphasia, and focal neurologic deficits. Seizures and coma may occur.
-An inconstant but characteristic electroencephalographic finding is a localized spiked and slow wave pattern. |
|
|
Mortality rate in adult herpes encephalitis?
|
-Early diagnosis is crucial, because there is a greater than 70% mortality rate in untreated patients.
-Treatment is with acyclovir, which significantly reduces mortality, but many survivors have permanent deficits. |
|
|
Is herpes encephalitis an imaging diagnosis or a clinical one?
|
Unfortunately, it's kinda neither. You have to have a high clinical and imaging suspicion. Also unfortunately, CSF studies are often negative.
|
|
|
Why does herpes encephalitis have a predilection for the temporal lobes?
|
The predilection for the temporal lobes is because the virus is usually latent within the gasserian ganglion.
|
|
|
What parts of the brain does herpes encephalitis like to involve?
|
-Temporal lobes--everybody knows that, BUT
-The frontal lobes may also be involved. -The insular cortex is often involved, but the adjacent putamen is usually spared. |
|
|
What does adult herpes encephalitis look like?
|
-CT scans show a poorly defined area of decreased density in one or both temporal lobes.
-There is usually swelling with mass effect. -Streaky enhancement is variable. -The CT findings are not usually seen before the fifth day of symptoms. -With MR, the findings may be identified somewhat sooner. -There is a nonspecific pattern of increased signal on the intermediate, FLAIR, and T2W images in the temporal and/or frontal lobe(s) with sparing of the putamen. -This increased signal is best seen on a FLAIR sequence. -Increased signal on DWI has been reported. -Early on, meningeal enhancement may be seen. -Later, there may be parenchymal enhancement or evidence of hemorrhage. |
|
|
Differential diagnosis for imaging suggestive of herpes encephalitis?
|
The differential diagnosis includes middle cerebral artery infarct (which will often involve the putamen, unlike herpes), early bacterial cerebritis, and other types of viral encephalitis
|
|
|
What are the CNS manifestation if varicella zoster?
|
Varicella zoster rarely causes an encephalitis that is similar to that caused by herpes simplex. Another unusual manifestation is the syndrome of herpes zoster ophthalmicus and delayed contralateral hemiparesis caused by cerebral angiitis.
|
|
|
Describe zoster ophthalmicus? What is associated with it? What does it look like?
|
In this syndrome, there are cerebral infarcts resulting from large and medium vessel angiitis on the same side as ophthalmic zoster skin manifestations. Imaging studies show typical infarcts, and angiography shows segmental areas of narrowing and/or beading of the arteries.
|
|
|
What is Ramsay Hunt syndrome?
|
-Caused by varicella zoster of the seventh cranial nerve
-Clinically, there is ear pain and facial paralysis, accompanied by a vesicular eruption about the ear. |
|
|
Which cranial nerve is most commonly affected by herpes zoster neuritis? What is this called?
|
-Facial nerve
-Ramsay Hunt syndrome |
|
|
Imaging findings in Ramsay Hunt syndrome?
|
CT scans are usually normal, but MR may reveal increased contrast enhancement of the facial nerve.
|
|
|
What causes ADEM?
|
Acute disseminated encephalomyelitis (ADEM) is an acute demyelinating disease that occurs after a viral infection, following a vaccination, or sometimes spontaneously. It probably has an autoimmune basis; organisms are not isolated from brain tissue.
|
|
|
Signs/symptoms of ADEM?
|
Symptoms develop acutely: fever, headache, and meningeal signs. Seizures, focal neurologic deficits, stupor, and coma may develop.
|
|
|
Mortality rate in ADEM?
|
The mortality rate is 10% to 20%. When treated early with steroids, most patients make a full recovery.
|
|
|
What does ADEM look like?
|
-T2WIs and FLAIR imaging are much more sensitive than CT in identifying lesions of increased signal intensity in the white matter.
-The brainstem, cerebellum, and basal ganglia are often involved. -Optic neuritis is also common. -The lesions are usually multiple, but few in number. -Sometimes there is solid or ring enhancement of the lesions. -The appearance is similar to that seen in multiple sclerosis, but with a monophasic clinical course. -The lesions regress with successful treatment, correlating with clinical improvement. |
|
|
What is the severe form of ADEM called?
What does it look like? |
-Acute hemorrhagic leukoencephalitis is a severe variant of ADEM that is often fatal.
-The major imaging feature is a rapid progression of white matter lesions over the course of a few days. |
|
|
What causes SSPE?
|
Subacute sclerosing panencephalitis is caused by a variant of the measles virus.
|
|
|
Who gets SSPE? Signs/symptoms? Treatment?
|
It typically occurs in children and young adults who had measles before age 2, after a 6- to 10-year asymptomatic period. The disease causes progressive dementia, seizures, and paralysis, leading to death. There is no treatment.
|
|
|
Imaging findings in SSPE?
|
-Imaging studies initially reveal focal lesions in the gray matter and subcortical white matter.
-Later, there are periventricular white matter lesions that may enhance. -In the late stages there is usually profound cortical atrophy. |
|
|
Imaging features of japanese encephalitis?
What is this similar to? |
-Japanese encephalitis is a flaviviral encephalitis found in Asia.
-Bilateral thalamic and basal ganglia lesions are typical of this disease. -West Nile disease |
|
|
What does West Nile encephalitis look like?
|
-This is a mosquito-borne infection that results in a meningoencephalitis of variable clinical severity.
-As with Japanese encephalitis, MR shows increased signal on T2WIs in the thalami and basal ganglia |
|
|
What is Rasmussen encephalitis? What does it look like?
|
-Rasmussen encephalitis is a devastating disease of childhood, most likely of viral etiology.
-There are intractable seizures and progressive neurologic deficits. -The disease usually affects one cerebral hemisphere. -Imaging studies show severe atrophy of the involved hemisphere. -PET scans show the hemisphere to be hypometabolic. |
|
|
What's the syndrome where seizures and neurologic deficits are associated with severe atrophy of one cerebral hemisphere?
|
Rasmussen encephalitis
|
|
|
Signs/symptoms of Creutzfeldt-Jakob disease?
|
Clinically, there is rapidly progressive dementia, ataxia, and myoclonus, leading to death.
|
|
|
Imaging findings in Creutzfeldt-Jakob disease?
|
-Conventional MR scans are often normal early in the disease.
-DWI frequently demonstrates increased signal in the cerebral cortex and basal ganglia in early cases. -Atrophy and increased signal in the cortex and basal ganglia on FLAIR and T2W images develop as the disease progresses. -MR scans usually show characteristic findings of increased T2 signal in the pulvinar (posterior) nuclei of the thalamus. |
|
|
What's the bug to think of for meningitis in teens and young adults?
|
Neisseria meningitidis
|
|
|
What bugs do you think of for meningitis in a neonate?
|
Escherichia coli, group B streptococcus, and Listeria monocytogenes occur commonly in neonates.
|
|
|
What does acute meningitis look like on CT?
|
-They are usually normal.
-The inflammatory exudate caused by the meningitis may occasionally produce high density within the subarachnoid spaces, similar to that seen in subarachnoid hemorrhage. -The increased density is often more pronounced in the peripheral sulci than in the basal cisterns, unlike most cases of aneurysmal bleeding. -Diffuse cerebral edema is sometimes seen. -If contrast is given, there may or may not be meningeal enhancement. |
|
|
Complications of meningitis?
|
-Hydrocephalus
-Cerebritis/abscess -Ventriculitis -Venous or arterial infarctions. -Subdural effusions may be seen in infants, especially with H influenza meningitis. The hydrocephalus that may develop is usually of the communicating type, reflecting decreased function of the arachnoid villi in absorbing CSF. |
|
|
Imaging findings of meningitis specific to neonates?
|
-Subdural effusions may be seen in infants, especially with H influenza meningitis.
-With CT and MR, subdural effusions appear as thin collections along the surface of the brain that are isodense/isointense with CSF. -These sterile effusions can be identified with cranial sonography in infants. |
|
|
Findings of meningitis on neonatal cranial USG?
|
-Subdural effusions appear as thin collections along the surface of the brain that are isodense/isointense with CSF
-Echogenic sulci -Ventriculomegaly -Abnormal parenchymal echogenicity |
|
|
What type of mycobacterium causes tuberculous meningitis?
|
It is usually caused by Mycobacterium tuberculosis, but atypical mycobacteria, such as M avium-intracellulare can cause meningitis in AIDS patients.
|
|
|
Which patient population gets tuberculous meningitis?
|
Tuberculous meningitis has a predilection for infants and children but is seen in all age groups.
|
|
|
How does tuberculosis get into the meninges?
|
The disease spreads to the meninges hematogenously from the lungs, but the chest radiograph is normal in 40% to 75% of patients.
|
|
|
What if you think the patient has tuberculous meningitis, but the cxr and TB skin test are negative?
|
-It's still possible.
-The chest x-ray is normal in 40-75% of patients. -The tuberculin skin test is also frequently negative. |
|
|
Clinical presentation of tuberculous meningitis?
|
Clinically there is usually a subacute or insidious onset of headache, malaise, weakness, apathy, or focal neurologic findings.
|
|
|
What does tuberculous meningitis look like?
|
-Imaging studies will show enhancing, thickened meninges, especially near the base of the brain, unlike bacterial meningitis, where the peripheral meninges are more often involved.
-The often marked thickening of the meninges also distinguishes tuberculous and other granulomatous meningitides from pyogenic meningitis. -The thick exudate in the basal cisterns may extend into the Virchow-Robin spaces, causing a vasculitis. -This frequently leads to infarcts, which are better detected with MR than with CT. -Communicating hydrocephalus is another relatively common complication. |
|
|
Differential for the appearance of tuberculous meningitis?
|
The differential diagnosis of tuberculous meningitis includes fungal meningitis, racemose cysticercosis, sarcoidosis, and carcinomatous meningitis.
|
|
|
What does fungal meningitis look like?
|
-Fungal meningitis usually causes thick meningeal enhancement in the basal cisterns, as with tuberculosis.
-Enhancement is variable with cryptococcosis, depending on the immune status of the patient. -Hydrocephalus is common, but infarcts and extension of fungal meningitis into the brain occur less frequently than with tuberculous or pyogenic meningitis (except in cases of aspergillosis and mucormycosis). |
|
|
What imaging findings would steer you towards racemose cysticercosis instead of fungal or TB meningitis?
|
Racemose cysticercosis may show thick meningeal enhancement, but cystic lesions in the cisterns are also frequently found
|
|
|
Describe findings in neurosarcoid:
|
-It primarily affects the leptomeninges, so that abnormal meningeal enhancement is seen with CT or MR.
-Focal parenchymal enhancing mass lesions or nonenhancing small white matter lesions may also be seen. |
|
|
Imaging findings in viral meningitis?
|
Imaging studies are typically normal.
|
|
|
What sorts of things cause epidural abscess of the brain?
|
An epidural abscess may be caused by penetrating injuries, surgery, sinusitis, mastoiditis, orbital infection, or, rarely, hematogenous spread.
|
|
|
Imaging findings in epidural abscesses?
|
-CT scans show an inwardly convex, extra-axial collection with increased density compared to CSF.
-The inner margin usually enhances with contrast. -There may be adjacent sinusitis or skull abnormalities. -MR is more sensitive in demonstrating these lesions and can do so in multiple planes. -Cortical venous thrombosis resulting in venous infarcts is a common result of these infections. -Subdural empyemas show increased signal on DWI, distinguishing them from subdural effusions |
|
|
Do epidural abscesses spread quickly?
|
-The strong dural attachments prevent rapid expansion of epidural abscesses.
-However, a subdural empyema may spread rapidly throughout the subdural space and is acutely life threatening. |
|
|
How can you tell a subdural empyema from a subdural fluid collection on MR?
|
Subdural empyemas show increased signal on DWI, distinguishing them from subdural effusions
|
|
|
What sorts of things can cause meningeal enhancement (aside from meningitis)?
|
-Mild, smooth dural, or meningeal enhancement may be seen after brain surgery and in patients with a ventriculostomy tube, especially with MR.
-The enhancement can persist for years and should be considered benign in this clinical setting. -It most likely reflects a chemical meningitis resulting from perioperative hemorrhage. -Intracranial hypotension from a spontaneous or iatrogenic CSF leak also results in smooth dural thickening and enhancement. |
|
|
What portion of AIDS pts have CNS manifestations?
|
The incidence of CNS involvement has decreased since the introduction of highly active antiretroviral therapy (HAART), yet up to two thirds of AIDS patients develop some kind of CNS disease.
|
|
|
List the most common CNS infections found in HIV pts: What are the most common CNS tumors?
|
-The most common infections include HIV encephalopathy; toxoplasmosis, cryptococcosis, and other fungal infections; CMV and Herpes meningoencephalitis; mycobacterial infection; PML; and meningovascular syphilis.
-Primary CNS lymphoma is by far the most common tumor, but metastatic lymphoma, gliomas, and rarely Kaposi sarcoma may also occur. |
|
|
Where does HIV encephalopathy usually occur in the brain?
|
-The centrum semiovale is involved most severely, but all white matter tracts, including the brainstem and cerebellum, may be affected.
-The cortical gray matter is usually spared. |
|
|
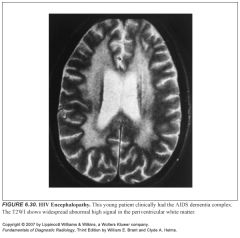
What does HIV encephalopathy look like clinically?
|
Clinically, patients with HIV encephalitis may develop a subcortical dementia with cognitive, behavioral, and motor deterioration. This is known as AIDS dementia complex (ADC), which occurs in about 7% to 15% of AIDS patients
|
|
|
What is the most common form of CNS disease in pediatric patients with AIDS? How does it present?
|
-HIV encephalopathy
-Infants and children with HIV encephalitis exhibit loss of developmental milestones, apathy, failure of brain growth, and spastic paraparesis. -This is the most common form of CNS disease in pediatric patients with AIDS, in whom opportunistic infections and CNS tumors are unusual. |
|
|
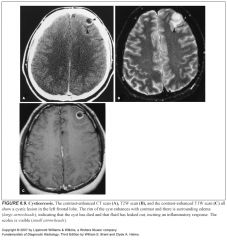
What does HIV encephalopathy look like?
|
-Diffuse atrophy is the most common manifestation
-This is largely central atrophy, reflecting the predominant white matter involvement. -White matter lesions are also commonly seen in patients with ADC. -MR is significantly more sensitive than CT for detecting these abnormalities. -A diffuse pattern of increased signal in the deep white matter or multiple small punctate white matter lesions on T2WIs are the most common findings. -The punctate lesions do not correlate well with symptoms. -The lesions do not exhibit mass effect or abnormal contrast enhancement. -The most severe cases of HIV encephalopathy show extensive bilateral areas of abnormal signal throughout the periventricular white matter, brainstem, and cerebellum. -A decreased n-acetyl aspartate (NAA) peak is often found in the affected white matter with MR spectroscopy. -The clinical and imaging abnormalities often respond to treatment with HAART. -In infants and children with HIV infection, atrophy is the most common observation, followed by calcifications in the basal ganglia. -White matter calcifications and low-density lesions are also sometimes seen. |
|
|
What CD4 count is CNS toxoplasmosis associated with?
|
occurs in patients with CD4 counts below 100 cells/mm3
|
|
|
Is CNS toxoplasmosis a primary infection or is it a reactivation?
|
CNS toxoplasmosis results from reactivation of the previously acquired infection
|
|
|
What does CNS toxo look like?
|
-Multiple enhancing mass lesions with surrounding vasogenic edema.
-The lesions are usually relatively small—between 1 and 4 cm in diameter. -Larger lesions usually exhibit ring enhancement, while smaller lesions are usually solid. -The lesions are usually of increased signal on precontrast T2WIs. -Unlike bacterial abscesses, toxoplasmosis lesions are not high in signal on DWI. -The basal ganglia are a favored site, but white matter and cortical lesions are also common. |
|
|
Main differential for something that looks like CNS toxo?
|
-The main differential consideration is primary CNS lymphoma
-A clinical and imaging response to antitoxoplasmosis antibiotics will usually distinguish between toxoplasmosis and lymphoma in most cases -Biopsy is usually reserved for atypical cases or when there is no response to antibiotics. -Other infections or tumors may occasionally mimic toxoplasmosis but are unusual. |
|
|
Most common fungal CNS infection in HIV pts?
|
Cryptococcosis is the most common fungal infection.
|
|
|
Imaging findings in meningitis in an HIV pt?
|
-Meningitis is usually mild because of the diminished inflammatory response of the immunocompromised host.
-Therefore, there is usually little or no enhancement of the meninges, and imaging studies are usually normal. |
|
|
What do cryptococcomas look like?
|
-Cryptococcosis may sometimes present as dilated Virchow-Robin spaces filled with cryptococcus organisms, known as gelatinous pseudocysts.
-These cysts appear as rounded, smoothly marginated lesions in the basal ganglia that are nearly isodense and isointense to CSF. -There is no enhancement following contrast administration, which distinguishes these lesions from toxoplasmosis. |
|
|
How can you tell a cryptococcoma from toxo?
|
Cryptococcomas don't enhance
|
|
|
Name the virus associated with PML. Is PML a primary infection or a reactivation?
|
Progressive multifocal leukoencephalopathy is an infection of immunosuppressed patients caused by reactivation of a papova virus (the JC virus).
|
|
|
Where are lesions of PML usually found?
|
In non-AIDS immunosuppressed patients, PML has a predilection for the occipital lobes, but in AIDS patients, any part of the brain may be involved.
|
|
|
What does PML look like?
|
-MR reveals focal lesions of increased signal on FLAIR and T2W images and decreased signal on T1WIs within the subcortical and deep white matter.
-CT shows white matter lesions of decreased density. -The lesions may be solitary or multifocal. -Mass effect and contrast enhancement are almost always absent, which are important distinguishing features. |
|
|
What are you often trying to distinguish PML from? What helps you?
|
-The main differential diagnosis in the setting of AIDS is that of HIV encephalitis.
-Unlike PML, HIV encephalitis is usually more diffuse and less intense on T2WIs, and does not extend to the gray–white junction. |
|
|
What does CMV encephalitis look like?
|
-There are many cases of pathologically proven CMV brain infection with normal CT and MR scans.
-CMV meningoencephalitis is occasionally imaged as areas of increased signal on T2WIs in the periventricular white matter. -Subependymal contrast enhancement, if present, is a valuable diagnostic sign. -Rarely, CMV will present as a ring-enhancing mass. |
|
|
What do CNS tuberculous infections in HIV pts look like?
|
-Most patients present with meningitis.
-Imaging studies in these patients reveal communicating hydrocephalus and/or meningeal enhancement. -Tuberculomas occur in about 25% of patients with HIV-related CNS tuberculosis, but tuberculous abscesses are less common. -Tuberculomas are usually smaller and have less edema than tuberculous abscesses. |
|
|
What does primary CNS lymphoma look like?
|
-Solitary or multiple enhancing mass lesions are found with neuroimaging studies.
-The lesions are usually centrally located within the deep white matter or basal ganglia, but cortical lesions also occur. -There may be subependymal spread or extension across the corpus callosum, which do not usually occur with toxoplasmosis. -With MR imaging, there is variable signal intensity, with areas of low or high signal on T2WIs and isosignal or low signal on T1WIs. -With CT, the lesions are often isodense with gray matter. -The lesions almost always enhance with contrast in either a ring or solid pattern. |
|
|
How do you tell toxoplasmosis apart from primary CNS lymphoma?
|
-The imaging appearance is often indistinguishable
-The main distinguishing features are size and number. -Toxoplasmosis is more frequently multiple, and the lesions are usually smaller than with lymphoma. -Isointensity with white matter on T2WIs and diffuse, homogeneous contrast enhancement favor lymphoma. -High signal on T2WIs (often with a low signal rim) and ring enhancement following contrast administration favor toxoplasmosis. -MR spectroscopy shows increased choline and decreased NAA with lymphoma, while toxoplasmosis shows decreased choline and NAA with increased lipid and lactate. -Toxoplasmosis is also more common than lymphoma and responds to antibiotic therapy. |
|

|
1
|
|

|
2
|
|

|
3
|
|

|
4
|
|

|
5
|
|

|
6
|
|

|
7
|
|

|
8
|
|
|
9
|
|

|
10
|
|

|
11
|
|

|
12
|
|

|
13
|
|

|
14
|
|

|
15
|
|

|
16
|
|

|
17
|
|

|
18
|
|

|
19
|
|

|
20
|
|

|
21
|
|

|
22
|
|

|
23
|
|

|
24
|
|

|
25
|
|

|
26
|
|

|
27
|
|

|
28
|
|

|
29
|
|
|
30
|
|

|
31
|
|

|
32
|
|

|
33
|
|

|
34
|
|

|
35
|
|
|
What infections should you think of if there is evidence of an infarct?
|
-Aspergillus (especially if it's a hemorrhagic infarct)
-TB (especially if caudal basal ganglia) -Syphilis (especially if there's focal menigneal enhancement) -HIV |
|
|
What infections should you think of if you see calcifications?
|
-TB
-HIV (associated with atrophy, especially in peds pts) -Cysticercosis |
|
|
Differential for multiple ring enhancing lesions:
|
-Toxo
-Lymphoma -Fungus (candida, aspergillus) |
|
|
Which fungus is especially associated with hemorrhage?
|
Aspergillus
|
|
|
What should you think of if you see lesions without much associated mass effect?
|
-HIV encephalopathy
-CMV -PML |
|
|
What should you think of if you see disease in the bilateral inferior frontal lobes associated with sinus disease?
|
Mucormycosis
|
|
|
Basilar meningeal enhancement=
|
-TB
-Fungus (crypto, histo) |
|
|
Subependymal enhancement=
|
-CMV
-Lymphoma (nodular) |
|
|
Immunocompromised pt with multiple nodular enhancing lesions=
|
-Toxo
-TB -Fungus -Lymphoma (less likely) |

