![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is a Newtonian Fluid? |
Def 1. Homogeneous fluid with a viscosity that does not change with flow rate. Def 2. Shear rate and shear stress of the fluid are proportional. This is true for water but not for blood. |
|
|
|
What is the viscosity of water |
0.01 poise or 1 centipoise at 20 °C. 0,695 at 37°C. 1.8 at 0° |
|
|
|
Plasma Viscosity |
1.2 at 37°C. Relative viscosity of 1.7 |
|
|
|
Blood viscosity? |
Blood has a relative viscosity of 4 to 5 when measured at moderate or high shear rates, but the viscosity is much higher at low shear rates. |
|
|
|
Hydraulic Resistance? |
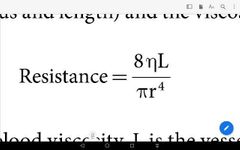
|
|
|
|
Units of resistance |
Resistance = Pressure / Flow =mmHg/ml/min =Pressure drop/Cardiac Output = Mean Aortic P - right atrial pressure = 100/5000 =0.02mmHg/ml/min To convert to Wood units multiply by 1000. The absolute resistance units may be converted to Wood units by dividing by 80. For example, the normal SVR is 700–1600 dyne·s/cm5, or 9–20 Wood units.). |
|
|
|
Poiselle vs CVS. |
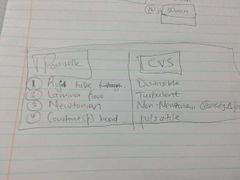
|
|
|
|
Pressure - Flow relationships of different blood vessels Draw the graph |
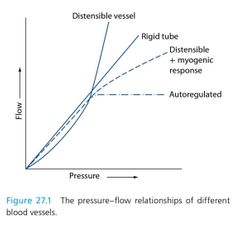
|
|
|
|
What is shear thinning? |
The apparent viscosity of blood decreases as the shear rate is increased – an effect known as shear thinning |
|
|
|
List Factors that affect Anomalous Viscosity of Blood |
1. Hematocrite: direct relationship 2. Temperature: inverse relationship 3. Flow rate: inverse relationship 4: Vessel diameter : direct relationship. |
|
|
|
What are the units of Viscosity |
The unit of viscosity is the poise (equal to 1 dyne·s/cm2). At 20°C, the viscosity of water is 0.01 poise, or 1 centipoise. |
|
|
|
Types of Capillaries & location (6) |

|
|
|
|
Alternatives for Trans endothelial transport |
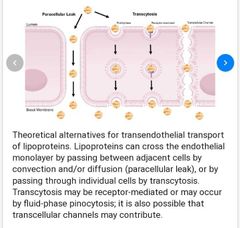
|
|
|
|
Define Wall tension incl formula (4) |
The wall tension is the force per unit length tangential to the vessel wall that opposes a distending force that tends to pull apart a theoretical split in the wall (i.e. prevents vessel rupture). *and is related to the distending force (the product of transmural pressure and radius), by the law of Laplace: Wall tension = Pressure × Radius |
|
|
|
Two main functions of Capillaries |
(i) delivery and removal of nutrients and metabolites to tissues by diffusion across the capillary wall and (ii) distribution of fluid between the intravascular and extravascular compartments by bulk flow of fluid and solutes across the semipermeable capillary wall (impermeable to large protein molecules). |
|
|
|
Name the four Starling Forces involved in the filtration process (4) Use a diagram. |
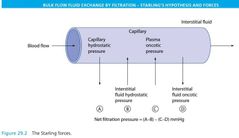
capillary hydrostatic pressure, interstitial hydrostatic pressure, plasma oncotic pressure and interstitial fluid oncotic pressure |
|
|
|
Define & describe net filtration pressure. (4) Write the formula & normal values (4) |
The NFP – the resultant pressure of the four Starling forces – can be calculated at the arterial and venous ends of a capillary as follows: NFP = (Pc −Pif ) − (πp −πif ) where Pc is the capillary hydrostatic pressure, Pc at the arterial end of the capillary = 35 mmHg, Pc at the venous end of the capillary = 15 mmHg; Pif is the interstitial fluid hydrostatic pressure = 0 mmHg; πp is the plasma oncotic pressure = 28 mmHg; πif is the interstitial fluid oncotic pressure = 3 mmHg; NFP at arterial end of the capillary = 10 mmHg and NFP at venous end of the capillary = −10 mmHg. Bulk flow across the capillary wall = k × NFP, where k is the capillary membrane filtration constant. |
|
|
|
What is the net fluid loss from capillary filtration per day |
The net fluid loss from filtration in the capillaries is only 4 L/day, and this is reabsorbed by the lymphatics. |
|
|
|
What the factors determining Capillary Hydrostatic Pressure? |
The ratio of precapillary & post capillary resistances CHP = Post capillary resistance / Precapillary Resistance |
|
|
|
Functions of the endothelium (3) |
nutrient and waste product diffusion fluid filtration endothelial cells produce vasoactive substances |
|
|
|
What vasoactive substances are produced by the Endothelium? Mention their stimulation and Effect (12) |
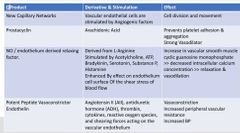
|
|
|
|
List the 6 Functions of the Endothelial Glycocalyx |
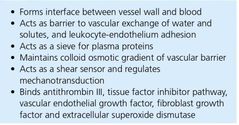
|
|
|
|
What is the endothelial Glycocalyx (4) |
1. In 2010, Levick and Michel proposed that the endothelial glycocalyx layer is the small pore system of the transvascular semipermeable membrane of the endothelium 2. Layer of Glycoprotiens & Glycosaminoglycans (mucopolysacharrides) bound to the lumina surface of the Endothelial Cells to form the interface between blood and capillary wall. |
|
|
|
What causes loss of the Endothelial Glycocalyx Layer (4) |
Hypervolaemia (^ANP) Diabetes Hyperglycaemia Inflammatory mediators: surgery & Sepsis: Namely = CRP, TNF, Bradykinin, Mast Cell Tryptase |
|
|
|
What restores and protects the glycocalyx layer (4) |
Antithrombin III Hydrocortisone N-Acetylcysteine Sevoflurane |
Break down the clot Anti-inflammation Detoxify Anaesthesia. |
|
|
Which tissues do NOT contain lymph Vessels |
Central Nervous System Bone Cartilage Epithelium |
|
|
|
Rate of lymph flow |
120 mL/hr or 2–3 L/ day. |
|
|
|
Compare the protein conc of lymph in interstial fluid, liver & intestine (3) |
Interstial Fluid: 2g/dL Intestine 3-4g/dL Liver 6g/dL |
|
|
|
What are the determinants of the rate of venous return to the heart (6) |
The factors that determine the rate of venous blood flow back to the heart are as follows: • The pressure gradient for venous return • Venous valves • The skeletal muscle pump • The respiratory pump • The effect of ventricular contraction and relaxation • Venomotor tone |
3pumps |
|
|
Draw the configurational changes in veins on a volume / pressure graph. (6) |
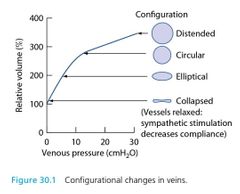
|
|
|
|
What is the Mean Systemic Filling Pressure? What does it indicate? |
mean systemic filling pressure (MSFP) – the average of all the pressures in different vessels weighted according to their relative compliances. This is a single hydrostatic assessment of the filling of the cardiovascular system and indicates the pressure moving blood back towards the right atrium to maintain the cardiac output. |
|
|
|
Define the venous pressure gradient (formula) |
T he pressure gradient through the veins to the right atrium is the main factor determining the rate of venous return and is equal to the difference between the MSFP (7 mmHg) and the mean right atrial pressure (1 mmHg): T he pressure gradient for venous return = MSFP – Mean right atrial pressure = 6 mmHg |
|
|
|
What increases and decreases MSFP? |
The MFSP increases with venomotor tone or blood volume and falls with venodilation or blood loss. Changes in total peripheral resistance do not affect the MFSP. |
|
|
|
Graphically demonstrate the effect of sympathetic Outflow on the cardiac output curve. 6 |
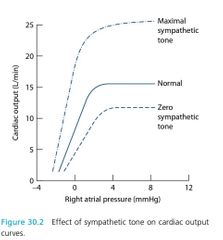
|
|
|
|
Define venous return (equation) |
Venous return is proportional to the difference between MSFP and right atrial pressure, which is the hydrostatic pressure gradient promoting venous return. In this range of right atrial pressure (i.e. 0–7 mmHg), venous return can be defined by the following equation: Venus return = (MSFP - RAP) / Resistance to venous return The ‘resistance to venous return’ is a term that reflects the resistance and capacitance of the venous circulation. |
|
|
|
Draw the normal venous return curve |
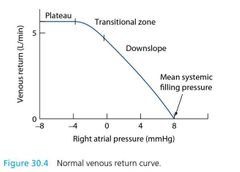
|
|
|
|
Right heart bypass preparation; |

|
|
|
|
Draw a graph showing the effect of MSFP on the Venous Return Curve. |

|
Note: A 15% increase in blood volume will double the MSFP, whereas a 15% decrease will reduce it to zero. |
|
|
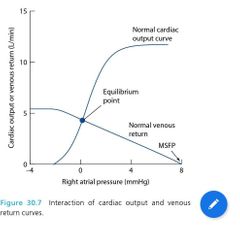
What is the equilibrium point? |
The point of intersection of cardiac output and venous return curves is known as the equilibrium point It intersects @ CO of 5l & RAP of zero |
|
|
|
Graph showing effects of changes in Resistance to Venous Return |
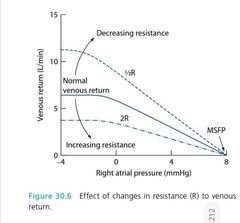
|
|
|
|
Effect of Sympathetic Activity on the Equilibrium Point |
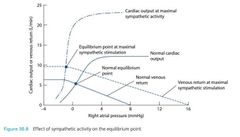
|
|
|
|
How much, & at what pressure, is blood in the arteries? |
The arteries (with the arterioles) contain approximately 15% of the total blood volume (i.e. 750 mL) at a mean pressure of around 100 mmHg. |
|
|
|
Define Arterial pressure. |
Arterial pressure is the force exerted per unit area of the arterial wall. |
|
|
|
What is Mean arterial pressure? How can MAP be measured |
The mean arterial pressure, is the average arterial pressure acting during the cardiac cycle, is the driving force for blood flow and it can be measured by averaging the pressure recorded under an arterial pressure curve over time |
|
|
|
What is arterial pressure? |
Arterial pressure is the force exerted per unit area of the arterial wall. |
|
|
|
What increases systolic blood pressure? |
Systolic blood pressure increases when there is (i) an increase in stroke volume; (ii) an increase in ejection velocity (without a change in stroke volume); (iii) a decrease in aortic or arterial distensibility; and (iv) an increase in diastolic pressure of the previous pulse |
|
|
|
What increases diastolic blood pressure |
a decrease in ejection velocity; (ii) an increase in aortic or arterial distensibility; and (iii) an increase in total peripheral resistance |
|
|
|
What is arterial pulse pressure? Formula? |
Arterial pulse pressure is the difference between systolic and diastolic pressures: Pulse pressure = Systolic pressure − Diastolic pressure |
|
|
|
MAP formulas (2) |
Mean arterial pressure = Diastolic + 1/3 (Systolic − Diastolic)
Or
Mean arterial pressure = Peripheral run off × Total peripheral resistance |
|
|
|
Resistance formula |
Resistance = Pressure/ Flow |
|
|
|
How does a fall in compliance affect the pulse pressure? |
A fall in arterial compliance increases the pulse pressure for two reasons: (i) the ventricular ejection of blood into the stiff arteries produces a greater increase in systolic pressure and (ii) the hydraulic filter (Windkessel), which normally maintains diastolic pressure, is impaired by the reduced arterial elasticity |
|
|
|
How does arteriolar constriction and dilation affect arterial pressure and capillary pressures? |
Arteriolar dilation tends to reduce the hydrostatic pressure drop across these vessels: arterial pressure decreases, and capillary pressure increases. Arteriolar constriction tends to increase the hydrostatic pressure drop: arterial pressure increases, and capillary pressure decreases. |
|
|
|
What are the arteriolar functions? (3) |
Alter total peripheral resistance. • Alter the vascular resistances of individual organs. • Alter capillary hydrostatic pressure. |
|
|
|
In Which organ is myogenic conrol more important? |
myogenic activity is dominant in the brain and the kidneys and is the mechanism of the autoregulation of blood flow seen in those organs over a wide range of mean arterial blood pressures. |
|
|
|
Diagrammatic representation of the mechanisms by which the cardiovascular system is controlled. |

|
|
|
|
The sympathetic and parasympathetic nerves in the brain and spinal cord involved in cardiovascular control. |

|
|
|
|
Draw the Haemorrhage: effects on venous return and cardiac output curves. |
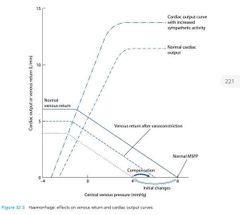
|
|
|
|
Endocrine response to Haemorrhage Flow Chart |
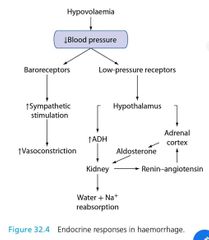
|
|
|
|
What is the use of a valsalva maneuver? |
The Valsalva manoeuvre may be used clinically to assess autonomic function and also to slow supraventricular tachycardia. The autonomic function can be assessed by determining the Valsalva ratio. |
|
|
|
What is the Valsalva Ratio? And what is the normal value? |
The Valsalva ratio is equal to the minimum heart rate (longest R–R interval) in phase IV divided by the maximum heart rate (shortest R–R interval) in phase IV. The Valsalva ratio is normally greater than 1.5, but in patients with impaired autonomic function, it is less than 1.5 |
|
|
|
Valsalva Maneuver in autonomic dysfunction? |
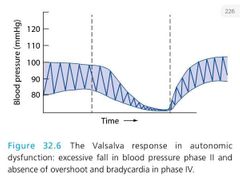
|
|
|
|
The Valsalva manoeuvre in Congestive Heart Failure |
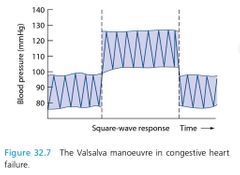
|
|
|
|
What are the 3 factors determining exercise tolerance? |
Cardiovascular performance incl peripheral vasculature Pulmonary gas exchange Skeletal muscle metabolism Pulmonary gas exchange Skeletal muscle metabolism |
|
|
|
What determines the capacity for Peak Exercise Performance |
The capacity for peak exercise performance therefore depends on the maximum ability of the cardiovascular system to deliver O2 to the skeletal muscles and of the exercising muscles to extract O2 from blood |
|
|
|
What is the formula for oxygen uptake? |
Ficks equation Oxygen uptake = (Cardiac output) X (content of arterial oxygen - content of mixed venous oxygen) = (SV x HR) X (CaO2 - CvO2) |
|
|
|
How does the cardiovascular system respond to exercise (4) |
1. Increased Cardiac output up to six times: this facilitates oxygen uptake. 2. Redistribution of cardiac output from non-active (splanchnic & Renal) tissues to skeletal muscles : enhances oxygen delivery 3. Greater O2 extraction >> widened ateriovenous oxygen difference. 4. Increased pulmonary blood flow (by increase in CO & vasodilation) |
|
|
|
What is maximal oxygen capacity? |
At maximal exercise, the maximal ability of a person to take in, transport and use oxygen (functional aerobic capacity) is called maximal oxygen capacity ( VO2max) |
|
|
|
Equation for VO2max? |
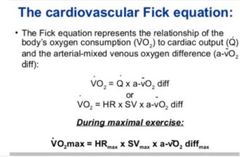
|
|
|
|
Diagrammatic representation of the negative feedback arterial baroreceptor reflex. |

|
|
|
|
Diagram: Cardiovascular Changes During Hemorrhage |

|
|
|
|
What is the mechanism for training induced improvements in VO2max? |
*The primary mechanism for training-induced improvements in VO2 max is an increase in cardiac output secondary to an increased stroke volume in response to exercise. *Peaked heart rate is generally not affected by training. |
|
|
|
What is the Bain Bridge Reflex. |
When there is stimulation of the Vagal VenoAtrial Stretch Receptors it results in; 1. Increase in HR - Selective sympathetic activity to the SA node. 2. Increase in Urine Volume 3. Increase in Salt excretion 2&3 are due to: A. Renal sympathetic activity B. Inhibition of ADH secretion C. Increase in ANP production |
|
|
|
What is the function of the Vagal Myelinated VenoAtrial Stretch Receptors? |
It functions to regulate cardiac size when venous pressure is high and to adjust blood volume. |
|
|
|
Where are the Unmyelinated Vagal and sympathetic cardiac mechanoreceptors? |
Form a fine network in Atria and mainly left ventricle |
|
|
|
Where are the Myelinated Vagal mechanoreceptors found? |
Around the coronary arteries |
|
|
|
Difference between Ventricular vs Atrial Unmyelinated Vagal & Sympathetic Mechanoreceptors. |
Atrial: fire during height of atrial filling during Inspiration. Ventricular : Fire during contraction |
|

