![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
69 Cards in this Set
- Front
- Back
|
Function of respiratory system |
The exchange of gases between air & blood |
|
|
Respiratory system divisions |
Upper respiratory Lower respiratory Plueral membranes Respiratory muscles |
|
|
Upper respiratory tract |
*consists of parts OUTSIDE of the chest cavity: -air passages of the nose (enters) -nasal cavities (2) -pharynx (throat) -larynx (voice box) -upper trachea (wind pipe) |
|
|
Lower respiratory tract |
*consists of parts INSIDE chest cavity: -lower trachea -lungs -bronchial tubes -alveoli (air sacs for exchange of gas) |
|
|
Respiratory muscles |
-FORM the chest cavity -diaphragm -intercoastal muscles (in-between ribs) |
|
|
Plueral membranes |
PROTECTS the lungs -parietal pleura LINES the chest wall -visceral pleura COVERS the lungs BETWEEN the pleura membranes is serous fluid which prevents friction |
|
|
Upper nasal cavity |
contains olfactory receptors (sense of smell) which DETECT vaporized chemicals |
|
|
Nasal cavities (2) |
LOCATED in the skull
Air that is inhaled is WARMED (almost to body temp) as it goes towards the lungs
|
|
|
Nasal mucosa (lining) |
Is a ciliated epithelium tissue lining with goblet cells that produces mucus |
|
|
Cilia hair (nasal cavities) |
-Inside nostrils -Help block dust -Sweep out pathogens |
|
|
Nose |
-Composed of bone -area where AIR enters the body -nasal hairs trap pathogens |
|
|
Goblet cells |
Produce mucus that helps trap pathogens |
|
|
Paranasal Sinuses |
-air cavities in the skull -FUNCTION is to lighten skull -PROVIDES tone to your voice -LINED with ciliated epithelium tissue -mucus that is produced drains into nasal cavities. |
|
|
Nasal septum |
SEPARATES nasal cavities |
|
|
Pharynx (throat) |
-Muscular tube with 3 parts ***oropharynx (close to mouth) ***nasopharynx (close to nose) ***laryngopharynx (close to v-box) -POSTERIOR to nasal & oral cavities |
|
|
Nasopharynx (close to nose) |
Air ONLY passageway |
|
|
Oropharynx (close to mouth) |
food AND air passageway |
|
|
Laryngopharynx (close to voice box) |
food AND air passageway |
|
|
Larynx (voice box) |
-MADE of 9 pieces of cartilage to PREVENT collapse (firm yet flexible) (firm yet flexible) -FUNCTIONS: speaking and air passageway between pharynx & trachea |
|
|
Epiglottis (most superior cartilage of Larynx) |
CLOSES during swallowing like a trap door to PREVENT the entry of saliva or food into the Larynx |
|
|
Vocal cords |
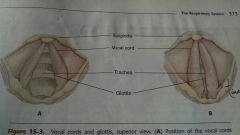
MOVE according to breathing or speaking |
|
|
Trachea (wind pipe) |
-Composed of cartilage -INFERIOR to larynx, SUPERIOR to bronchi -ciliated epithelium tissue -air passageway takes air to bronchia |
|
|
Bronchioles |
Smaller bronchial tubes extending from bronchial tree that have alveoli (air sacs) @ the ends
**no cartilage in the walls of bronchioles (important in asthma) |
|
|
Bronchial tree |

-the branching of the bronchial tubes -they are the PASSAGEWAY for air |
|
|
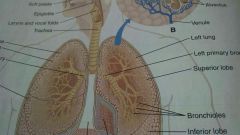
Lungs |

-LOCATED on either side of the heart in the chest cavity and encircled by the rib cage -Separated by the mediastinum -The base of each lung rests on diaphragm |
|
|
Hilus |
indentation on medial surface where the primary bronchus, pulmonary artery and veins enter the lung |
|
|
Aveolar cell types |
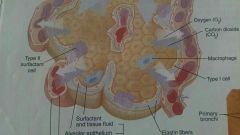
Type 1 cells that creates the aveolar walls are simple squamous epithelium (single, thin to allow for exchange of gases)
Type 2 cells secrete a lipoprotein surfactant that mixes w/tissue fluid that helps decrease surface tension for exchange of gases |
|
|
Aveoli |
Also known as AIR SACS @ the ends of the bronchioles |
|
|
LUNGS divided into sections |

Left side of lung sections: Superior lobe Inferior lobe Cardiac notch (Sit In Chair Little Friend)
Right side of lung sections: Superior lobe Middle lobe Inferior lobe
|
|
|
Elastin fibers |
flexible for exchange of gases |
|
|
Mechanisms of breathing |
Ventilation (inhalation/exhalation) Muscular (plays a role) Endocrine (influences) Circulatory (plays a role) |
|
|
Ventilation |
The term for the movement of air to and from the aveoli |
|
|
Muscle used in breathing |
Diaphragm- contracts, flattens & moves downward External intercostal- pulls ribs upward and outward Internal intercostal- pulls ribs downward and inward |
|
|
Pressures related to breathing |
Atmospheric pressure- pressure of the air around us Intrapleural pressure- pressure between parietal & visceral pleura (always slightly below atmospheric pressure, aka negative pressure Intrapulmonic pressure- pressure within the bronchial tree & alveoli (fluctuates below and above atmospheric pressure during each cycle of breathing |
|
|
Inhalation (aka inspiration) |
Motor impulses from the medulla travel on the phrenic nerves to the diaphragm & intercostal nerves to the external intercostal muscles
Diaphragm contracts and moves downward and expands the chest cavity from tip to bottom
(AT THE SAME TIME)
External intercostal muscles pull the ribs up and out which expands the chest cavity side-to-side and front-to-back
|
|
|
Exhalation ( aka expiration) |
Begins when motor impulses from the medulla decrease and the diaphragm & external intercostal muscles relax Diaphragm relaxes & rib cage falls down (AT THE SAME TIME) External intercostal muscles relax, chest cavity size decreases, lungs compress, alveoli compress, air is squeezed out of lungs |
|
|
Inhalation vs Exhalation process |
Inhalation= Active process; requires muscle contraction Exhalation= Passive process; depends on elasticity of healthy lungs |
|
|
Pulmonary volumes |
Variations in lung capacity varies with size and age of the person |
|
|
Tidal volume |
The amount of air in normal inhalation & exhalation |
|
|
Minute respiratory volume (MRV) |
Amount of air inhaled/exhaled in one minute |
|
|
Inspiratory reserve |
Deepest inhale as possible |
|
|
Expiratory reserve |
Deepest exhale as possible |
|
|
Vital capacity |
Deepest inhale & exhale Singers, athletes, emphysemia |
|
|
Residual air |
The amount of air left AFTER deepest exhale |
|
|
Spirometers |
used to measure exhalation |
|
|
Gases exchanged (external & internal) |
Oxygen and carbon dioxide are exchanged in two sites: the lungs and the tissue of the body |
|
|
Eternal respiration |
Movement of gases between air in alveoli and blood in the pulmonary capillaries AND air from external environment |
|
|
Internal respiration |
Movement of gases between blood in the systemic (everywhere but lungs) capillaries AND to cells in tissue fluid |
|
|
Diffusion |
HIGHER concentration to LOWER concentration |
|
|
Partial pressure (P) |
the concentration of two gases in a particular part of the body (CO2 & O2) Measured the same as blood pressure mmHg |
|
|
Transport of gases in blood |
Oxygen is carried on RBC's, they need hemoglobin (protein) and iron
-WEAK bond because oxygen is being carried to the cells (for cell respiration)
Carbon dioxide- some is dissolved in plasma and some is carried on hemoglobin, most are changed into bicarbonate ions and carried in the plasma, then changed back into CO2 when the blood reaches the lungs to be exhaled |
|
|
Regulation of respiration |
Two types of mechanisms regulate breathing - nervous mechanisms - chemical mechanisms |
|
|
Respiratory centers |
Medulla contains respiratory center which is comprised of - inspiration center (inhalation) - expiration center (exhalation) ** antagonistic relationship- CANNOT INHALE & EXHALE @ THE SAME TIME |
|
|
Inspiration center |
- generates impulse - respiratory muscle - contraction (inhalation) - baroreceptors in lungs - detect stretching - sensory impulses - medulla |
|
|
Hearing Breuer inflation reflex |
PREVENTS over inflation of lungs |
|
|
Pons (normal breathing) |
Helps to inhale properly or longer APNEUSTIC CENTER- allows us to prolong inhalation. PNEUMOTAXIC CENTER- interrupts inhalation AND contributes to exhalation SUPERIOR to medulla |
|
|
Hypothalamus |
Changes our respiration rate to accommodate our needs |
|
|
Cerebral cortex |
can play a role in changing breathing rate |
|
|
Breathing control |
ONLY the MEDULLA controls breathing PONS have temporary control over breathing |
|
|
Respiratory reflexes |
respiratory reflexes CONTROLLED by the medulla: coughing- uncontrollable is reflex sneezing- irritants in nasal cavity yawning- cool brain, etc hiccups- spasms of the diaphragm |
|
|
Chemical regulation |
IMPACT on BREATHING from blood pH, blood levels of oxygen & carbon dioxide |
|
|
Chemoreceptors |
DETECT changes in blood gases and pH and LOCATED in carotid & aortic bodies AND in the MEDULLA |
|
|
Hypoxemia |
decrease of oxygen is DETECTED by chemoreceptors in carotid & aortic bodies. GENERATES sensory impulses on glossopharageal & vagus nerves sent to medulla to INCREASE respiratory rate to speed inhalation to raise oxygen levels. |
|
|
Excess carbon dioxide |
Excessive amounts of CO2 in blood can disrupt pH balance (lowers pH) making blood MORE acidic |
|
|
Greater regulator of respiration |
Carbon dioxide is the greater regulator of respiration. Too much CO2 causes pH levels to drop. |
|
|
Respiratory acidosis |
Too acidic (LOW pH)
1-6 level = acidosis
|
|
|
Respiratory alkalosis |
too alkaline (HIGH pH)
8-14 level = alkalosis |
|
|
Respiratory compensation |
a LOW pH or HIGH pH OTHER than respiratory system reasons DISEASES can cause the pH to be HIGH or LOW. * Metabolic acidosis * Metabolic alkalosis |
|
|
Aging & the respiratory system |
-Muscles weaken - cause pH levels to LOWER - aging causes LOWER O2 which causes cell respiration issues - macrophages weaken so there is more pathogens |

