![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
194 Cards in this Set
- Front
- Back
|
Define Monkenberg medical calcific sclerosis.
What is the common co-morbid condition? Does it cause lumenal stenosis? |
Dystrophic calcification of media lamina of muscular arteries
diabetes mellitus No lumenal stenosis |
|
|
What cells are involved in forming an atheroma? (3)
|
monocytes, macrophages, and helper T cells
|
|
|
Name 5 arteries most commonly associated with atheroslcerosis in descending order.
|
1. abdominal aorta
2. CAD 3. popliteal arteries 4. internal carotid arteries 5. circles of willis |
|
|
What is the most feared complication of atherosclerotic lesion?
|
ruptured thrombosis that can thrombose over.
|
|
|
What are 3 types of lesions that develop in arteries in atherosclerosis?
|
1. fatty streak
2. fibrous plaque (atheroma) 3. complicated lesion (raised, lipid center, dangerous) |
|
|
Which anatomic portion of vessels is commonly affected by atherosclerosis? why?
|
Areas of turbulent flow (e.g. branch points)
turbulence leads to endothelial injury --> inflammation |
|
|
what are major components of a plaque? (2)
|
1. fibrous cap
2. lipid core |
|
|
Which 2 mobidities are associated with hyaline arteriolosclerosis?
|
Hypertension and diabetes
|
|
|
what is the pathogenesis of hyaline arteriolosclerosis?
|
deposition of protein in the vessel wall and occlude the lumen
|
|
|
What type of arteriosclerosis is associated with malignant hypertension?
what is the pathogenesis? Which arteries are frequently affected? |
Hyperplastic arteriolosclerosis
vascular wall thickening caused by deposition of SMCs and basement membranes. Kidney vessels are frequently affected |
|
|
Differentiate b/t benign HTN and malignant HTN.
|
Benign HTN: Systolic < 200mmHg and diastolic < 120 mmHg
Malignant HTN: systolic >200mmHg and diastolic > 120 mmHg |
|
|
Onion skin lesion and fibrinoid necrosis is associated with what type of arteriosclerosis?
|
Hyperplastic arteriolosclerosis
|
|
|
The following lesions are observed in what organ? Describe them.
1. arteriovenous nicking 2. copper-wiring 3. Silver-wiring |
Observed in hypertensive retinopathy (retinal arteriolosclerosis)
the following are observed in ophthalmoscopy: 1. arteriovenous nicking: inapparent veins due to thickening of the arteries 2. copper-wiring: tranlucnecy of the artery due to thickening 3. Silver-wiring: relfects the light due to massive thickening |
|
|
What are cytoid bodies and cotton-wool spots? Where are they observed?
|
They are observed in choroidal, retinal infarcts due to hypertensive retinopathy
Cotton-wool spots are pale areas on the retina due to colleciton of swollen axons (seen with opthalmoscope) Cytoid bodies are accumulation of mitochodria and damaged axons (seen under microscope) |
|
|
Classify vasculitis by the size of vessels each affects.
|
Large vessel vasculitis: Giant cell (temporal) arteritis and Takayasu arteritis ("pulseless") disease
Medium vessels vasculitis: Polyarteritis nodosa (PAN), Kawasaki disease, thromboangitis obliterans (Buerger disease) Small vessel disease: Wegener granulomatosis, Microscopic polyangiitis, Churg-Strauss syndrome, Drug-induced ANCA-associated vasculitis |
|
|
What is the most common systemic vasculitis seen in US adult population?
most commonly affected artery? |
Giant Cell arteritis
Temporal artery |
|
|
Granulomatous medial inflammation with giant cells, mural thickening, fragmentation of internal elastic lamina.
What vasculitis is it |
giant cell arteritis
|
|
|
A 60 YO Male presents with jaw claudication, sudden visual loss, and headache and throbbing pain in the temporal region.
what vasculitis is it? |
Giant cell arteritis
|
|
|
A 50 YO Asian female presents with weak radial pulse and pulmonary hypertension.
What vasculitis? |
Takayasu vasculitis
|
|
|
Which vasculitis is associated with smoking?
|
Thrombonagitis obliterans (Buerger disease)
|
|
|
A 60 YO male presents with fever, malaise, and weight loss. The lab shows increased serum creatinine and positive HBV antigens.
What vasculitis is it? Is this disorder associated ANCA? |
polyarteritis nodosa.
Not associated with ANCA |
|
|
A 13 YO male presents with palpable purpura, hemoptysis, hematuria and weakness.
The path lab indicates there is luekocytoclatosis near vessels, fibrinoid necrosis, but no granulomatosis. He is also p-ANCA positive. What vasculitis is most likely? |
Microscopic polyangiitis
|
|
|
What vasculitis disorders are associated p-ANCA? c-ANCA?
|
p-ANCA: microscopic polyangiitis and Churg-Strauss syndrome
c-ANCA: Wegener's granulomatosis |
|
|
A pt presents with asthma and palpable purpura. What vasculitis do you suspect?
|
allergic angiitis and granulomatosis (Churg-Strauss syndrome)
|
|
|
What 3 organs are involved in Wegener's granulomatosis?
What 3 lesions are involved in WG? |
3 organs ("ELK"): ENT, lung, kidneys
3 lesions: 1. respiratory acute necortizing granulomas 2. vascular necrotizing/granulomatous vasculitis 3. rapidly progressive glomerulonephritis |
|
|
What heart chamber is most anterior? most posterior?
Which structure lies behind the most posterior chamber of the heart? This allows for what imaging technique? |
Most anterior: Right ventricle
Most posterior: left atrium Allows for trans-esophageal echocardiography |
|
|
Name 2 papillary muscles in the left ventricle.
Which one is more prone to ischemia? why? |
Anterolateral pap muscle (dual blood supply from RCA and LCA)
Posteromedial pap muscle - more prone to ischemia and tearing due to a single blood supply (PDA) |
|
|
What is the clinical significance of left atrial appendage (auricle)?
|
more prone to thrombus formation
|
|
|
What regions of the heart and parts of the conduction system are supplied by the following arteries?
1. RCA 2. LAD 3. Left circumflex artery |
1. RCA: SA node, AV node, atria, and posterior and inferior aspects of LV, right bundle, posterior division of left bundle
2. LAD: 2/3 of ventricular septum, anterior LV and some inferior apex, His Bundle, anterior division of left bundle 3. circumflex: lateral aspect of LV |
|
|
what is fibromuscular dysplasia?
what is the most affected group? What is the most common complication? |
focal irregular thickening of walls of medium-sized and large muscular arteries.
Common in young women Renovascular hypertension due to low RPF, which activates the RAS system |
|
|
What is associated with rupture of berry aneurysm?
Name 3 most common site of berry aneurysm? |
Subarchnoid hemorrhage
1. anterior communicating artery 2. middle cerebral artery 3. jxn b/t MCA and posterior communicating artery |
|
|
What is fibromuscular dysplasia?
Which artery is most commonly affected? What complication can arise from this? Which population is it most common in? |
Fibromuscular dysplasia is a focal irregular thickening of walls of medium sized and large muscular artery.
Renal artery is most commonly affected --> activation RAS system --> hypertension Most common in young females |
|
|
How are true aneurysm and false aneurysm different grossly?
How is dissection different from the above two? |
true aneurysm: luminal dilation and bounded by all vascular wall componenets
false aneurysm: breach through the wall and forms extravascular hematoma dissection: a tear in the intima layer that causes blood to enter b/t the layers of the vessel. the blood dissects b/t the layers of wall. |
|
|
What is the most common etiology of aneurysm?
|
atherosclerosis
|
|
|
Describe the pathogenesis of aneurysm due to atherosclerosis.
|
Atherosclerotic intimal thickening --> inner intimal ischemia --> loss of smooth muscle cell --> Erdheim medial degeneration AND
inflammation --> increased matrix metalloproteinase production by macrophages --> ECM degradation both factors contribute to a decreased in wall strength --> luminal dilation |
|
|
What is Erheim medial degeneration?
|
cystic medial degeneration/necrosis due to atherosclerosis that results in weakened tunica media.
Can lead to aneurysmal dilatation. #1 risk factor is HTN. also can be due to Marfan's |
|
|
List most commons for aortic aneurysm.
1. most common population? 2. Most common location? 3. most common cause? |
1. >65 YO male smokers
2. distal to renal arteries at the iliac artery bifurcation 3. atherosclerosis |
|
|
List 4 complications associated with aortic aneurysm.
|
1. rupture (very fatal); critical diameter is 5cm
2. branch obstruction due to plaque 3. embolism 4. impingement on adjacent structures |
|
|
List 3 most common causes of ascending thoracic aortic aneurysm
|
1. Hypertension, which results in Erheim medial degeneraiton
2. atherosclerosis 3. syphilitic aortitis |
|
|
List 3 complications associated with thoracic aortic aneurysm
|
1. aortic ring dilation --> aortic insufficiency
2. encroachment/invasion of adjacent structure 3. rupture |
|
|
Where is the most common site of syphilitic aneurysm?
At what stage of syphilis does this occur? |
most common in ascending aorta.
tertiary stage; caused by Treponema pallidum |
|
|
What is obliterative endarteritis? How is this related to syphilitic aortic aneurysm?
|
Obiterative endarteritis is invasion of vaso vasorum by plasma cells.
This leads to ischemia of tunica media --> fibrosis and loss of elastic recoil --> weakened wall |
|
|
How does aortic valve get involved in tertiary syphilis?
|
May cause aortic valve ring dilation --> aortic regurgitation
symptoms include 1. end-diastolic murmur 2. decreased diastolic pressure --> increased pulse pressure |
|
|
What is the #1 risk factor of aortic dissection?
where is the most common site of aortic dissection? |
hypertension
ascending aorta within 10 cm of aortic valve. |
|
|
How is aortic dissection classified?
|
Debakey I: both ascending and descending portions are involved
Debakey II: only ascending portion is involved Debakey III: only descending portion is involved type A: involves ascending aorta type B: only involves descneding aorta. |
|
|
What are 2 connective tissue disorders associated with aortic aneurysm and aortic dissection?
|
Marfan's syndrome: defective fibrillin-1
Ehler-Danlos syndrome: defective type III collagen |
|
|
A 50 YO male presents with a sudden onset of anterior chest pain. He describes the pain as ripping or tearing and pain radiates toward the back. After 2 hours the pain extends to the abdomen.
What is the likely disorder? |
Aortic dissection
|
|
|
A pt presents with pink face, arm, and shoulder. He is clinically diagnosed with small cell lung carcinoma. What do you suspect?
|
superior vena cava syndrome: extrinsic compression of SVC
|
|
|
What is the most common venous lesion in adults?
Where is the most common site? |
varicose veins
superficial veins of lower extremities |
|
|
Name 3 complications associated with varicose veins.
|
1. cosmetic effects
2. impaired drainage --> stasis --> congestion, edema, pain, ischemia, decreased wound healing 3. rarely embolism |
|
|
Obstructive lymphedema is commonly associated after what procedure?
|
radiation damage following radical mastectomy
|
|
|
Name the disease.
Common in AIDS pts due to Bartonella henselae. Red papules and nodules grossly. |
Bacillary angiomatosis
|
|
|
What is vascular ectasias?
Name 3 types of vascular ectasias. |
dilation of pre-existing vessels
1. Nevus flammeus or Sturge-Weber disease ("port wine stain", "birthmark"): dilated dermal vessels; has trigeminal nerve distribution 2. Spider telangiectasia: associated with high estrogen 3. Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease): congenitally dilated capillaies on skin and mucous membranes; presents with mucosal bleeding (GI and epistaxis) |
|
|
What is the most common vascular tumor in adults?
|
hemangioma
|
|
|
What is the most common pediatric neoplasm?
|
hemangioma (mostly strawberry hemagioma)
|
|
|
A pt presents with painful, discolored mass on a distal digit under the fingernail. Histomorphology shows modified smooth muscles cells and branching vascular cells. What do you suspect?
|
glomus tumor
|
|
|
Which soft tissue tumor is associated with AIDS and HSV 8?
What is the morphology of this tumor? |
Kaposi sarcoma
slit-like vessels and spindle cells |
|
|
What vascular neoplasm is associated with viny chloride?
|
hepatic hemangiosarcoma (highly malignant)
also associated with arsenic and thorotrast |
|
|
What microbial agent is associated with acute lymphagitis?
What tumor is associated with chronic lymphedema? |
Strep pyogene causing cellulitis, which inflames the lymphatics
lymphangiosarcoma is associated with chronic lymphedema |
|
|
Name 2 malignant vascular neoplasms.
Which one has a better prognosis? which one is CD31 positive? |
Angiosarcoma: 30% 5 yr survival; CD31 positive
Hemangiopericytoma: 60-85% 5 yr survival: CD 31 negative |
|
|
What is the leading cause of death in US?
|
acute MI
|
|
|
What is the main cause of acute MI?
|
thrombotic primary plaque rupture --> complete occlusion
|
|
|
What type of clot can be treated with thrombolytics?
|
red clots: regular thrombus
white clots: platelet rich clots; can't be treated with thrombolytics |
|
|
The following symptoms indicate differential dx of chest pain. Identify each.
1. Typically reroducible with palpation or movement 2. hurts when breathing 3. hurts with coughing and will radiate to the trapezius region 4. internal tearing pain that extends to the back 5. burning sensation often exacerbated by eating |
1. chest wall pain
2. pleuritic pain 3. pericarditis 4. aortic dissection 5. esophageal/GI pain |
|
|
When do acute MI patients commonly present in a day? why?
|
typically early morning. This is when there is highest level of catecholamine (Circadian rhythm)
|
|
|
Describe 3 types of angina. what type of EKG findings do you expect with each angina?
|
1. Stable angina: chest pain with exertion; secondary to fixed, atheroscleortic CAD; ST depression on EKG
2. Prinzmetal variant angina: occurs at rest secondary to coronary artery spasm; ST elevation with stress test 3. Unstable angina: worsening chest pain at rest; often due to disrupted plaque; ST depression on ECG; may progress to acute MI |
|
|
What is Levine sign? When do you see this?
|
Seen with acute MI;
The sign is a distinctive look of someone having a acute MI; seen with clenched fist held over chest |
|
|
List 3 most common coronary arteries involved in acute MI.
|
LAD > RCA > circumflex artery
|
|
|
List the appropriate leads for the following part of the heart:
1. anterior leads 2. lateral leads 3. inferior leads |
1. anterior: V1-V5
2. lateral: V6, avL, I 3. inferior: II, III, avF |
|
|
How are non-STEMI different from STEMI?
What is the clinical importance of differentiating the two? |
non-STEMI: non-ST elevation MI; no path Q wave observed; associated with subendocardial infarction
STEMI: ST elevated MI; pathological Q wave can be observed; transmural MI; indicates the current injured myocardial cells STEMI indicates MI in progress. Permanent damage can be prevented with rapid catherization of the plaque. |
|
|
What does pathological Q wave represent?
|
It represents dead tissue seen in transmural infarction.
Q wave does not distinguish b/t newly dead tissue from old infarcts. |
|
|
How do you differentiate b/t acute transmural MI from old infarcts?
|
Old infarcts show pathological Q waves but no ST elevation
ongoing infarct shows pathological Q wave AND ST elevation |
|
|
What serum markers indicate acute MI?
Which one is most specific and sensitive? When does it appear and peak? |
Troponin: most specific and sensitive; appears 8 hrs after MI and peaks in 24 hr
CK-MB: rises 4 hrs after peaks in 24 hrs |
|
|
What is the most common complication of acute MI? When does it occur?
|
arrhythmia
occurs in first 4 days |
|
|
Inferior MI is associated with what type of heart blocks?
Anterior MI is associated with what type of heart blocks? |
inferior MI: first degree AV block, Wenkebach second degree AV block
Anterior MI: Mobitz second degree AV block |
|
|
What EKG finding indicates reperfusion after acute MI?
|
Automatic intraventricular rhythm (AIVR)
|
|
|
How does acute mitral insufficiency occur after acute MI?
Where is the MI in this scenario? |
due to rupture of posteromedial papillary muscle
Usually occurs with inferior MI due to insufficient RCA. |
|
|
List complications of acute MI that occur 4-7 days the event.
|
1. Left ventricular rupture --> cardiac temponade --> death
2. septal rupture (holocystic murmur heard) 3. papillary muscle rupture --> mitral insufficiency |
|
|
Right ventricular infarct is most commonly associated with abnormal EKG findings in what leads?
|
Associated with inferior MI (leads II, III, avF)
|
|
|
What is Kussmaul's sign?
What type of infarction is this sign most commonly associated with? |
Kussmaul's sign shows an increase in JVP with inspiration and pulsus paradoxus (decreased BP with inspiration and increased BP with expiration)
associated with right ventricular infarction, cardiac tamponade, cardiac tumor |
|
|
60 YO male presents with malaise, fever, and pain. He had an acute MI 5 weeks ago. The lab shows elevated ESR. Physical shows frictional rubbing sound. What syndrome is most likely?
|
Dressler's syndrome: immune-mediated pericarditis post-MI.
|
|
|
What drug is contraindicated in a pt suffering from acute MI with:
1. heart blocks 2. hypotension 3. in any acute MI |
1. beta blockers
2. ACE inhibitor 3. Ca channel blockers |
|
|
When does a ventricular aneurysm develop post-MI?
Where is the most common site? What other complications are associated with ventricular aneurysm? |
occurs weeks to months post-MI.
Complications of ventricular MI include: 1. mural thrombus formation 2. lower Ejection fraction 3. heart failure may follow |
|
|
List 7 symptoms of rheumatic fever.
|
"FEVERSS"
Fever Erythema marginatum Valvular damage (most common cause of mitral stenosis) increased ERS Red hot joint (polyarthritis) SubQ nodules St vitus dance (chorea) |
|
|
What infection occurs prior to Rheumatic fever? What is the causative organism?
|
Pharyngitis due to group A strep pyogene
|
|
|
What is the most commonly affected age group in rhematic fever?
|
age 5-15
|
|
|
Describe the pathogenesis of Rhematic fever.
|
Abs are generated from M proteins of Group A pyogene --> hypersensitivity II and IV against sarcomere, smooth muscule, valves, fibroblasts and other connective tissue disorder.
|
|
|
What are Aschoff bodies? What phase of the disease are they seen?
|
Aschoff bodies are central area of fibrinoid necrosis surrounded by Anitschkow cells (reactive histocytes)
seen in cellular phase of rheumatic fever |
|
|
List 2 most common valves associated Rheumatic fever.
What type of pericarditis is produced by RF? |
Mitral valve (most common) and aortic valve
fibrinous inflammation "Bread and butter" pericarditis |
|
|
What are 2 long-term complications of rheumatic fever?
|
mitral valve stenosis --> Left atrium enlargement
thrombus formation |
|
|
What is the most common cause of aortic stenosis in adults?
What is the prognosis of aortic stenosis? What is the critical diameter aortic opening to produce severe symptoms? |
Calcification
poor prognosis: medial survival of 2-3 yrs critical level of stenosis below 0.5cm2 |
|
|
What complications are associated with aortic stenosis?
|
gradual stenosis --> concentric LV hypertrophy
sudden stenosis --> Acute LV dilatation and decreased SV |
|
|
A 30 YO female presents with dyspnea and fatigue. During physical, a midsystolic click and systolic murmur is heard. What do you suspect?
How can you move the "click" closer to S1? closer to S2? |
suspect mitral valve prolapse
Increase the preload (e.g. squat or sustained hand grip) --> closer to S2 decreased the preload (e.g. valsava) --> closer to S1 |
|
|
Mitral valve prolapse is associated with what 2 genetic disorders?
|
Marfan's syndrome (defect in Fibrilin 1)
Ehler-Danlos syndrome (defective collagen) |
|
|
What are complications of mitral valve proplase? (4)
|
1. infective endocartitis
2. mitral insufficiency/regurgitation 3. atrial and ventricular arrhthmias 4. sudden death secondary to ventricular fib (very rare) |
|
|
What are symptoms of infective endocarditis?
|
"FROM JANE"
Fever Ruth's spots: irregular red area with central white dot on retina Osler's nodes: painful nodules on pads of fingers or toes Murmur Janeway's lesion: painless lesions on palms and feet Anemia Nailbed hemorrhage Emboli (septic) |
|
|
What is the most common causative organism in acute infective endocarditis? subacute endocarditis? after insertion of prosthetic valve? IE associated with ulcerative colitis or colorectal cancer?
Which valve is most commonly affected? Which valve is most commonly affected in IV drug abusers? |
acute: staph aureus
subacute: Strep viridan prosthetic valve: staph epidermidis UC or colorectal cancer: strep bovis mitral valve is most commonly affected triscupid valve is most commonly affected in IVDA |
|
|
A pt diagnosed with mucin producing colon tumor gets ultrasound. It reveals vegetation on mitral valve. What do you suspect?
|
marantic endocaritis (nonbacterial thrombotic endocarditis)
|
|
|
Libman Sacks endocarditis is associated with what disorder?
|
systemic lupus erythematosus
|
|
|
what 2 ddx are suspected with fibrosis of triscupid valve and pulmonary valve?
|
infective endocarditis in IVDA
Carcinoid heart disease |
|
|
What is the most common cause of mitral regurgitation?
|
mitral valve prolapse
|
|
|
What is Barlow's syndrome?
What histological feature is seen in the affected tissue? |
Barlow syndrome is associated with mitral valve prolapse.
myxomatous degeneration of mitral leaflets: pathological weakening of connective tissue |
|
|
What physical law explains compensatory ventricular hypertrophy due to increased wall stress?
|
law of LaPlace
|
|
|
What is the most common risk factor of mitral anular calcification?
|
renal failure
|
|
|
Differentiate b/t acute and chronic mitral regurgitation
|
Acute: normal LA, normal heart size, decreasing gradient, S4, profound symptoms, sinus rhythm, elevated Pul artery pressure
chronic: enlarged LA and heart, holocytic murmur, soft S1, indolent symptom, atrial fibrillation, normal PA until LV dysfxn, S3 |
|
|
what is the most common symptom of mitral stenosis?
What is the hemodynamic hallmark of mitral stenosis? |
dyspnea
reduced response of cardiac output to exercise |
|
|
A pt presents with dyspnea, fatigue, hoarsness. Physical reveals RV lift, P2 sound. Echo reveals diastolic leaflet doming.
What type of valvular disease is this? |
mitral stenosis.
|
|
|
What is the most common cause of aortic stenosis in children?
|
congenital bicuspid aortic valve
|
|
|
Describe how aortic stenosis leads to pulmonary hypertension.
|
aortic stenosis --> increased LVEDP (end-diastolic pressure) --> high pressure transmitted to pulmonary system --> pulm HTN
|
|
|
what is the overall prognosis of aortic stenosis?
List a poor prognosis factor. List 2 "better" prognosis factors. |
overall poor (median 2-3 yr survival)
poor: heart failure (2 yr 50% survival) better: syncope (3 yr 50% survival) better: angina (5 yr 50% survival) |
|
|
What type of murmur is heard in aortic stenosis?
How can you increase the intensity of the murmur? decrease? |
diamond shaped systolic murmur
Increase preload --> increase intensity decrease preload --> decrease preload |
|
|
What type of hypertrophy occurs in aortic stenosis? aortic regurgitation?
|
aortic regurgitation --> eccentric (dilated) hypertrophy
aortic stenosis --> concentric hypertrophy |
|
|
What is a typical BP in aortic regurgitation?
What auscultory sounds are heard in aortic regurgitation? |
decreased diastolic pressure and increased systolic pressure (widened pulse pressure; e.g. 150/60)
S3 is heard Long decrescendo diastolic murmur is heard |
|
|
What is Austin Flint murmur? What condition is associated with it?
|
aortic regurgitation jet vibrating the anterior leaflet of the mitral valve --> causes functional mitral stenosis
|
|
|
What is the surgical indication of valve replacement in aortic regurgitation?
Is it only for symptomatic pts? |
when Austin Flint murmur is heard.
indicated in both symptomatic and asymptomatic pts. |
|
|
Endocardial cushion forms what parts of the heart? (3)
|
upper part of ventricular septum
lower part of atrial septum AV valves |
|
|
What embryological structure develops into great vessels?
|
Left arches
Right arches atrophy |
|
|
In which direction does the heart loop developmentally? what is the condition called if the direction is reversed?
|
to the right (dextro-looping)
situs inversus (left or levo-looping) |
|
|
Which vessels has the highest SaO2 in fetal circulation?
What keeps the ductus arteriosus open? |
umbilical vein
PGE2 |
|
|
what keeps pulmonary resistance high before birth? (3)
What lowers the resistance after birth? (2) |
increased resistance is due to:
1. coiling of pulmonary arterioles 2. pulmonary vasoconstriction 3. increased smooth muscle mass in the pulmonary arterioles after birth: 1. replacement of alveolar fluid by air 2. vasodilation of pulmonary arterioles by increased alveolar oxygen tension and bradykinin stimulation |
|
|
Name 3 congenital heart diseases associated with left-to-right shunt.
Which one is most common? What happens to the Sao2 in the heart chambers in each condition? |
ventricular septum defect (VSD): most common, Sao2 step up in the RV and pulmonary artery
Atrial septum defect (ASD): SaO2 step up in RA, RV, and PA patent ductus arteriosus (PDA): SaO2 step up in pulmonary artery |
|
|
What is Eisenmenger's syndrome?
|
Uncorrected VSD, ASD, and PDA causes compensatory RV hypertrophy --> causes right-to-left shunt --> cyanosis
|
|
|
In what congenital heart defect, do you observe machinary murmur?
|
patent ductus arteriosus (PDA)
|
|
|
What is Williams syndrome?
|
congenital suprvalvular aortic stenosis
|
|
|
discuss two types of coarctation of aorta.
|
infantile: coarctation proximal to ductus arteriosus
adult: coarctation distal to ductus arteriosus |
|
|
A 10 YO boy shows up with asymmetrical radial pulse, which is slightly increased. A bruit is heard in the left side of chest. What do you do next?
What do you suspect? |
feel for femoral pulse.
If no femoral pulse, suspect coarctation of aorta |
|
|
What complications are associated with adult aortic coarctation?
What do you find on Chest X ray? |
decreased blood pressure on lower extremity -->
1. leg claudication 2. decreased renal flow --> activation of RAA system --> HTN |
|
|
Compare and contrast central cyanosis and acrycyanosis.
|
Central cyatnosis: lips and core; often due to circulatory or ventilator problem
Acrycyanosis: peripheral; can be observed without heart or lung problems |
|
|
How do you calculate cardiac output using Fick's principle?
|
CO or blood flow = oxygen delivery (VO2)/ (Arterial O2 sat - venous O2 sat)
|
|
|
Describe the hyperoxia challenge test.
|
It is helpful distinguishing from R--> L shunt from other causes of hypoxemia
steps 1. administer FiO2 100% O2 2. in R --> L shunt, will NOT correct 3. in V/Qmismatch, alveolar hypoxia, and diffusion impairment, will correct. |
|
|
Name 5 cyanotic congenital heart diseases.
which one is most common? |
Tetralogy of Fallot (most common)
Transdisposition of the great vessels Truncus arteriosus Tricuspid atresia Total anomalous pulmonary venous return |
|
|
Name 4 defects in tetralogy of Fallot.
Where does a change in SaO2 occur? (where in the heart?) |
"PROVe"
Pulmonary stenosis RV hypertrophy Overriding Aorta Ventricular septal defect Step down (decreased SaO2) in LV and aorta |
|
|
What is Tet spell? How do you improve the condition?
|
Tet spell is a sudden episode of increased hypoxemia and cyanosis.
Increased by squatting --> increased afterload --> more Left-to-right shunting --> more blood is oxygenated |
|
|
What are the defects in transposition of great vessels?
What protective defects are necessary for survival? |
Aorta from RV and pulmonary artery from LV
VSD, ASD, and/or PDA are needed to sustain life. |
|
|
What is the defect in truncus arteriosus?
What happens to the Sao2 in RV and LV? |
aorta and pulmonary artery share common trunk
step down in LV and step up in RV |
|
|
What structural change is noted in all types of cardiomyopathy (CM)?
Which type has systolic dysfunction? diastolic dysfunction? Which one is most common? least common? |
All CM have dilated Left atrium
Dilated CM: most common; systolic dysfunction Hypertrophic CM: diastolic dysfunction restrictive CM: least common; diastolic dysfunction |
|
|
List etiologies of dilated cardiomyopathy.
Most common? 2nd most common? 3rd most common? |
"ABCD...."
A Beriberi (wet, thiamine deficiency): 3rd most common Chaga's disease, Coxsackie virus, cocaine Drugs: doxirubicin, anthracyclines Genetic defect: second most common Idiopathic: most common |
|
|
A 45 YO male with alcohol problems complain of SOB, dyspnea on exertion, and cough. Physical exam reveals S3, S4, narrow pulse pressure. Echo reveal 35% ejection fraction. What do you suspect?
|
dilated cardiomyopathy.
|
|
|
What is the most common cause of death in young, athletic individuals?
|
hypertrophic cardiomyopathy
|
|
|
Which wall of the heart is significantly enlarged in hypertrophic cardiomyopathy?
What microscopic pathological hallmark do you find in HCM? What is the clinical significance of it? |
subaortic interventricular septum
disarray of myofibers --> fatal arrhythmia |
|
|
What are 3 common causes of restrictive myocardiopathy?
|
amyloidosis
radiation fibrosis fibrosis after open-heart surgery |
|
|
What do Davies disease, Loffler's endomyocarditis, and endocarial fibroelastosis have in common?
|
they are all restrictive cardiomyopathy.
|
|
|
List 3 common infectious agents that cause myocarditis. Which one is most common?
|
Coxsackie virus: most common
Chaga's disease (Trypanosoma cruzi) Lyme disease (Borrelia burgdorferi) |
|
|
What type of inflammatory cells are predominant in viral myocarditis under light microscopy?
|
mononuclear cells
|
|
|
You suspect myocarditis and a endocardial biopsy. Histology shows mixed inflammatory cells, multinucleated cells and extensive necrosis.
What type of myocarditis do you suspect? |
giant cell myocarditis
|
|
|
List 2 most common indications for cardiac transplant.
What are 2 common complications associated with the transplant? |
dilated cardiomyopathy
ischemic heart disease complications: allograft rejection, diffuse stenosing intimal proliferation of the intramural arteries |
|
|
What is the #1 known cause of the pericarditis?
|
Coxsackie virus
#1 overall cause is idiopathic |
|
|
List 6 types of acute pericarditis.
which one is most common? Dressler's syndrome is associated with which type of pericarditis? |
1. serous
2. fibrinous: most common; associated with Dressler's syndrome (post-MI autoimmune pericarditis) 3. purulent 4. caseous 5. hemorrhagic 6. chylous |
|
|
What is the most common cause of caseous pericarditis?
|
Mycobacterium tuberculosis
|
|
|
What is soldier's plaque?
|
Focal, chronic/healed, epicardial plaque on pericardium.
|
|
|
List 2 complications of pericarditis.
|
constrictive pericarditis: impaire diastolic filing, decrease SV and cardiac output
adhesive mediastinopericarditis (adhesion b/t pericardial layers and surrounding mediastinal structures) --> the heart contracts against all the surrounding structures --> hypertrophy and dilation |
|
|
What kind of inheritance pattern does the familial form of hypertrophic cardiomyopathy have?
where is the mutation? |
autosomal dominant
mutation of myosin heavy chain on chromosome 14. |
|
|
What is the pathogenesis of the murmur in hypertrophic cardiomyopathy?
How do you increase the murmur? decrease? |
hypertrophy of septum --> creates pressure gradient b/t LV and aorta (higher in LV) --> sucks the anteior leaflet of the mitral valve toward the wall --> mitral regurgitation during systole --> systole murmur
Increase murmur: decrease preload (e.g. valsalva maneuever, standing) decrease murmur: increase afterload or preload (squatting, sustained-hand grip) |
|
|
What is the most likely mechanism of syncope and sudden death in hypertrophic cardiomyopathy?
|
sustained ventricular tachycardia and fibrillation due to disarrayed myofibers
|
|
|
What is the first line of drug therapy in hypertrophic cardiomyopathy? adjunct drug?
|
large dose of beta blockers
Ca channel blockers are adjunct |
|
|
What kind of inheritance pattern does dilated cardiomyopathy follow? (genetic cause)
What protein is defective, most commonly? |
autosomal dominant
defective beta-myosin heavy chain |
|
|
A 27 YO female presents with signs of congestive heart failure (SOB, dyspnea on exertion, cough, orthopnea). She delivered a baby 4 weeks ago. What do you suspect?
|
dilated cardiomyopathy
|
|
|
How are the staging system and NYHA functional classification system different in categorizaing heart failure?
|
staging system: don't go back in stage
NYHA: can move up and down the class; degree of LV dysfunction does not correlate) |
|
|
What is the gold stand for heart failure diagnosis?
|
2D echocardiogram and doppler
|
|
|
What serum marker is used as a confimatory tool for dx of LV dysnfunction?
|
brain natriuretic peptide (BNP): seceted with dilatation of LV
|
|
|
Compare and contrast concentric and eccentric hypertrophy.
|
Concentric: myofibers added in parellel; due to pressure overload (e.g. high afterload); thickens
eccentric: myofibers added in series; due to volume overload (e.g high afterload); lengh of the muscle is increased |
|
|
compare and contrast systolic heart failure from diastolic heart failure.
|
Systolic: low EF; most commonly due to CAD (decreased ventricular contraction)
diastolic: high EF; due to HTN, concentric hypertrophy, and aortic stenosis (noncompliant ventricle --> restrictive filling) |
|
|
What is the recommended tx for abnormal preload in heart failure? afterload?
|
Reduce volume in preload: loop diuretics, Na restriction
reduce systemic resistance in afterload: ACEI, ARB, nitrate, hydralazine |
|
|
what heart failure drugs are not known to improve survival rate of patients? (3)
|
Diuretics, digoxins, IV ionotropes
|
|
|
What is the most common cause of right-sided heart failure?
|
left sided heart failure
|
|
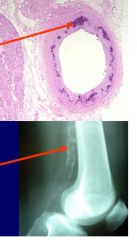
What type of arteriosclerosis is this? Does it lead to ischemia of the affected region?
|
Monkenberg arteriosclerosis: calcification of the media
Does not narrow the lumen --> no ischemia |
|
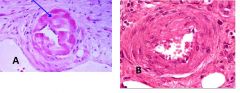
The folloiwng pictures show arteriolosclerosis. What type of arteriolosclerosis is this?
What 2 disorders are associated with picture "A"? |
A: hyaline arteriolosclerosis; associated diabetes and hypertension
B: hyperplastic arteriolosclerosis; associated with malignant HTN |
|
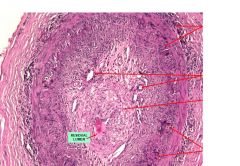
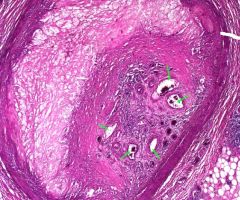
A 60 YO male presents with throbbing pain on the temporal area and jaw claudcation. Temporal artery is biopsied and shown in the picture.
1. what is the dx? 2. What symptom indicates medical emergency? 3. what are bottom 2 arrows pointing at? |
1. temporal (giant cell) arteritis
2. sudden vision loss 3. multinucleated giant cells |
|
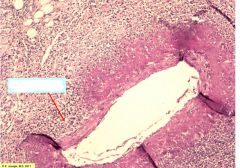
The following picture is a biopsy from a pt diagnosed with polyarteritis nodosa.
1. What does the arrow indicate? 2. What type of immune complexes are associated with PAN? |
1. a small area of the vessel that does not show fibrinoid necrosis
2. HepB surface antigen-ab complex |
|
|
Compare and contrast stable plaque with vulnerable plaque.
|
Stable plaque: thick fibrous cap, thick smooth muscle cell layer, small lipid core, less prone to rupture
vulnerable plaque: thin fibrous cap, thin SMC layer, large lipid core, more prone to rupture, and macrophages interact with thrombus |
|
This is a section of occluded coronary artery. What do small, green arrows indicate?
|
recanalization
|
|
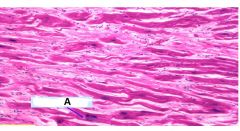
This is a biopsy of heart muscle. what does this indicate? What is A?
|
myocardial hypertrophy
A: enlarged (Box-shaped) nucleus |
|
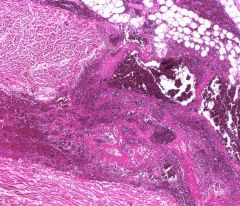
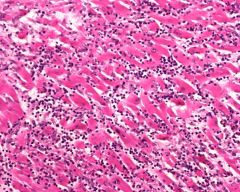
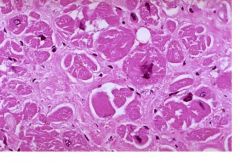
This picture depicts tranmural infarction of the heart. What type of leukocytes are present? What type of necrosis is going on?
|
PMNs (neutrophils)
Coagulative necrosis |
|
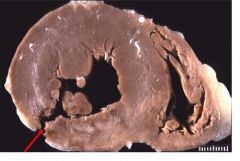
This is a picture of heart. What does the arrow indicate? In how many days, does this event occur following the initial event?
|
The arrow indicates ruptured ventricular wall.
Occurs 3-7 days post-MI. |
|
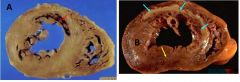
Pictures A and B indicate post-MI heart. Which one would show ST-depression on EKG when the heart is undergoing MI? ST-Elevation?
|
A: ST depression (subendocardial infarction)
B: ST elevation (transmural infarction) |
|
|
List 2 microscopic findings within 1-4 hours of onset of MI.
|
myocardial Cell swelling
wavy myofibers |
|
|
Within how many hours after the onset of MI do you expect neutrophils to show up?
|
12-24 hours
|
|
|
When is the heart most prone to rupture after experiencing MI?
|
3-7 days after MI
|
|
|
When do you well-established granulation tissues settle after experiencing MI? How about collagenous scar tissue?
|
granulation tissues show in 10-14 days
scar tissues appear after 2 months. |
|
|
When can ventricular aneurysm form after experiencing MI? What are complications of ventricular aneurysm?
|
Ventricular aneurysm is a late complication that forms after 2 months of having MI.
Complications of the aneurysm include CHF, mural thrombosis, arrhythmia |
|

In this pic, is the MI ongoing or healed? How do you know?
|
It's healed. The white tissue represent fibrous scar tissue. And there is no hyperemia around the white tissue, which indicate the MI is healed.
|
|
Is this viral myocarditis or an ongoing MI?
How do you know? |
viral myocarditis
There are infiltrates of MNCs with a few plasma cells and eosinophils |
|

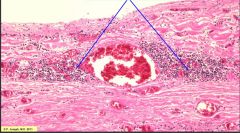
What are indicated by the arrows? What type of cells are within the structures?
|
Aschoff bodies (in rhematic endocarditis)
Anischtkow cells (enlarged macrophages) |
|
|
What is the most common cause of mitral stenosis?
|
rhematic fever
|
|
|
List 3 gross findings of rheumatic valvulitis.
|
1. thickened chordae tendinae
2. thickended mitral valve 3. LV hypertrophy |
|

You heard "friction rub" upon ausculation and the autopsy shows above picture?
What type of pericarditis is this? What is a common syndrome associated with this type of pericarditis? |
fibrinous pericarditis. Commonly associated with the Dressler's syndrome (post-MI autoimmune attack of the pericardium)
|
|
This section of aorta is taken from a pt diagnosed with syphilitic aneurysm. The arrows are pointing at the inflammatory cells around the blood vessels.
1. What is the name of the vessels? 2. What inflammatory cells are present? 3. What is this process called? |
1. vasa vasorum
2. plasma cells and lymphocytes 3. obliterative endarteritis or plasmacystic vasculitis |
|
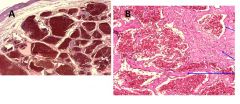
What type of vascular tumor is A? B?
|
A: capillary hemangioma
B: cavernous hemagioma |
|
|
What is the most common primary cardiac neoplasm?
List 2 complications |
atrial myxoma
complications: syncope (by blocking mitral orifice) and embolization |
|
|
What are histopathological findings of dilated cardiomyopathy?
|
Mostly same as normal myocardium but might see some fibrosis
|
|
|
Which hole is most commonly defective in ventricular septal defect? atrial septal defect?
|
VSD: membranous portion of IV septum
ASD: septum secudum |
|
This is a biopsy of myocardium. What do you suspect?
|
Hypertrophic cardiomyopathy. disarray of myofibers
|
|
|
What is a paradoxical embolus? when do you see this?
|
A paradoxical embolus is an venous embolus that ends up in the systemic circuit.
This is seen with a rise in right atrial pressure (usually due to pulmonary hypertension), and this can open foramen ovale. Foramen ovale acts like a one-way valve; it is closed when the left pressure is higher than the right pressure. However, when the right pressure become higher, the foramen ovale could open and allow venous embolus to enter systemic circuit. |
|
|
A 3 YO boy presents with chest pain and dyspnea. All the physical exams point to having an MI. What do you suspect?
|
Kawasaki vaculitis: one of its complications is coronary artery aneurysm --> MI
|

