![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
Compare innate and adaptive responses to allergens |
Innate: recognize and clear standard antigens (mast cells, macrophages, dendritic cells, natural killer cells, compliment cytokines) Adaptive: B and T cells mediated - has immune memory and amplifies cytokine response —> highly specific T Cells mature in thymus —> CD4/8 helper cells B Cells mature in lymphoid organs (BM, fetal liver) Both have memory Able to discern self from non-self |
|
|
Provide the clinical criteria for anaphylaxis |
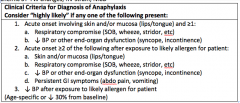
1. antigen + hypotension 2. MM/Skin + one of: SOB, hypotension 3. 2 of: MM/Skin, Hypotension, SOB, N/V/D |
|
|
OLD What are the 4 Coombs and Gel hypersensitivity reactions (give an example of each) |
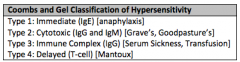
1 : antigen recognised by IgE or IgG cells 2: cell bound antigen activates compliment system - Rh, graves, goodpastures, transfusion reaction (ABO), 3: immune complex floating around —> depositis in tissues i.e. GN, Serum Sickness, HSP,RA 4: Deayed rx - contact dermaitits, Td - PPD, EM, SJS, Tens, - antigen antibody اللي تحت هو الصح |
|
|
Describe the anaphylactic process |
IgE is released by plasma cells and responds to novel antigen, causing sensitization. Re-exposure to the antigen leads to mast cell degranulation with up-regulated receptorMediators: histamine, tryptase, chymase, carboxypeptide A —> capillary permeability, vasodilation, smooth muscle contraction, myocardial depression |
|
|
Name 8 Sx of anaphylaxis? 5 ECG changes? |
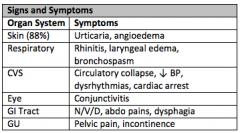
ECG Changes:
|
|
|
Provide 10 DDx of anaphylaxis |
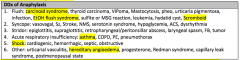
|
|
|
What are the 3 indications for IV epinephrine in anaphylaxis? Indication for glucagon? |
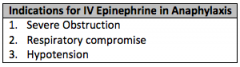
Glucagon if patient on BB (1mg bolus then 1-5mg/hr) |
|
|
Name 10 ways to reduce the mortality risk of anaphylaxis in patients in the ED |
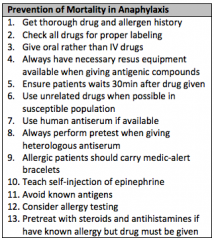
|
|
|
What is angioedema? Tx? Quincke's Disease? |
Edema of deeper dermal and subcutaneous tissues without pruritis Quincke's = angioedema of the uvula Tx: as per anaphylaxis |
|
|
OLD Name 10 causes of serum sickness Pathophysiology? |
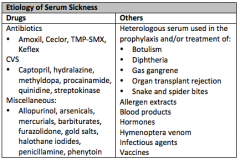
Type III reaction, immune-complex deposition 4-10d after exposure: generalized lymphadeopathy with urticaria, joint pains, fever Tx: stop agent, antihistamines, possible steroids ABX: Amoxil, Septra Anti-sz: Dilantin Antivenoms Hymenoptera Transfusion |
|
|
How does radiocontrast dye cause a hypersensitivity reaction? Risk Factors for contrast allergy? Prevention? |
Direct mast-cell degranulation, not IgE mediated RF: Previous reaction Atopy/asthma/allergic dz Prevetion of Contrast Reaction (per UPTODATE) NO TEST DOSING - this is not recomended CHECK if different contrast material can be used Accepted regimen if you have time:
In An Emergency:
|
|
|
Reasons to admit anaphylaxis? |
|
|
|
OLD What are possible causes of angioedema? Treatment? Mechanism of ACE-I angioedema? |
Causes: ACEi Anaphylaxis/anaphylactiod Hereditary (C1 esterase inhibitor deficency) Standard treatment: same tx as anaphylaxis (avoid this tx if hereditary) If hereditary: Ruconest (recombinant C1-esterase inhibitor), FFP ACEI angioedema in 0.1-0.2% 2° to inhibited metabolism of bradykinin and substance Pusually in the 1st month but can occur 10 years latertx supportive ? can try FFP |
|
|
Define Anaphylactoid Reaction |
Clinically similar to anaphylaxis but not IgE mediated mediated by direct mast cell and basophil degranulation do not require prior sentisitazation so can occur at single exposure |
|
|
Anaphylaxis Risk Factors |
high SES summer/early fall female > 30 adults IV/topical antigen > risk than oral Atopy = increased risk for mucosal route of reactioncauses: Food, drug, insect stings, latex = majority of causes |
|
|
Treatmet of Anaphylaxis |
Remove stingers benadryl 50 mg IV/PO epinephrine sc 0.3-0.5 (kids 0.01mg/kg) IM or epi IV 1-10mcg/min IVP/minute (1ml of 1:10000 in 9cc NS or 0.1ml of 1:1000 in 9cc NS = 10 mcg/ml)dirty epi drip 1mg in 1000NS = 1mcg/ml (can pull push doses from the bag or run an infusion) Ventolin/Atrovent for bronchospasm Neb Epi 5ml of 1:1000 in NS (peds 0.5ml/kg max 5ml) Steroids Methyl pred 125mg IV (Pred po) Epi refractory —> norepi Glucagon if poor response to epi or on beta blockade |
|
|
Biphasic Reactions = # patients? |
Can occur up to 3 days post rx # clinically important biphasic reactions < 1% Risk Factors
UP TO DATE: no consensus on duration of observation (2016)those with the above risk factors should be observed for 12 hoursotherwise min. 2 hours some guidelines recomend 4-6 hours (world allergy organisation) |
|
|
What is Mastocytosis? S/S? Dx? Tx? |
Disorders of too many mast cellscutaneous sxs: urticaria pigmentosa systemic: mast cell hyperplasia in BM, gut liver and spleen (pathologic #, AP, diarrhea, headache, flushing) Dx
Tx:
|
|
|
OLD Risk Factors for increased severity of anaphylaxis 6 |
* List from UTD |
|
|
DDx for rash and joint pain |
|
|
|
NSAID Anaphylaxis Mechanism |
Inhibition Cox - inhibits thromboxane production increased leukotriine production |
|
|
Epi MOA |
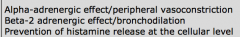
|

